Chapter 63 with our Microbiology MCQs and explanations! Test your knowledge and understanding of key concepts with our complete set of multiple choice questions with detailed explanations for each answer. Increase your confidence and understanding of the fascinating world of microorganisms!
Microbiology is the study of living organisms that are not visible to the naked eye. All microorganisms such as amoebae, protozoa, viruses, bacteria are studied in microbiology. Microbes play a major role in nutrient cycling, decomposition, food spoilage, disease control and causation, and biotechnology. Due to their versatile nature, they can be used for different purposes.
Below is a set of microbiology MCQs along with the answers for your reference. These will help students improve their conceptual knowledge.
Microbiology MCQs 3101 to 3150
- Urea is decomposed by the species?
- Micrococcus sps.
- Nitrosomonas sps.
- Proteus sps.
- Both Micrococcus sps. and Proteus sps.
Answer and Explanation
Answer: Both Micrococcus sps. and Proteus sps.
Urea is a nitrogen-containing waste product found in urine. Several bacterial species are capable of decomposing urea, including both Micrococcus and Proteus. This decomposition process breaks down urea into ammonia and carbon dioxide.
The other options are incorrect:
- Nitrosomonas sps.: While this species plays a role in the nitrogen cycle, it specifically oxidizes ammonia into nitrite, not decomposing urea directly.
- Parasitic form must contain?
- Capsules
- Cell-wall
- Endospores
- Flagella
Answer and Explanation
Answer: Cell-wall
A cell wall is a rigid outer layer that provides structural support and protection for most parasites. It helps them maintain their shape and resist the harsh environments they may encounter within their host.
The other options are incorrect:
- Capsules: While some parasites can produce capsules, it’s not a defining characteristic. Capsules are often temporary structures for specific purposes, not essential for all parasites.
- Endospores: Endospores are dormant structures formed by some bacteria, not a typical feature of parasitic organisms. Endospores allow bacteria to survive harsh conditions, not a requirement for most parasites.
- Flagella: Flagella are hair-like structures for movement, found in some parasites but not all. Many parasites rely on other means of locomotion or remain stationary within their host.
- Transformation was observed mainly in?
- Bacteriophages
- Temperate phages
- ? –phage
- All of these
Answer and Explanation
Answer: Temperate phages
Transformation, the process of a bacterium taking up foreign genetic material from its environment and incorporating it into its own genome, is primarily observed in temperate phages. These phages have the ability to integrate their DNA into the host bacterium’s genome during the lysogenic cycle, facilitating the transfer of new genetic material and leading to genetic transformation.
The other options are incorrect:
- Bacteriophages: This is a broad term encompassing both temperate and virulent phages. While transformation can occur in some virulent phages under specific circumstances, it’s not the main way it’s observed.
- λ (Lambda) -phage: This is an example of a temperate phage commonly used in research to study transformation. However, the question asks for the main type where transformation is observed, not a specific phage.
- All of these: As explained above, transformation is not as prevalent in virulent phages as it is in temperate phages.
- Capsulated forms of bacteria are?
- Virulent
- A virulent
- Useful
- Symbiotic
Answer and Explanation
Answer: Virulent
Capsulated forms of bacteria are often virulent. Capsules are protective structures surrounding bacterial cells that enhance their ability to cause disease by helping them evade the host’s immune system. Capsules can prevent phagocytosis and enhance bacterial survival within the host, contributing to their virulence.
The other options are incorrect:
- A virulent: This option appears to be a typographical error and does not provide a coherent choice.
- Useful: While some bacteria with capsules can be beneficial and have specific functions in certain contexts (e.g., probiotics), the presence of capsules typically enhances the bacteria’s pathogenicity rather than usefulness in symbiotic or other beneficial relationships.
- Symbiotic: Capsulated forms of bacteria are more commonly associated with pathogenicity rather than symbiosis. While some symbiotic bacteria may possess capsules, it’s not a defining characteristic of symbiotic relationships between bacteria and hosts.
- The bacterial cells participating in conjugation are?
- Conjugants
- Fertile cells
- Exconjugants
- None of these
Answer and Explanation
Answer: Conjugants
The bacterial cells participating in conjugation are called conjugants. Conjugation is a process of genetic transfer between bacterial cells that involves direct physical contact and exchange of genetic material, typically in the form of plasmids, through a conjugation bridge or pilus.
The other options are incorrect:
- Fertile cells: Fertility can refer to the ability to participate in conjugation. However, not all fertile cells are actively engaged in conjugation at a given time. “Conjugants” specifically refers to the bacteria involved in the current conjugation event.
- Exconjugants: These are the cells that have already undergone conjugation and separated. They may now possess the transferred genetic material. “Conjugants” refers to the bacteria during the act of conjugation, not after.
- The coating of a bacterium with antibody or complement that leads to enhanced phagocytosis of the bacterium by phagocytes is called?
- Opsonisation
- Aggulation
- CFT
- None of these
Answer and Explanation
Answer: Opsonisation
Opsonisation is a crucial process in the immune system where particles, like bacteria, are tagged for destruction by phagocytes (white blood cells). Opsonins, such as antibodies and complement proteins, coat the surface of the bacteria. Phagocytes have receptors that specifically recognize these opsonins, allowing them to effectively engulf and eliminate the bacteria.
The other options are incorrect:
- Agglutination: This refers to the clumping together of bacteria due to antibodies binding to specific antigens on their surface. While it can enhance immune recognition, it doesn’t directly trigger phagocytosis like opsonisation.
- CFT (Complement Fixation Test): This is a laboratory test that detects the presence and activity of the complement system in the blood. While the complement system plays a role in opsonisation, CFT itself is not the process of coating bacteria for phagocytosis.
- Infection that results in pus formation are called?
- Focal infection
- Acute infection
- Pyogenic infection
- Chronic infection
Answer and Explanation
Answer: Pyogenic infection
A pyogenic infection is an infection caused by pus-forming bacteria. These bacteria, often staphylococci or streptococci, trigger an inflammatory response in the body. As white blood cells fight the infection, they die and accumulate along with dead tissue and bacteria, forming pus.
The other options are incorrect:
- Focal infection: This refers to a localized infection confined to a specific tissue or organ. While pus formation can occur in focal infections, it’s not the defining characteristic. Other types of infections can also be focal.
- Acute infection: This describes an infection with a rapid onset and short duration. Pus formation can happen in both acute and chronic infections.
- Chronic infection: This is a long-term infection that persists for weeks, months, or even years. Pus formation can be a feature of chronic infections as well, but it’s not exclusive to them.
- Presence of viable bacteria in the blood stream is called?
- Viraemia
- Septicaemia
- Bacteraemia
- Bactericidal
Answer and Explanation
Answer: Bacteraemia
Bacteraemia refers to the presence of viable (living and reproducing) bacteria in the bloodstream. This can be a serious condition as bacteria can spread throughout the body and cause widespread infection.
The other options are incorrect:
- Viraemia: This term refers to the presence of viruses in the bloodstream, not bacteria.
- Septicaemia: Septicemia is a more severe form of bacteraemia. It’s characterized by the presence of bacteria in the bloodstream along with a systemic inflammatory response (sepsis). Sepsis can lead to organ damage and even death.
- Bactericidal: This term describes something that kills bacteria, not the presence of bacteria itself.
- ßßß-haemolytic bacteria is?
- Streptococcus pyogenes
- Str. pneumoniae
- Str. viridans
- Str. faecalis
Answer and Explanation
Answer: Streptococcus pyogenes
ß-haemolytic bacteria refers to bacteria that produce complete haemolysis on blood agar, resulting in a clear zone around the colonies. Streptococcus pyogenes, also known as Group A Streptococcus, is one such bacterium. It is known to cause a variety of infections, including strep throat, skin infections, and more severe conditions like necrotizing fasciitis and toxic shock syndrome.
The other options are incorrect:
- Str. pneumoniae: This bacterium is typically alpha-hemolytic, meaning it causes a partial greening of red blood cells on agar plates.
- Str. viridans: Similar to Str. pneumoniae, this species is also commonly alpha-hemolytic.
- Str. faecalis: This bacterium is usually non-hemolytic, meaning it doesn’t cause any lysis of red blood cells on blood agar plates.
- The natural reservoir of infection for cholera is?
- Flies
- Horse
- Man
- None of these
Answer and Explanation
Answer: Man
Humans are the primary reservoir for cholera, an infectious disease caused by the bacterium Vibrio cholerae. Infected individuals shed the bacteria in their feces, which can contaminate water sources. When others consume contaminated water, they can become infected, perpetuating the cycle.
The other options are incorrect:
- Flies: While flies can transmit various diseases mechanically by carrying pathogens on their bodies, they are not a natural reservoir for cholera.
- Horse: Horses are not susceptible to cholera and wouldn’t be a natural reservoir for the bacteria that infects humans.
- Vibrio cholera differs from vibrio eltor by?
- It shares some Inaba, Ogawa subtypes with eltor
- Resistant to polymuxin
- Eltor is non-motile
- Causes less subclinical infections as compared to eltor
Answer and Explanation
Answer: Causes less subclinical infections as compared to eltor
Vibrio cholerae O1 biotype El Tor (often referred to as El Tor) causes more subclinical infections compared to Vibrio cholerae O1 classical biotype (often referred to as classical cholera). Subclinical infections are those in which individuals are infected with the bacterium but do not exhibit clinical symptoms of the disease. El Tor strain is associated with milder symptoms and higher rates of subclinical infections, contributing to its spread.
The other options are incorrect:
- Shares some Inaba, Ogawa subtypes with eltor: This is true for both biotypes.
- Resistant to polymuxin: Neither are typically resistant.
- Eltor is non-motile: Both are motile.
- Prophylaxis of cholera is?
- Protected water supply
- Environmental sanitation
- Immunisation with killed vaccines
- All of these
Answer and Explanation
Answer: All of these
Cholera is a serious diarrheal illness caused by the bacterium Vibrio cholerae. A multi-pronged approach is crucial for effective cholera prophylaxis (prevention). Here’s how each option contributes:
- Protected water supply: Contaminated water is the primary source of cholera transmission. Ensuring access to clean, safe drinking water significantly reduces the risk of infection.
- Environmental sanitation: Proper sewage disposal and sanitation practices prevent the spread of V. cholerae in the environment. This minimizes the contamination of water sources.
- Immunisation with killed vaccines: Cholera vaccines offer some protection against the disease. While not foolproof, they can reduce the severity of symptoms and prevent severe illness.
- Acid fast bacteria are?
- Neisseria
- Staphylococci
- Mycobacteria
- All of the above
Answer and Explanation
Answer: Mycobacteria
Acid-fast bacteria are a specific group of bacteria characterized by their cell wall’s unique composition. This cell wall makes them resistant to decolorization during certain staining techniques. Mycobacteria, such as Mycobacterium tuberculosis (causing tuberculosis) and Mycobacterium leprae (causing leprosy), are well-known examples of acid-fast bacteria.
The other options are incorrect:
- Neisseria: These are Gram-negative bacteria, not classified as acid-fast. They are commonly associated with various infections, including meningitis and gonorrhea.
- Staphylococci: These are also Gram-positive bacteria and not considered acid-fast. Staphylococcus aureus is a common example, known for causing various skin infections and foodborne illnesses.
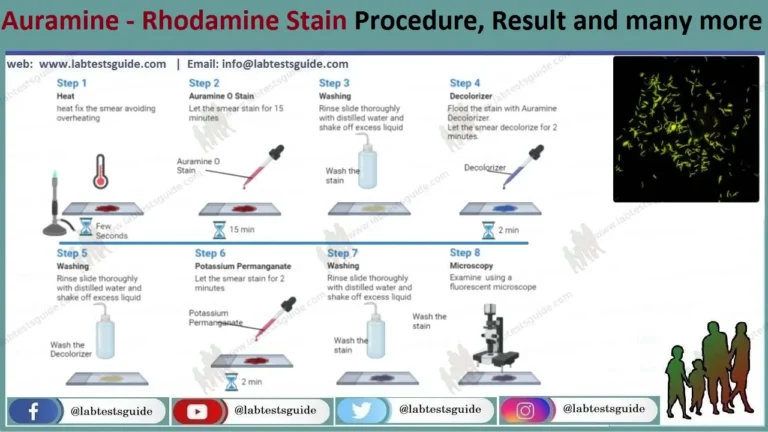
- Mycobacteria are stained with?
- Gram’s staining
- Simple staining
- Both Gram’s staining and Simple staining
- Ziehl – Neelsen’s staining
Answer and Explanation
Answer: Ziehl – Neelsen’s staining
Mycobacteria are stained using Ziehl – Neelsen’s staining, a specific technique designed to identify acid-fast bacteria. This technique utilizes a combination of dyes and heat to overcome the resistance of the mycobacterial cell wall.
Incorrect Options:
- Gram’s staining: This is a widely used staining method that differentiates bacteria based on their cell wall composition into Gram-positive and Gram-negative categories. Mycobacteria wouldn’t be readily identifiable using Gram’s stain due to their unique cell wall structure.
- Simple staining: Simple staining involves applying a single dye to visualize bacteria under a microscope. While it can provide basic information about bacterial morphology, it doesn’t offer the specific identification capabilities required for acid-fast bacteria.
- Both a and b: As explained above, neither Gram’s staining nor simple staining are ideal for identifying Mycobacteria.
- Niacin test is positive in case of?
- Corynebacterium
- M. tuberculosis
- M. bovis
- M. avium
Answer and Explanation
Answer: M. tuberculosis
The niacin test is a biochemical test used to differentiate Mycobacterium tuberculosis from other mycobacterial species. In the niacin test, M. tuberculosis produces niacin (nicotinic acid) from niacinamide (nicotinamide), resulting in a positive test indicated by a yellow to orange color change. Other mycobacterial species, including M. bovis and M. avium, typically do not produce niacin, resulting in a negative niacin test.
The other options are incorrect:
- Corynebacterium: The niacin test is not typically used to differentiate Corynebacterium species. Corynebacteria are not known to produce niacin, and the niacin test is not routinely performed for this bacterial genus.
- M. bovis: M. bovis is one of the mycobacterial species that typically yield a negative result in the niacin test. Unlike M. tuberculosis, M. bovis does not produce niacin from niacinamide, resulting in a negative test.
- M. avium: M. avium, like M. bovis, typically produces a negative result in the niacin test. It does not produce niacin from niacinamide, which distinguishes it from M. tuberculosis, yielding a negative test result.
- Streptococcus forms causes which type of infections?
- Fever
- Zoonotic
- Pyogenic
- None of these
Answer and Explanation
Answer: Pyogenic
Pyogenic refers to bacteria that produce pus, a characteristic feature of many Streptococcus infections. Streptococcus bacteria can infect various tissues, causing the formation of pus-filled lesions.
The other options are incorrect:
- Fever: Fever can be a symptom of a Streptococcus infection, but it’s not specific to Streptococcus and can occur with many other infections.
- Zoonotic: Zoonotic refers to diseases transmissible between animals and humans. While some Streptococcus species can cause zoonotic infections, not all Streptococcus infections are zoonotic.
- Streptococcus pyogenes classification is based on?
- Protein M
- Protein T
- Protein R
- Polysaccharide C
Answer and Explanation
Answer: Protein M
Protein M is a key surface protein on Streptococcus pyogenes that plays a crucial role in virulence (causing disease). It helps the bacteria evade the immune system and adhere to host cells. Classification of S. pyogenes is primarily based on different M protein types, with over 200 identified so far.
The other options are incorrect:
- Protein T: While proteins like Protein T might exist in Streptococcus pyogenes, they are not the primary basis for classification.
- Protein R: Similar to Protein T, Protein R might be present but isn’t the main factor for classification.
- Polysaccharide C: Polysaccharide capsules are present in some Streptococcus species, but S. pyogenes doesn’t have a polysaccharide capsule and classification relies on Protein M.
- aaa-haemolytic streptococci are also known as?
- Str. pyogenes
- Virulence group
- Viridans group
- None of these
Answer and Explanation
Answer: Viridans group
Alpha-haemolytic streptococci are also known as the viridans group. These bacteria are characterized by their ability to cause incomplete or partial haemolysis on blood agar, resulting in a greenish discoloration around the colonies. The viridans group includes various species of streptococci commonly found as part of the normal flora in the oral cavity, respiratory tract, and gastrointestinal tract.
The other options are incorrect:
- Str. pyogenes: Streptococcus pyogenes is a beta-haemolytic streptococcus, not an alpha-haemolytic one. It causes complete haemolysis on blood agar and is associated with various infections, including strep throat, skin infections, and invasive diseases such as necrotizing fasciitis and toxic shock syndrome.
- Virulence group: While streptococci can be classified based on their virulence properties, the term “virulence group” is not specifically used to refer to alpha-haemolytic streptococci. It is more commonly used in broader discussions of bacterial virulence mechanisms.
- None of these: This option is incorrect because alpha-haemolytic streptococci are indeed known as the viridans group. Choosing “None of these” would negate the established understanding of their classification.
- Streptolysin O is inactivated by?
- CO2
- Nitrogen
- Oxygen
- Serum
Answer and Explanation
Answer: Oxygen
Streptolysin O is a toxin produced by Streptococcus pyogenes. It can be reversibly inactivated by oxidation, meaning exposure to oxygen. This process disrupts the toxin’s structure and hinders its ability to damage cells.
The other options are incorrect:
- CO2 (Carbon Dioxide): While CO2 can affect some bacterial processes, it’s not known to directly inactivate Streptolysin O.
- Nitrogen: Nitrogen gas is generally not involved in inactivating bacterial toxins.
- Serum: Serum is the liquid portion of blood containing various components, including antibodies. Some components in serum can neutralize Streptolysin O, but not through direct inactivation. Antibodies in serum bind to the toxin, preventing it from attaching to and lysing (breaking down) host cells.
- Streptolysin ‘S’ is?
- Oxygen unstable
- Thermostable
- Oxygen stable
- None of these
Answer and Explanation
Answer: Oxygen stable
Streptolysin S, unlike Streptolysin O, is a toxin produced by Streptococcus pyogenes that is oxygen stable. This means exposure to air (oxygen) doesn’t inactivate it. This characteristic allows Streptolysin S to remain active and contribute to the damaging effects of Streptococcus pyogenes infections.
The other options are incorrect:
- Oxygen unstable: As mentioned above, Streptolysin S is specifically known for its stability in the presence of oxygen.
- Thermostable: While Streptolysin S might have some heat resistance, it’s not necessarily considered exceptionally thermostable. High temperatures can potentially denature (inactivate) the toxin.
- None of these: Among the given options, oxygen stability is the defining characteristic of Streptolysin S.
- Of the following, this is a capsulated organism?
- Bacillus anthracis
- Escherichia-coli
- Corynebacterium
- Brucella
Answer and Explanation
Answer: Bacillus anthracis
Bacillus anthracis is a Gram-positive, rod-shaped bacterium known for its capsule. This capsule is a polysaccharide layer surrounding the bacterial cell wall and plays a crucial role in virulence (causing disease) by protecting the bacteria from phagocytosis (engulfment by immune cells).
The other options are incorrect:
- Escherichia coli (E. coli): E. coli is a common Gram-negative bacterium that typically does not have a capsule.
- Corynebacterium: Some Corynebacterium species might possess a capsule, but it’s not a universal feature for the entire genus.
- Brucella: Similar to Corynebacterium, some Brucella species might have capsules, but it’s not a defining characteristic.
- Gasgangarene bacillus is?
- Facultative anaerobe
- Obligate anaerobe
- Facultative aerobe
- Obligate aerobe
Answer and Explanation
Answer: Obligate anaerobe
Gas gangrene is most commonly caused by bacteria of the genus Clostridium, specifically Clostridium perfringens. Clostridium species are obligate anaerobes, meaning they require an oxygen-free environment for growth and survival. They cannot tolerate oxygen and will die in its presence.
The other options are incorrect:
- Facultative anaerobe: Facultative anaerobes can grow with or without oxygen. While some bacteria associated with gas gangrene can tolerate some oxygen, true gas gangrene bacilli are obligate anaerobes.
- Facultative aerobe: Facultative aerobes prefer oxygen but can grow in anaerobic environments. This is the opposite of what gas gangrene bacilli require.
- Obligate aerobe: Obligate aerobes require oxygen for growth and will die in its absence. This is not the case for gas gangrene bacilli.
- Coagulase test is used for?
- Salmonella
- Staphylococcus
- Bordetella
- Pneumococcus
Answer and Explanation
Answer: Staphylococcus
The coagulase test is a diagnostic tool used to differentiate between various Staphylococcus species, particularly to identify Staphylococcus aureus. This test detects the presence of an enzyme called coagulase, which helps S. aureus clump together and evade the immune system.
The other options are incorrect:
- Salmonella: Salmonella is a Gram-negative bacterium and doesn’t produce coagulase.
- Bordetella: Bordetella species, like Bordetella pertussis (whooping cough), are Gram-negative bacteria and don’t produce coagulase.
- Pneumococcus: Pneumococcus, also known as Streptococcus pneumoniae, is a Gram-positive bacterium but doesn’t produce coagulase. The coagulase test is not typically used for identifying this organism.
- Those fungi which do not have a sexual stage are classified as
- Phycomycetes
- Ascomycetes
- Basidiomycetes
- Fungi imperfecti
Answer and Explanation
Answer: Fungi imperfecti
Fungi imperfecti, also known as “deuteromycetes” (though this term is no longer formally used), is a classification category for fungi that lack a known sexual reproductive stage. These fungi reproduce asexually through methods like spores or fragmentation.
The other options are incorrect:
- Phycomycetes: Phycomycetes is a phylum of fungi that can reproduce both sexually and asexually.
- Ascomycetes: Ascomycetes is another major phylum of fungi known for their sexual reproduction with the formation of spores within sacs called asci.
- Basidiomycetes: Similar to Ascomycetes, Basidiomycetes is a phylum where sexual reproduction is a defining characteristic. They produce spores on club-shaped structures called basidia.
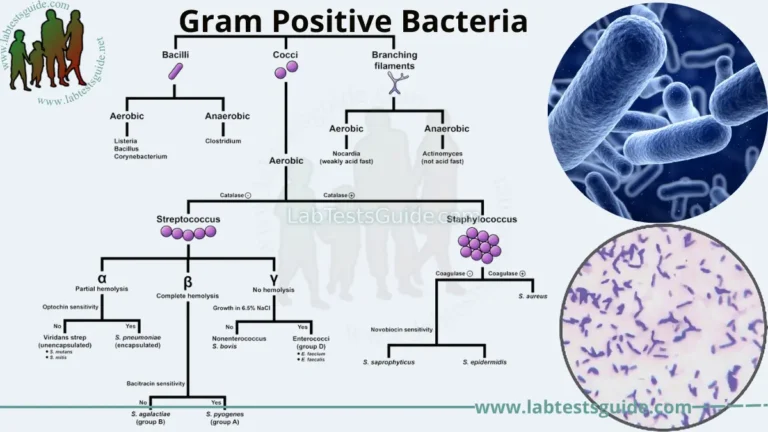
- In Gram positive bacteria, ratio of RNA to DNA is
- 8 : 1
- 1 : 2
- Almost equal
- None of these
Answer and Explanation
Answer: 8 : 1
In Gram-positive bacteria, the ratio of RNA to DNA is approximately 8:1. This means that Gram-positive bacteria typically have a higher ratio of RNA to DNA compared to Gram-negative bacteria. RNA is involved in various cellular processes, including protein synthesis, and the higher RNA content in Gram-positive bacteria reflects their robust metabolic activity.
The other options are incorrect:
- 1 : 2: This ratio is not characteristic of Gram-positive bacteria. A ratio of 1:2 would indicate more DNA than RNA, which is not typically observed in Gram-positive bacteria.
- Almost equal: Gram-positive bacteria generally have a higher ratio of RNA to DNA, as mentioned earlier. Therefore, the ratio of RNA to DNA is not “almost equal” in Gram-positive bacteria.
- None of these: This option is incorrect because the ratio of RNA to DNA in Gram-positive bacteria is indeed approximately 8:1. Choosing “None of these” would disregard the established understanding of the RNA to DNA ratio in Gram-positive bacteria.
- Ziehl – Neelson stain is a __
- Simple stain
- Counter stain
- Differential stain
- None of them
Answer and Explanation
Answer: Differential stain
The Ziehl-Neelsen stain is a specific staining technique used to identify acid-fast bacilli, a group of bacteria that resist decolorization with acid-alcohol after being stained with carbol fuchsin.
The other options are incorrect:
- Simple stain: A simple stain uses just one dye to color all cells generally. It is not specific for any particular structure within the cell.
- Counter stain: A counterstain is a second stain applied after a primary stain to provide contrast. It is used in conjunction with a primary stain, not alone. The Ziehl-Neelsen stain uses carbol fuchsin as the primary stain and methylene blue as the counterstain.
- None of them: This option is incorrect because Ziehl–Neelsen stain is indeed a differential stain. It is specifically designed to differentiate between acid-fast and non-acid-fast bacteria, making it a type of differential stain.
- Wet mount slide preparations are used in microbiology as they allow to see?
- Size and shape of individual organisms
- Characteristic arrangement or grouping of cells
- Motility of the organism
- All of these
Answer and Explanation
Answer:
Wet mount slide preparations offer a quick and simple way to observe various features of microorganisms in microbiology. Here’s why they are useful for all the listed options:
- Size and shape of individual organisms: By suspending the specimen in a drop of liquid on the slide, wet mounts allow for direct visualization of the organism’s size and overall shape under a microscope.
- Characteristic arrangement or grouping of some cells: Certain bacteria or fungi exhibit specific patterns in their growth, like chains (streptococci), clusters (staphylococci), or filaments. Wet mounts can reveal these characteristic arrangements.
- Motility of the organism: Motile organisms, like some bacteria or protozoa, can be observed moving within the liquid droplet on a wet mount slide. This can help differentiate motile from non-motile species.
- Organism resistant to degradative lysosomal enzymes includes
- M.tuberculosis
- Legionella pneumophila
- Both a and b
- Both b and c
Answer and Explanation
Answer: Both a and b
As explained previously, both M. tuberculosis and Legionella pneumophila have mechanisms to resist degradation by lysosomal enzymes within immune system phagocytes:
- M. tuberculosis: This bacterium’s waxy cell wall hinders fusion with lysosomes.
- Legionella pneumophila: This bacterium replicates within a specialized vacuole, evading lysosomal fusion.
The other options are incorrect:
- Both b and c: There is no option “c” presented in the original question.
- The main difference in true bacteria and mycoplasma is that it does not posses ?
- Flagella
- Cell wall
- ATP synthesis
- A capsule
Answer and Explanation
Answer: Cell wall
The main difference between true bacteria and mycoplasma is that mycoplasma lack a cell wall. True bacteria have a cell wall made of peptidoglycan, which gives them shape and rigidity. Mycoplasma, on the other hand, are flexible and pleomorphic (can change shape) due to the absence of a cell wall.
The other options are incorrect:
- Flagella: Both true bacteria and some mycoplasma species can possess flagella for motility.
- ATP synthesis: Both true bacteria and mycoplasma have mechanisms for ATP synthesis, the energy currency in cells.
- A capsule: While not as common, some mycoplasma species can have capsules, a sugary layer outside the cell wall. However, the lack of a cell wall is the defining feature that distinguishes them from true bacteria.
- The organism responsible for retarding penetration of host cell by an inhibitor of ATP synthesis?
- M.pneumoniae
- Rickettsia rickettsii
- Chlamydia trachomatis
- Chlamydia psitacci
Answer and Explanation
Answer: Chlamydia trachomatis
Chlamydia trachomatis is an obligate intracellular bacterium, meaning it can only survive and replicate inside a host cell. It possesses a unique two-stage life cycle that allows it to resist some antibiotics and evade the host’s immune system. One key aspect of this cycle is the formation of an inclusion body within the host cell.
The other options are incorrect:
- M. pneumoniae: Mycoplasma pneumoniae is another bacterium, but it is not an obligate intracellular pathogen. It does not form inclusion bodies within host cells.
- Rickettsia rickettsii: Rickettsia rickettsii is also a bacterium, but it resides within the cytoplasm of host cells and does not form inclusion bodies.
- Chlamydia psittaci: Chlamydia psittaci is another species of Chlamydia, but its mechanism of pathogenesis likely does not involve retarding penetration by inhibitors of ATP synthesis.
- Mycoplasmas differ from Chalamy-diae in that, it
- has ability to cause urinary tract infection
- lack of atrue bacterial cell wall
- susceptible to penicillin
- All of these
Answer and Explanation
Answer: lack of atrue bacterial cell wall
Mycoplasmas differ from Chlamydiae in that they lack a true bacterial cell wall. Mycoplasmas are characterized by having a plasma membrane but no peptidoglycan layer typical of bacterial cell walls. This feature makes them inherently resistant to antibiotics that target cell wall synthesis, such as penicillin.
The other options are incorrect:
- Has ability to cause urinary tract infection: Mycoplasmas, including Mycoplasma genitalium and Mycoplasma hominis, can indeed cause urinary tract infections. However, this is not a distinguishing feature between mycoplasmas and Chlamydiae, as some species of Chlamydiae can also cause urinary tract infections.
- Susceptible to penicillin: Mycoplasmas are inherently resistant to penicillin due to their lack of a cell wall. Penicillin primarily targets bacteria by interfering with cell wall synthesis, which mycoplasmas lack.
- Fungal disease in human is caused by –
- Inhalation of conidia
- Invasion of mucous membrane
- Contamination of wounds with conidia or myceliat fragments
- All of these
Answer and Explanation
Answer: All of these
Fungal diseases in humans can be caused by various means, and all the options listed are valid routes for fungal infection:
- Inhalation of conidia: Fungal spores, called conidia, are lightweight and easily inhaled. They can lodge in the lungs and germinate, leading to respiratory infections.
- Invasion of mucous membrane: Fungi can invade and infect mucous membranes, such as those in the mouth, vagina, or gastrointestinal tract. This can lead to conditions like thrush or vaginal yeast infections.
- Contamination of wounds with conidia or mycelial fragments: If a wound comes into contact with fungal spores (conidia) or parts of the fungal body (mycelial fragments), it can become infected. This is especially risky for deep wounds or those with compromised healing.
- Fungi differs with bacteria in that it ?
- Contain no peptidoglycan
- Are prokaryotic
- Susceptible to griseofulvin
- All of these
Answer and Explanation
Answer: All of these
Fungi differ from bacteria in several key ways, and all the options listed are true:
- Contain no peptidoglycan: Bacterial cell walls are made of peptidoglycan, a unique structure absent in fungal cell walls. Fungal cell walls are composed of chitin, similar to the exoskeletons of insects.
- Are prokaryotic: Bacteria are single-celled prokaryotes, meaning their cells lack a defined nucleus and membrane-bound organelles. Fungi, on the other hand, are eukaryotes with complex cells containing a nucleus and other organelles.
- Susceptible to griseofulvin: Griseofulvin is an antifungal medication that disrupts fungal growth. It has no effect on bacteria.
- A polysaccharide capsule is present on cryptococci which ?
- Inhibits phagocytosis
- Is an aid to diagnose
- Cross reacts with rheumatoid factor
- All of these
Answer and Explanation
Answer: Inhibits phagocytosis
The polysaccharide capsule present on Cryptococci serves to inhibit phagocytosis by host immune cells. This capsule is a virulence factor that helps the fungus evade the host immune system by preventing phagocytic cells, such as macrophages, from engulfing and destroying the fungal cells.
The other options are incorrect:
- Is an aid to diagnose: While the presence of a polysaccharide capsule can aid in the diagnosis of cryptococcal infections, as it can be visualized using certain staining techniques, this is not the primary function of the capsule.
- Cross reacts with rheumatoid factor: Cryptococcal polysaccharide capsules do not cross-react with rheumatoid factor. Rheumatoid factor is an autoantibody that can be present in the blood of individuals with rheumatoid arthritis.
- All of these: While it is true that the polysaccharide capsule inhibits phagocytosis and aids in diagnosis, there is no evidence to suggest that it cross-reacts with rheumatoid factor.
- The bacteria, which is motile at 22oC but non-motile at 37oC is
- Tranformation
- Transduction
- Conjugation
- Cell fusion
Answer and Explanation
Answer: Cell fusion
Cell fusion refers to the process by which two or more individual cells merge to form a single cell. It is not specifically related to the temperature-dependent motility of bacteria.
The other options are incorrect:
- Transformation: Transformation is a process by which bacteria take up and incorporate foreign genetic material from their environment. It is not related to temperature-dependent motility.
- Transduction: Transduction is a process by which genetic material is transferred from one bacterium to another by a bacteriophage. It does not involve temperature-dependent motility.
- Conjugation: Conjugation is a process of genetic transfer in bacteria mediated by a conjugative plasmid or conjugative transposon. It does not involve temperature-dependent motility.
- Techoic acid is ?
- Found in the walls of Gram positive bacteria
- Provide receptors for phages
- Make up outer wall of Gram negative bacteria
- Influence the permeability of the membrane
Answer and Explanation
Answer: Found in the walls of Gram positive bacteria
Teichoic acids are a key component of the cell wall in Gram-positive bacteria. They contribute to the overall structure and rigidity of the cell wall.
The other options are incorrect:
- Provide receptors for phages: While some surface structures on bacteria can serve as phage receptors, teichoic acids are not the primary ones.
- Make up outer wall of Gram negative bacteria: Gram-negative bacteria have a different cell wall structure. Their outer membrane contains lipopolysaccharides (LPS) instead of teichoic acids.
- Influence the permeability of the membrane: Teichoic acids are located in the cell wall, not the cytoplasmic membrane. However, they can indirectly influence membrane permeability by affecting the overall structure and charge of the cell wall.
- One flagelium at one end of the organ is called ?
- Monotrichate
- Amphitrichate
- Iophotrichate
- Peritrichate
Answer and Explanation
Answer: Monotrichate
Monotrichate” refers to a bacterium having a single flagellum at one end. This flagellum is responsible for the cell’s movement.
The other options are incorrect:
- Amphitrichate: This describes bacteria with a single flagellum or multiple flagella at both ends.
- Lophotrichate: This refers to bacteria with a cluster or tuft of flagella at one or both ends.
- Peritrichate: This describes bacteria with multiple flagella distributed all over the cell surface.
- What is the function of bacterial capsule?
- Production of organism from phagocytosis
- Helps in adherence of bacteria to surface in its environment
- Both a and b
- None of these
Answer and Explanation
Answer: Both a and b
The bacterial capsule is a gelatinous layer outside the cell wall that provides several functions, including:
- Helps in adherence of bacteria to surfaces: The capsule can contain adhesive molecules that allow bacteria to stick to surfaces in their environment. This is important for colonization and can contribute to biofilm formation.
- Protects bacteria from phagocytosis: The capsule’s polysaccharide composition makes it difficult for white blood cells (phagocytes) to engulf and destroy the bacteria. This helps bacteria evade the host’s immune system.
The other options are incorrect:
- None of these: This option is incorrect as it disregards the well-established functions of the bacterial capsule. The capsule serves important roles in protection from host defenses and surface adherence, as described in options a and b.
- Which of the following is the charachteristic of bacterial spore?
- Highly refractile
- Usually dehydrated
- Sensitive to formaldehyde
- All of these
Answer and Explanation
Answer: All of these
Bacterial spores are unique dormant structures formed by certain bacteria under unfavorable conditions. They possess several characteristic features:
- Highly refractile: Bacterial spores have a thick and dense coat that bends light significantly. This makes them appear bright under a microscope when stained using specific techniques.
- Usually dehydrated: During spore formation, bacteria expel water from the cytoplasm, leading to a dehydrated state. This allows the spore to survive harsh environments for extended periods.
- Sensitive to formaldehyde: Formaldehyde is a common disinfectant that can inactivate vegetative bacteria (growing form) but may not be entirely effective against spores due to their robust structure. While some specialized sterilization techniques involving formaldehyde can target spores, they often require longer exposure times compared to vegetative cells.
- Which of the following are acid fast structures?
- Mycobacteria
- Bacterial spores
- Nocardia
- All of these
Answer and Explanation
Answer: All of these
cid-fast structures are those that resist decolorization with acid after being stained with a special dye (carbol fuchsin) during a laboratory test. Here’s why all the options are considered acid-fast:
- Mycobacteria: This is the classic example of acid-fast bacteria. They possess a thick cell wall rich in mycolic acids, which are responsible for the acid-fast staining property. Examples include Mycobacterium tuberculosis (causing tuberculosis) and Mycobacterium leprae (causing leprosy).
- Bacterial spores: While not bacteria themselves, spores of some bacteria, like those from the genus Bacillus, also exhibit acid-fastness due to the presence of a tough outer coat.
- Nocardia: This is a genus of bacteria known for being partially acid-fast. Their cell walls contain some mycolic acids, leading to variable staining results. Some Nocardia species may stain completely acid-fast, while others may appear weakly acid-fast or non-acid-fast.
- All of the following are acid fast structures except?
- Clostridium
- Bacterium spores
- Exoskeleton
- None of these
Answer and Explanation
Answer: Clostridium
Clostridium is a genus of bacteria that does not possess an acid-fast cell wall. While some Clostridium species can form spores, these spores themselves can be acid-fast, but the vegetative form (growing bacteria) of Clostridium is not.
The other options are incorrect:
- Bacterial spores: As mentioned earlier, spores of some bacteria, including some Bacillus species, are indeed acid-fast due to their tough outer coat.
- Exoskeleton: Exoskeletons are not a feature of bacteria. They are rigid external structures found in some invertebrates like insects and arthropods. Exoskeletons wouldn’t be stained by the acid-fast technique as they are not bacterial structures.
- All of the following are energy source of bacteria except?
- Oxidation of inorganic compounds
- Oxidation of organic compounds
- Absorption of heat
- Utilisation of visible light
Answer and Explanation
Answer: Absorption of heat
Bacteria are not capable of directly utilizing heat as an energy source. They rely on chemical processes to harvest energy.
The other options are incorrect:
- Oxidation of inorganic compounds: Some bacteria, called chemolithotrophs, obtain energy by oxidizing inorganic compounds like hydrogen sulfide or iron.
- Oxidation of organic compounds: Many bacteria, called heterotrophs, break down organic compounds like sugars or proteins for energy.
- Utilization of visible light: Photosynthetic bacteria use light energy to convert carbon dioxide into organic molecules for energy, similar to plants.
- Identify the obligate anaerobes?
- Salmonella
- Vibrio cholera
- Cl. tetani
- Sarcinae
Answer and Explanation
Answer: Cl. tetani
Clostridium tetani is an obligate anaerobe, meaning it can only survive and grow in the absence of oxygen. Oxygen is toxic to this bacterium.
The other options are incorrect:
- Salmonella: Salmonella is a facultative anaerobe, able to grow with or without oxygen.
- Vibrio cholera: Vibrio cholera is also a facultative anaerobe.
- Sarcinae: Sarcinae are facultative anaerobes as well. These bacteria can switch their metabolism depending on the oxygen availability.
- Streptococci which are destroyed at 60°C for 30 minutes
- Preptostreptococci
- Strepto viridans
- Strepto hemolyticus
- All of these
Answer and Explanation
Answer: All of these
The temperature and time combination of 60°C for 30 minutes is effective in destroying a variety of Streptococci species, including:
- Preptostreptococci: These are a group of lactic acid bacteria often found in the mouth and human gastrointestinal tract.
- Strepto viridans: These are common inhabitants of the human mouth and upper respiratory tract. While some strains can cause opportunistic infections, they are generally not considered highly virulent.
- Strepto hemolyticus: This species includes several groups, some of which are highly pathogenic, like Streptococcus pyogenes (causes strep throat) and Streptococcus pneumoniae (causes pneumonia).
- Toxins or enzymes which are not produced by streptococcus pyrogens
- Hyaluronides
- Phosphate
- Hemolysin
- Streptokinase
Answer and Explanation
Answer: Phosphate
Phosphate is an inorganic molecule essential for various cellular functions but is not a toxin or enzyme. Streptococci pyogenes produce a variety of toxins and enzymes that contribute to their virulence (disease-causing ability).
The other options are incorrect:
- Hyaluronidase: This enzyme breaks down hyaluronic acid, a component of connective tissue, and helps streptococci spread through tissues.
- Hemolysin: This toxin lyses (breaks open) red blood cells, contributing to some of the symptoms of streptococcal infections.
- Streptokinase: This enzyme dissolves blood clots, potentially aiding the spread of bacteria through the bloodstream.
- Dengue fever is caused by ?
- Bacteria
- Virus
- Fungi
- Rickettsia
Answer and Explanation
Answer:
Dengue fever is an infectious disease caused by a specific type of virus called the dengue virus. Viruses are much smaller and simpler than bacteria and fungi. Rickettsia are also small organisms, but they are more closely related to bacteria than viruses.
The other options are incorrect:
- Bacteria: Bacteria are single-celled organisms that can cause a variety of diseases, but dengue fever is not one of them.
- Fungi: Fungi are eukaryotic organisms that can cause infections like athlete’s foot or ringworm, but they are not responsible for dengue fever.
- Rickettsia: While Rickettsia can cause diseases like typhus, they are not the cause of dengue fever.
- Cholera red reaction is identified by
- Sulphuric acid
- Nitric acid
- Hydrochloric acid
- Carbolic acid
Answer and Explanation
Answer: Sulphuric acid
The cholera red reaction is a diagnostic test used to identify the presence of Vibrio cholerae in a stool sample. In this test, a stool sample is mixed with a small amount of concentrated sulphuric acid. If the sample turns red within a few minutes, it indicates the presence of cholera toxin, which is produced by Vibrio cholerae.
The other options are incorrect:
- Nitric acid: While Vibrio cholerae does produce nitrites, nitric acid itself is not used in the test.
- Hydrochloric acid: Hydrochloric acid wouldn’t trigger the specific reaction needed for the test.
- Carbolic acid (Phenol): Carbolic acid is not used in the cholera red reaction. It has disinfectant properties and wouldn’t promote the formation of nitrosoindole.
- Diagnosis of carrier of salmonella typhi may be shown by?
- Fecal culture
- Bile culture
- Urine culture
- All of these
Answer and Explanation
Answer: All of these
Salmonella Typhi, the bacteria responsible for typhoid fever, can be shed in various ways by carriers who don’t experience symptoms themselves. Here’s why each culture method can be useful:
- Fecal culture: This is the most common and readily available test for detecting Salmonella Typhi in stool samples. However, shedding of the bacteria can be intermittent, so multiple negative tests might not rule out a carrier state entirely.
- Bile culture: This test directly examines bile extracted from the gallbladder, where Salmonella Typhi can reside in chronic carriers. It’s considered more sensitive than stool culture but is a more invasive procedure.
- Urine culture: While less common than stool culture, Salmonella Typhi can be excreted in the urine of some carriers, making this test another option for detection.
- Daisy head colony is associated with?
- M.tuberculosis
- C.diphtheriae
- Cl. tetani
- None of these
Answer and Explanation
Answer: C.diphtheriae
Corynebacterium diphtheriae bacteria, when grown on tellurite-containing media, can form colonies with a characteristic “daisy head” appearance. These colonies are large, gray, and have a central dark core surrounded by a lighter peripheral zone.
The other options are incorrect:
- M. tuberculosis (Mycobacterium tuberculosis): This bacterium causes tuberculosis and typically forms rough, wrinkled colonies on culture media.
- Cl. tetani (Clostridium tetani): Clostridium tetani is an obligate anaerobe and wouldn’t grow on standard culture plates used for C. diphtheriae. Its colonies can appear flat, round, and with irregular edges.
- None of these: While the other options aren’t typically associated with daisy head colonies, it’s important to note that colony morphology can vary depending on the specific culture media and growth conditions.
- Neil mooseri reaction is related to?
- Rickettsiae
- Chlamydiae
- Spirochaetes
- Clostridium periringens
Answer and Explanation
Answer: Rickettsiae
The Neil Mooseri reaction, also known as the Neil Mooser phenomenon, is a serological reaction used in the diagnosis of rickettsial infections, particularly epidemic typhus caused by Rickettsia prowazekii. It involves the agglutination of Proteus OX19 strain antigen-coated particles in the presence of patient serum containing antibodies against rickettsiae.
The other options are incorrect:
- Chlamydiae: The Neil Mooseri reaction is not related to Chlamydiae. Chlamydiae are intracellular bacteria that cause diseases such as chlamydia, but they do not elicit the Neil Mooser phenomenon.
- Spirochaetes: The Neil Mooseri reaction is not related to Spirochaetes. Spirochaetes are a group of bacteria characterized by their spiral shape and include pathogens such as Treponema pallidum (the causative agent of syphilis), Borrelia burgdorferi (the causative agent of Lyme disease), and Leptospira species.
- Clostridium perfringens: The Neil Mooseri reaction is not related to Clostridium perfringens. Clostridium perfringens is a Gram-positive, spore-forming bacterium that is associated with food poisoning and gas gangrene, but it is not involved in the Neil Mooser phenomenon.
The questions are typically designed to assess the technical skills and knowledge required for the laboratory profession, including the ability to analyze laboratory test results, perform laboratory procedures, and maintain laboratory equipment.
To prepare for these MCQs, candidates should have a thorough understanding of the key concepts and principles of laboratory science. They should also be familiar with common laboratory equipment and procedures, as well as laboratory safety protocols.
Candidates may also benefit from studying specific laboratory science textbooks or taking online courses that cover the material tested in the MCQs. Additionally, practicing sample MCQs and reviewing the answers can help candidates identify areas where they may need to improve their knowledge or skills.
Overall, the MCQs for lab technologists are designed to be challenging and comprehensive, requiring candidates to demonstrate a high level of proficiency in the field of laboratory science.