Chapter 3 with our Hematology MCQs with Answer and explanations! Test your knowledge and understanding of key concepts with our complete set of multiple choice questions with detailed explanations for each answer.

MCQs:
Hematology, the study of blood and its components, plays a crucial role in the diagnosis and treatment of various medical conditions. Lab staff working in the field of haematology are responsible for performing a wide range of tests and analyses to help healthcare professionals make accurate diagnoses and treatment decisions. To excel in this field, it’s essential for lab staff to have a deep understanding of haematology, and mastering Multiple Choice Questions (MCQs) can be a highly effective way to achieve this goal.
Hematology MCQs No 101 – 150
- Which white blood cell type is responsible for producing antibodies?
- Eosinophils
- Lymphocytes
- Eosinophils
- Neutrophils
Answer & Explanation
Answer: Lymphocytes
The correct answer is Lymphocytes. They are a type of white blood cell responsible for producing antibodies, which are vital for the immune system’s ability to recognize and neutralize pathogens.
Here are the incorrect options with brief explanations:
- Eosinophils: These white blood cells are primarily involved in combating parasitic infections and allergic responses. They release toxins to destroy parasites and regulate allergic reactions.
- Neutrophils: Neutrophils are another type of white blood cell that play a crucial role in the body’s defense against infections. They primarily target and destroy bacteria by engulfing them.
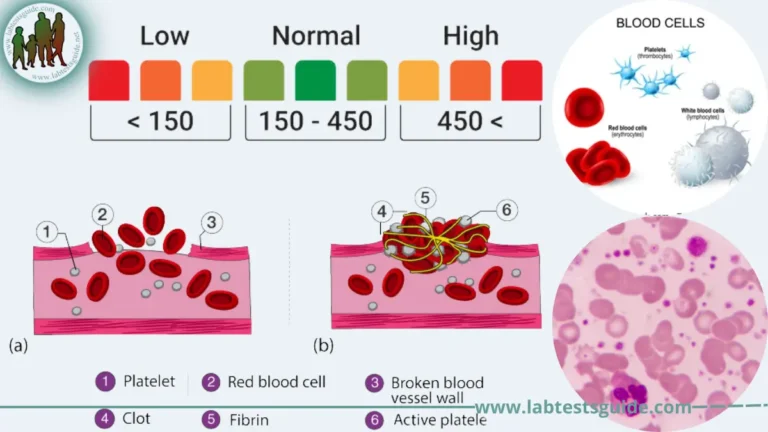
- Which of the following is a condition characterized by an excessive production of platelets, leading to an increased risk of clotting?
- Lymphoma
- Leukemia
- Hemophilia
- Thrombocytosis
Answer & Explanation
Answer: Thrombocytosis
The correct answer is Thrombocytosis. It’s a condition where there’s an abnormal increase in the number of platelets in the blood, elevating the risk of clot formation.
Here are the incorrect options with brief explanations:
- Lymphoma: Lymphoma is a cancer of the lymphatic system, characterized by the abnormal growth of cells in the lymph nodes or other lymphatic tissues.
- Leukemia: Leukemia is a type of cancer affecting the blood and bone marrow, causing an abnormal increase in white blood cells, not specifically platelets.
- Hemophilia: Hemophilia is a genetic disorder that affects the blood’s ability to clot properly due to deficiencies in specific clotting factors, particularly factors VIII or IX.
Both lymphoma and leukemia involve blood-related issues but are distinct from thrombocytosis, which specifically refers to the excessive production of platelets leading to clotting risks. Hemophilia, on the other hand, involves clotting factor deficiencies rather than an excess of platelets.
- What is the term for the process of stopping bleeding by forming a stable blood clot?
- Fibrinolysis
- Coagulation
- Thrombolysis
- Hemostasis
Answer & Explanation
Answer: Hemostasis
The correct answer is Hemostasis. It refers to the body’s process of stopping bleeding by forming a stable blood clot to prevent excessive blood loss.
Here are the incorrect options with brief explanations:
- Fibrinolysis: Fibrinolysis is the process of breaking down blood clots, not forming them. It involves the dissolution of clots when they are no longer needed.
- Coagulation: Coagulation is closely related to hemostasis but specifically refers to the initial stages of blood clot formation, involving the conversion of liquid blood to a gel-like clot.
- Thrombolysis: Thrombolysis is the medical treatment aimed at dissolving dangerous blood clots, often using medications or specialized procedures to break down existing clots that can cause blockages.
While all these terms are related to blood clotting or clot dissolution, hemostasis specifically denotes the process of forming a stable blood clot to stop bleeding, distinct from fibrinolysis, coagulation, and thrombolysis, which involve different aspects of clotting or clot breakdown.
- Which of the following is a condition characterized by an excess of iron in the body, leading to organ damage?
- Thalassemia
- Hemophilia
- Hemochromatosis
- Anemia
Answer & Explanation
Answer: Hemochromatosis
The correct answer is Hemochromatosis. It’s a condition where there’s an excessive accumulation of iron in the body, leading to potential damage in organs like the liver, heart, and pancreas due to the toxic effects of iron overload.
Here are the incorrect options with brief explanations:
- Thalassemia: Thalassemia is a genetic blood disorder involving abnormal hemoglobin production, leading to anemia. It’s not directly associated with excessive iron accumulation.
- Hemophilia: Hemophilia is a genetic disorder that affects blood clotting due to deficiencies in clotting factors, particularly factors VIII or IX. It doesn’t cause iron overload.
- Anemia: Anemia refers to a deficiency in red blood cells or hemoglobin, resulting in reduced oxygen-carrying capacity in the blood. While some forms of anemia can be associated with chronic conditions leading to iron overload, anemia itself doesn’t cause excess iron accumulation.
Hemochromatosis stands apart from these conditions as it specifically involves the excessive buildup of iron in the body, which can lead to organ damage, unlike thalassemia, hemophilia, or anemia, which have distinct causes and effects.
- What is the primary function of neutrophils in the immune system?
- Allergic reactions
- Antibody production
- Phagocytosis of bacteria
- Defense against parasites
Answer & Explanation
Answer: Phagocytosis of bacteria
Neutrophils are primarily responsible for phagocytosis, which is the process of engulfing and destroying bacteria and other foreign particles. They’re part of the body’s rapid response to infections, especially bacterial ones.
Here are the incorrect options with brief explanations:
- Allergic reactions: Neutrophils are not primarily involved in allergic reactions. While they can be present during certain inflammatory responses, their main function is related to combating infections rather than allergic processes.
- Antibody production: Antibody production is mainly carried out by lymphocytes, specifically B cells, which are a different type of white blood cell.
- Defense against parasites: Neutrophils are not the primary cells involved in defense against parasites. Eosinophils are more associated with combating parasitic infections due to their ability to release toxins to fight off parasites.
Neutrophils’ key role lies in their ability to engulf and destroy bacteria through phagocytosis, distinguishing them from cells involved in allergic reactions, antibody production, and defense against parasites.
- What is the medical term for an abnormally low level of all types of blood cells (red blood cells, white blood cells, and platelets)?
- Thrombocytosis
- Leukocytosis
- Aplastic anemia
- Pancytopenia
Answer & Explanation
Answer: Pancytopenia
Pancytopenia refers to a condition characterized by a significant decrease in the number of all types of blood cells: red blood cells, white blood cells, and platelets. It can result from various causes such as bone marrow disorders, infections, or certain medications.
Here are the incorrect options with brief explanations:
- Thrombocytosis: Thrombocytosis refers to an excessive increase in platelet count, not a decrease in all blood cell types as seen in pancytopenia.
- Leukocytosis: Leukocytosis indicates an elevated white blood cell count, but it doesn’t involve a decrease in red blood cells or platelets, which is characteristic of pancytopenia.
- Aplastic anemia: Aplastic anemia is a condition characterized by a reduction in red blood cells caused by bone marrow failure. However, pancytopenia encompasses a decrease in all blood cell types, not solely red blood cells.
Pancytopenia distinguishes itself from thrombocytosis, leukocytosis, and aplastic anemia by involving a significant reduction in the counts of all types of blood cells, which sets it apart from conditions that specifically involve an increase in platelets, white blood cells, or a decrease in only one blood cell type.
- Which laboratory test measures the percentage of red blood cells in a blood sample?
- Hematocrit
- Platelet count
- Coagulation time
- Hemoglobin
Answer & Explanation
Answer: Hematocrit
Hematocrit measures the percentage of red blood cells in a blood sample. It’s a part of a standard blood test that assesses the proportion of red blood cells in the total blood volume.
Here are the incorrect options with brief explanations:
- Platelet count: Platelet count measures the number of platelets in a blood sample, which is crucial for blood clotting, but it doesn’t assess the percentage of red blood cells.
- Coagulation time: Coagulation time measures how long it takes for blood to clot. It evaluates the blood’s clotting ability and isn’t related to the percentage of red blood cells.
- Hemoglobin: Hemoglobin is a protein within red blood cells that carries oxygen. While it’s often measured in a blood test and gives an indication of the oxygen-carrying capacity, it doesn’t directly measure the percentage of red blood cells in the blood sample.
Hematocrit is distinct from platelet count, coagulation time, and hemoglobin as it specifically measures the proportion of red blood cells in a blood sample, which is essential for assessing conditions like anemia or polycythemia.
- What is the term for the process of breaking down a blood clot?
- Thrombolysis
- Fibrinolysis
- Hemolysis
- Coagulation
Answer & Explanation
Answer: Thrombolysis
Fibrinolysis is a natural process that occurs in the body to prevent blood clots from becoming too large or lasting too long. The process involves the activation of plasmin, an enzyme that breaks down fibrin, the protein that forms the meshwork of a blood clot.
- Thrombolysis is a medical term for the use of medications to break down blood clots. Thrombolytic medications work by activating plasminogen, a precursor to plasmin.
- Hemolysis is the destruction of red blood cells.
- Coagulation is the process of blood clotting.
- Which of the following is the most mature normoblast?
- Pronormoblast
- Basophilic Normoblast
- Orthochromic Normoblast
- Polychromatic Normoblast
Answer & Explanation
Answer: Orthochromic Normoblast
An Orthochromic Normoblast is the most mature stage among the normoblasts. It’s the stage just before the normoblast becomes a fully mature red blood cell (erythrocyte). At this stage, the nucleus becomes pyknotic (condensed), preparing the cell for expulsion of the nucleus and final maturation into an erythrocyte.
Here are the incorrect options with brief explanations:
- Pronormoblast: Pronormoblast is the earliest stage in the development of red blood cells. It’s the least mature of the normoblasts and precedes the stages of basophilic, polychromatic, and orthochromic normoblasts.
- Basophilic Normoblast: Basophilic Normoblast is a stage after the pronormoblast and represents a more mature form but is still less mature than the orthochromic normoblast.
- Polychromatic Normoblast: Polychromatic Normoblast is a stage between the basophilic and orthochromic normoblasts. It’s less mature than the orthochromic normoblast but more mature than the basophilic normoblast.
Orthochromic Normoblast is the most mature stage among the options provided, representing the final stages of development before the red blood cell matures and loses its nucleus.
- Which of the following is a blood clot that has traveled from its original site and is blocking a blood vessel in another part of the body?
- Embolus
- Hematoma
- Thrombus
- Aneurysm
Answer & Explanation
Answer: Embolus
An embolus is a blood clot that has detached from its original location and traveled through the bloodstream to block a blood vessel in another part of the body. It can cause significant complications depending on where it lodges, such as pulmonary embolism if it blocks an artery in the lungs or stroke if it obstructs an artery in the brain.
Here are the incorrect options with brief explanations:
- Hematoma: A hematoma is a localized collection of blood outside the blood vessels, often caused by trauma. It’s not a blood clot that has traveled but rather a pooling of blood within tissues.
- Thrombus: A thrombus is a blood clot that forms and remains stationary at its original site within a blood vessel. It doesn’t travel to block blood vessels in other parts of the body.
- Aneurysm: An aneurysm is an abnormal bulge or ballooning in the wall of a blood vessel. While an aneurysm can lead to a rupture and subsequent internal bleeding, it’s not a blood clot that has traveled to block another blood vessel.
An embolus is distinct from a hematoma, thrombus, and aneurysm as it specifically refers to a blood clot that has detached and is blocking a blood vessel in a different part of the body, causing potential circulation complications.
- Which blood cell type is involved in the body’s immune memory and antibody production?
- Basophils
- Eosinophils
- Memory B cells
- Neutrophils
Answer & Explanation
Answer: Memory B cells
Memory B cells are a type of white blood cell that plays a crucial role in the body’s immune memory. When the body encounters a specific antigen, such as from a pathogen, some B cells become memory B cells. These cells “remember” the antigen, allowing for a quicker and more robust immune response upon subsequent exposures. They also contribute to antibody production, aiding in a faster and more targeted defense against previously encountered pathogens.
Here are the incorrect options with brief explanations:
- Basophils: Basophils are a type of white blood cell involved in allergic reactions and releasing histamine. They are not primarily associated with immune memory or antibody production.
- Eosinophils: Eosinophils are white blood cells that are important in combating parasitic infections and regulating allergic responses. They are not directly involved in immune memory or antibody production.
- Neutrophils: Neutrophils are a type of white blood cell primarily involved in the body’s immediate response to infections by engulfing and destroying pathogens. They do not have a role in immune memory or antibody production.
Memory B cells stand apart from basophils, eosinophils, and neutrophils as they specifically contribute to the immune system’s memory and antibody production, essential for recognizing and combating previously encountered pathogens.
- Which white blood cell type is primarily responsible for the production of antibodies during an immune response?
- Neutrophils
- Eosinophils
- Basophils
- Lymphocyte
Answer & Explanation
Answer: Lymphocyte
Which white blood cell type is primarily responsible for the production of antibodies during an immune response?
- Neutrophils
- Eosinophils
- Basophils
- Lymphocyte
- What is the term for the process of white blood cells engulfing and digesting foreign particles, such as bacteria?
- Hemostasis
- Phagocytosis
- Diapedesis
- Chemotaxis
Answer & Explanation
Answer: Phagocytosis
Phagocytosis is the process by which certain white blood cells, particularly macrophages and neutrophils, engulf and digest foreign particles like bacteria or other pathogens. These cells recognize, engulf, and break down the invaders to eliminate them from the body.
Here are the incorrect options with brief explanations:
- Hemostasis: Hemostasis is the process of stopping bleeding or preventing blood loss by forming blood clots. It’s not related to the engulfing and digestion of foreign particles by white blood cells.
- Diapedesis: Diapedesis refers to the movement of white blood cells out of the bloodstream and into surrounding tissues. It’s a step in the process by which white blood cells reach the site of infection but doesn’t involve the actual engulfing and digestion of foreign particles.
- Chemotaxis: Chemotaxis is the movement of cells towards or away from a chemical stimulus. While it plays a role in guiding white blood cells to the site of infection, it doesn’t specifically describe the process of engulfing and digesting foreign particles.
Phagocytosis is distinct from hemostasis, diapedesis, and chemotaxis as it specifically refers to the cellular process where white blood cells ingest and break down foreign particles, contributing to the body’s immune response against pathogens.
- Which of the following is a blood clot that forms inside a blood vessel and remains at the site of formation?
- Aneurysm
- Thrombus
- Hematoma
- Embolus
Answer & Explanation
Answer: Thrombus
A thrombus is a blood clot that forms within a blood vessel and remains at the site where it formed. It can partially or completely block the blood vessel, potentially leading to reduced blood flow or complete blockage.
Here are the incorrect options with brief explanations:
- Aneurysm: An aneurysm is an abnormal bulge or swelling in the wall of a blood vessel. It doesn’t necessarily involve the formation of a blood clot, but rather a weakened area that can potentially rupture.
- Hematoma: A hematoma is a collection of blood that has leaked from a damaged blood vessel and accumulated outside the blood vessel within tissues. It’s not a clot formed inside a blood vessel.
- Embolus: An embolus is a blood clot that has detached from its original site and traveled through the bloodstream, potentially blocking a blood vessel in another part of the body. It’s different from a thrombus, which forms and remains at the site of formation within a blood vessel.
A thrombus is distinct from aneurysms, hematomas, and emboli as it specifically refers to a blood clot that forms inside a blood vessel and stays in place, potentially causing obstruction or reduced blood flow at the site of formation.
- Which blood cell type is responsible for initiating the formation of blood clots?
- Platelets
- Red blood cells
- White blood cells
- Plasma cells
Answer & Explanation
Answer: Platelets
Platelets, also known as thrombocytes, are responsible for initiating the formation of blood clots. When there’s an injury to a blood vessel, platelets rush to the site and become activated, forming a plug to stop bleeding. They release substances that trigger a cascade of reactions leading to the formation of a blood clot.
Here are the incorrect options with brief explanations:
- Red blood cells: Red blood cells are primarily responsible for transporting oxygen from the lungs to the rest of the body and do not participate in the clotting process.
- White blood cells: White blood cells are part of the immune system and play a role in defending the body against infections. They are not directly involved in initiating the formation of blood clots.
- Plasma cells: Plasma cells are a type of white blood cell that produces antibodies, which are essential for the immune response. They do not have a direct role in initiating blood clot formation.
Platelets stand apart from red blood cells, white blood cells, and plasma cells as they specifically play a crucial role in the initial stages of forming blood clots to stop bleeding at the site of injury.
- Which of the following is a condition characterized by a low level of hemoglobin in the blood, often due to iron deficiency?
- Hemophilia
- Thalassemia
- Iron-deficiency anemia
- Sickle cell disease
Answer & Explanation
Answer: Iron-deficiency anemia
Iron-deficiency anemia is a condition marked by a low level of hemoglobin in the blood, usually due to insufficient iron in the body. Hemoglobin, which carries oxygen in red blood cells, decreases when there’s not enough iron available for its production, leading to anemia.
Here are the incorrect options with brief explanations:
- Hemophilia: Hemophilia is a genetic disorder characterized by a deficiency in clotting factors, particularly factors VIII or IX, leading to impaired blood clotting ability. It doesn’t directly involve low hemoglobin levels or iron deficiency.
- Thalassemia: Thalassemia is a genetic blood disorder where the body makes an abnormal form of hemoglobin, leading to anemia. It’s not specifically linked to iron deficiency; rather, it involves an abnormal hemoglobin structure.
- Sickle cell disease: Sickle cell disease is a genetic disorder affecting hemoglobin, causing red blood cells to become rigid and sickle-shaped. It leads to anemia but is distinct from iron-deficiency anemia as it’s caused by a different underlying mechanism.
Iron-deficiency anemia is unique among these conditions as it specifically involves low hemoglobin levels due to inadequate iron, whereas hemophilia, thalassemia, and sickle cell disease have different causes and mechanisms leading to anemia or impaired clotting without direct association with iron deficiency.
- Which blood cell type is responsible for carrying oxygen and carbon dioxide in the bloodstream?
- Plasma cells
- Platelets
- Red blood cells
- White blood cells
Answer & Explanation
Answer: Red blood cells
Red blood cells, also known as erythrocytes, are responsible for carrying oxygen from the lungs to the tissues and cells throughout the body. Additionally, they transport carbon dioxide, produced by cells, back to the lungs for exhalation.
Here are the incorrect options with brief explanations:
- Plasma cells: Plasma cells are a type of white blood cell that produces antibodies, crucial for the immune response. They are not involved in carrying oxygen or carbon dioxide in the bloodstream.
- Platelets: Platelets, or thrombocytes, are responsible for blood clotting. They play a vital role in preventing bleeding by forming clots but are not involved in gas exchange or transporting oxygen and carbon dioxide.
- White blood cells: White blood cells, or leukocytes, are a part of the immune system and are primarily responsible for defending the body against infections. They do not carry oxygen or carbon dioxide in the bloodstream.
Red blood cells are distinct from plasma cells, platelets, and white blood cells as they are specifically designed for the transport of oxygen from the lungs to the body’s tissues and cells and the transportation of carbon dioxide back to the lungs for exhalation.
- Which type of anemia is caused by a deficiency of vitamin B12 or folic acid?
- Iron-deficiency anemia
- Aplastic anemia
- Pernicious anemia
- Hemolytic anemia
Answer & Explanation
Answer: Pernicious anemia
Pernicious anemia is a type of anemia caused by the body’s inability to properly absorb vitamin B12, often due to a lack of intrinsic factor, a protein necessary for B12 absorption in the intestines. This condition can also occur due to a deficiency of folic acid. Both vitamin B12 and folic acid are crucial for red blood cell production, and their deficiency can lead to decreased red blood cell production and subsequent anemia.
Here are the incorrect options with brief explanations:
- Iron-deficiency anemia: Iron-deficiency anemia results from insufficient iron in the body, affecting the production of hemoglobin in red blood cells. It’s not directly caused by a deficiency of vitamin B12 or folic acid.
- Aplastic anemia: Aplastic anemia is a condition where the bone marrow fails to produce enough blood cells, including red blood cells, white blood cells, and platelets. It’s not specifically caused by a deficiency of vitamin B12 or folic acid.
- Hemolytic anemia: Hemolytic anemia occurs when red blood cells are destroyed faster than they are produced, leading to a low red blood cell count. It’s not caused by a deficiency of vitamin B12 or folic acid.
Pernicious anemia is distinct from iron-deficiency anemia, aplastic anemia, and hemolytic anemia as it specifically results from the body’s inability to absorb vitamin B12 or insufficient folic acid, affecting red blood cell production and leading to anemia.
- Which condition is characterized by the excessive production of red blood cells, leading to thickened blood?
- Leukemia
- Polycythemia vera
- Hemophilia
- Thrombocytopenia
Answer & Explanation
Answer: Polycythemia vera
Polycythemia vera is a condition where there’s an overproduction of red blood cells in the bone marrow, leading to an increased concentration of red blood cells in the bloodstream. This higher red blood cell count can result in thicker blood, leading to increased viscosity and potential complications such as blood clots.
Here are the incorrect options with brief explanations:
- Leukemia: Leukemia is a type of blood cancer characterized by the rapid production of abnormal white blood cells in the bone marrow, not an excessive production of red blood cells.
- Hemophilia: Hemophilia is a genetic disorder characterized by a deficiency in clotting factors, particularly factors VIII or IX. It does not involve an excess production of red blood cells.
- Thrombocytopenia: Thrombocytopenia is a condition characterized by a low platelet count, leading to an increased risk of bleeding due to impaired clotting, not an excessive production of red blood cells.
Polycythemia vera stands apart from leukemia, hemophilia, and thrombocytopenia as it specifically involves the excessive production of red blood cells, causing thickened blood and potential clotting complications.
- Which clotting factor is deficient in individuals with hemophilia B?
- Factor II
- Factor I
- Factor VIII
- Factor IX
Answer & Explanation
Answer: Factor IX
Hemophilia B, also known as Christmas disease, is a type of hemophilia caused by a deficiency or absence of clotting factor IX. This deficiency impairs the blood’s ability to clot properly, leading to prolonged bleeding episodes, particularly after injuries or surgeries.
Here are the incorrect options with brief explanations:
- Factor II: Factor II, also known as prothrombin, is a clotting factor involved in the coagulation cascade. However, deficiencies in Factor II are not associated with hemophilia B.
- Factor I: Factor I, also known as fibrinogen, plays a role in blood clotting by converting into fibrin, forming the meshwork of a blood clot. Deficiencies in Factor I are not related to hemophilia B.
- Factor VIII: Hemophilia A is caused by a deficiency in Factor VIII, not Factor IX. While both hemophilia A and B lead to impaired blood clotting, they are distinct conditions caused by deficiencies in different clotting factors.
Factor IX deficiency distinguishes hemophilia B from deficiencies in Factor II, Factor I, and Factor VIII, which are not associated with this specific type of hemophilia.
- What is the term for the liquid portion of the blood after it has clotted and the clotting factors have been removed?
- Serum
- Plasma
- Fibrinogen
- Hemoglobin
Answer & Explanation
Answer: Serum
Serum refers to the liquid portion of the blood that remains after the blood has clotted and the clotting factors, particularly fibrinogen, have been removed. It’s essentially plasma without the clotting factors, obtained by allowing the blood to clot and then separating the clot from the liquid.
Here are the incorrect options with brief explanations:
- Plasma: Plasma is the liquid component of blood that contains various proteins, electrolytes, hormones, and clotting factors. Unlike serum, plasma contains clotting factors.
- Fibrinogen: Fibrinogen is a clotting factor found in plasma that is converted to fibrin during blood clot formation. It’s not the term used to describe the liquid portion of blood after clotting and clotting factor removal.
- Hemoglobin: Hemoglobin is a protein found in red blood cells that carries oxygen. It’s not the term used to describe the liquid portion of blood after clotting and clotting factor removal.
Serum is distinguished from plasma, fibrinogen, and hemoglobin as it specifically refers to the liquid component of blood left after clotting, where clotting factors, including fibrinogen, have been removed, but other components remain present.
- Which clotting factor is essential for the formation of fibrin, the protein that forms the mesh of a blood clot?
- Factor VII
- Factor I
- Factor V
- Factor II
Answer & Explanation
Answer: Factor II
Factor II, also known as prothrombin, is a clotting factor that plays a crucial role in the coagulation cascade. When activated, prothrombin (Factor II) is converted into thrombin, which then converts fibrinogen (Factor I) into fibrin, the protein that forms the mesh or framework of a blood clot.
Here are the incorrect options with brief explanations:
- Factor VII: Factor VII is another clotting factor that participates in the coagulation cascade, but it’s not directly responsible for the formation of fibrin. It plays a role in the activation of Factor X.
- Factor I: Factor I is fibrinogen, a protein present in plasma. While it’s involved in blood clotting, it is the substrate that is converted to fibrin by thrombin (activated Factor II), rather than directly forming fibrin itself.
- Factor V: Factor V is another clotting factor involved in the coagulation cascade, but it functions in the conversion of prothrombin to thrombin. It’s not directly responsible for the formation of fibrin.
Factor II (prothrombin) stands apart from Factor VII, Factor I (fibrinogen), and Factor V as it’s specifically responsible for the conversion into thrombin, which, in turn, leads to the formation of fibrin, the meshwork of a blood clot.
- What is the term for the process of red blood cell production?
- Hemostasis
- Hematopoiesis
- Hemolysis
- Hemoglobin synthesis
Answer & Explanation
Answer: Hematopoiesis
Hematopoiesis is the process of creating new blood cells, including red blood cells (erythropoiesis), white blood cells, and platelets. It occurs primarily in the bone marrow, where hematopoietic stem cells differentiate and mature into various blood cell types.
Here are the incorrect options with brief explanations:
- Hemostasis: Hemostasis refers to the process of stopping bleeding or preventing blood loss by forming blood clots. It’s not related to the production of blood cells.
- Hemolysis: Hemolysis is the destruction or breakdown of red blood cells, which is the opposite process to their production. It’s not synonymous with the creation of new blood cells.
- Hemoglobin synthesis: Hemoglobin synthesis is the production of the hemoglobin protein within red blood cells that carries oxygen. While it’s a critical part of red blood cell maturation, it specifically refers to the production of a particular component within red blood cells, not the overall process of blood cell production.
Hematopoiesis stands apart from hemostasis, hemolysis, and hemoglobin synthesis as it specifically denotes the process of creating new blood cells, including red blood cells, white blood cells, and platelets, within the bone marrow.
- Which of the following is a genetic disorder that results in the formation of abnormal hemoglobin, causing red blood cells to become misshapen and break down easily?
- Hemophilia
- Hemochromatosis
- Thalassemia
- Sickle cell disease
Answer & Explanation
Answer: Sickle cell disease
Sickle cell disease is a genetic disorder characterized by the presence of abnormal hemoglobin, known as hemoglobin S. This abnormal hemoglobin causes red blood cells to assume a rigid, sickle-like shape instead of their normal flexible, round shape. The sickle-shaped cells can get stuck in blood vessels, leading to reduced blood flow and causing pain, organ damage, and increased susceptibility to infections. The abnormal cells also have a shorter lifespan, leading to anemia.
Here are the incorrect options with brief explanations:
- Hemophilia: Hemophilia is a genetic disorder characterized by a deficiency in clotting factors, particularly factors VIII or IX, leading to impaired blood clotting. It’s not related to abnormal hemoglobin or red blood cell shape.
- Hemochromatosis: Hemochromatosis is a genetic disorder that results in excess iron absorption by the body, leading to iron overload. It doesn’t involve abnormal hemoglobin or affect red blood cell shape.
- Thalassemia: Thalassemia is a genetic blood disorder that results in abnormal hemoglobin production, leading to anemia. However, it’s distinct from sickle cell disease, as it involves a different type of abnormal hemoglobin and doesn’t cause the characteristic sickle-shaped red blood cells.
Sickle cell disease is distinct from hemophilia, hemochromatosis, and thalassemia as it specifically involves the formation of abnormal hemoglobin, resulting in misshapen red blood cells, which can cause various health complications due to their altered shape and reduced lifespan.
- Which white blood cell type releases histamine and heparin during allergic reactions?
- Basophils
- Eosinophils
- Neutrophils
- Monocytes
Answer & Explanation
Answer: Basophils
Basophils are a type of white blood cell involved in the immune response and allergic reactions. They release histamine, which contributes to inflammation and allergic responses, and heparin, which acts as an anticoagulant to prevent blood clotting at the site of inflammation.
Here are the incorrect options with brief explanations:
- Eosinophils: Eosinophils are white blood cells primarily associated with combating parasitic infections and regulating allergic responses. While they play a role in allergies, they do not release histamine and heparin during allergic reactions as basophils do.
- Neutrophils: Neutrophils are white blood cells involved in the body’s immediate response to infections, particularly bacterial ones, through phagocytosis. They are not known for releasing histamine and heparin during allergic reactions.
- Monocytes: Monocytes are white blood cells that can transform into macrophages, which engulf and destroy pathogens. While they participate in the immune response, they do not release histamine and heparin during allergic reactions as basophils do.
Basophils stand apart from eosinophils, neutrophils, and monocytes as they specifically release histamine and heparin, contributing to allergic reactions and inflammation.
- Which of the following is a genetic condition that affects the shape of red blood cells, leading to blockages and pain crises?
- Sickle cell disease
- Hemochromatosis
- Polycythemia vera
- Hemophilia
Answer & Explanation
Answer: Sickle cell disease
Sickle cell disease is a genetic condition where the hemoglobin, a protein in red blood cells responsible for carrying oxygen, is abnormal. This abnormal hemoglobin causes the red blood cells to become rigid and sickle-shaped, leading to blockages in blood vessels, reduced blood flow, and pain crises. The sickle-shaped cells can get stuck in small blood vessels, causing tissue damage and various complications.
Here are the incorrect options with brief explanations:
- Hemochromatosis: Hemochromatosis is a genetic disorder characterized by excess absorption of dietary iron, leading to iron overload in the body’s tissues and organs. It doesn’t affect the shape of red blood cells or cause blockages and pain crises.
- Polycythemia vera: Polycythemia vera is a condition where there’s an overproduction of red blood cells, white blood cells, and platelets in the bone marrow. While it involves an increased number of red blood cells, it doesn’t alter their shape or cause blockages and pain crises like sickle cell disease.
- Hemophilia: Hemophilia is a genetic disorder characterized by a deficiency in clotting factors, leading to impaired blood clotting and increased bleeding. It doesn’t affect the shape of red blood cells or cause blockages and pain crises like sickle cell disease.
Sickle cell disease is distinct from hemochromatosis, polycythemia vera, and hemophilia as it specifically alters the shape of red blood cells, leading to blockages in blood vessels and painful crises due to the cells’ tendency to get stuck and impede blood flow.
- Which type of anemia is characterized by the destruction of red blood cells at a faster rate than they can be produced?
- Hemolytic anemia
- Aplastic anemia
- Pernicious anemia
- Iron-deficiency anemia
Answer & Explanation
Answer: Hemolytic anemia
Hemolytic anemia is a condition characterized by the accelerated destruction of red blood cells at a rate faster than the body can replace them. This premature destruction can occur due to various factors, including inherited conditions, infections, autoimmune disorders, medications, or exposure to certain toxins.
Here are the incorrect options with brief explanations:
- Aplastic anemia: Aplastic anemia is a condition where the bone marrow fails to produce enough red blood cells, white blood cells, and platelets, rather than being characterized by the destruction of red blood cells.
- Pernicious anemia: Pernicious anemia is caused by a deficiency in vitamin B12 absorption due to a lack of intrinsic factor. It primarily affects red blood cell production but doesn’t involve the destruction of red blood cells.
- Iron-deficiency anemia: Iron-deficiency anemia occurs when the body lacks sufficient iron to produce hemoglobin, leading to a decreased number of red blood cells. It’s not primarily characterized by the destruction of red blood cells at a faster rate.
Hemolytic anemia stands apart from aplastic anemia, pernicious anemia, and iron-deficiency anemia as it specifically involves the accelerated destruction of red blood cells, leading to a decreased number of circulating red blood cells compared to the rate of their production.
- What is the term for the process of breaking down hemoglobin into its component parts, including iron and heme?
- Hematopoiesis
- Hemostasis
- Hemoglobin synthesis
- Hemolysis
Answer & Explanation
Answer: Hemolysis
Hemolysis refers to the process of breaking down hemoglobin, found in red blood cells, into its component parts, including iron and heme. This breakdown occurs when red blood cells reach the end of their lifespan and are broken down by macrophages in the spleen and liver. Hemoglobin is separated into its constituents: heme, which is further degraded into biliverdin and iron, and globin, which is broken down into amino acids.
Here are the incorrect options with brief explanations:
- Hematopoiesis: Hematopoiesis refers to the formation or production of blood cells, including red blood cells, white blood cells, and platelets, rather than the breakdown of hemoglobin.
- Hemostasis: Hemostasis is the process of stopping bleeding or preventing blood loss by forming blood clots. It’s not related to breaking down hemoglobin into its parts.
- Hemoglobin synthesis: Hemoglobin synthesis is the process of creating hemoglobin within red blood cells, not the breakdown of hemoglobin into its components.
Hemolysis is distinct from hematopoiesis, hemostasis, and hemoglobin synthesis as it specifically refers to the breakdown of hemoglobin into its constituent parts, such as iron and heme, which occurs during the natural degradation of aging red blood cells.
- What is the term for the process of blood cell formation ?
- Hemostasis
- Hemolysis
- Hematopoiesis
- Hemoglobin synthesis
Answer & Explanation
Answer: Hematopoiesis
Hematopoiesis is the process of blood cell formation or production. It occurs primarily in the bone marrow, where hematopoietic stem cells differentiate and mature into various types of blood cells, including red blood cells, white blood cells, and platelets.
Here are the incorrect options with brief explanations:
- Hemostasis: Hemostasis refers to the process of stopping bleeding or preventing blood loss by forming blood clots. It’s not related to blood cell formation but rather to maintaining the integrity of blood vessels and preventing excessive bleeding.
- Hemolysis: Hemolysis is the breakdown of red blood cells and the release of their contents into the bloodstream, not the process of blood cell formation.
- Hemoglobin synthesis: Hemoglobin synthesis is the production of the hemoglobin protein within red blood cells, which is involved in carrying oxygen. While crucial for red blood cell function, it specifically refers to the production of a particular protein within red blood cells, not the overall process of blood cell formation.
Hematopoiesis stands apart from hemostasis, hemolysis, and hemoglobin synthesis as it specifically denotes the process of blood cell formation from hematopoietic stem cells in the bone marrow, giving rise to various types of blood cells necessary for oxygen transport, immune defense, and clotting.
- What is the term for the process by which blood cells move out of the bloodstream into surrounding tissues?
- Hemolysis
- Hemostasis
- Hematopoiesis
- Diapedesis
Answer & Explanation
Answer: Diapedesis
Diapedesis is the phenomenon where blood cells, particularly white blood cells or leukocytes, exit the bloodstream by squeezing through the vessel walls and entering the surrounding tissues. This process is crucial for immune responses, allowing white blood cells to reach sites of infection or injury to combat pathogens and promote healing.
Here are the incorrect options with brief explanations:
- Hemolysis: Hemolysis refers to the breakdown or destruction of red blood cells, resulting in the release of their contents into the bloodstream. It doesn’t involve the movement of blood cells out of the bloodstream into tissues.
- Hemostasis: Hemostasis is the process of preventing or stopping bleeding by forming blood clots to maintain the integrity of blood vessels. It’s not related to the movement of blood cells out of the bloodstream.
- Hematopoiesis: Hematopoiesis is the process of blood cell formation or production, occurring primarily in the bone marrow. It’s not related to the movement of blood cells out of the bloodstream into surrounding tissues.
Diapedesis specifically refers to the migration of blood cells, particularly white blood cells, from the bloodstream into the tissues, playing a critical role in the body’s immune response.
- What is the term for the liquid component of blood that contains water, electrolytes, and proteins
- Platelets
- Plasma
- Red blood cells
- Serum
Answer & Explanation
Answer: Plasma
Plasma is the straw-colored, liquid portion of blood that constitutes around 55% of total blood volume. It consists mainly of water, along with electrolytes (such as sodium and potassium) and various proteins, including albumin, globulins, and clotting factors. Plasma serves as a medium for transporting blood cells, nutrients, hormones, and waste products throughout the body.
Here are the incorrect options with brief explanations:
- Platelets: Platelets are small cell fragments in the blood that play a crucial role in blood clotting to prevent bleeding. They’re not the liquid component of blood but rather participate in the clotting process.
- Red blood cells: Red blood cells, or erythrocytes, are the most abundant cells in the blood and are responsible for carrying oxygen to the body’s tissues. They’re not the liquid component but rather cellular components of blood.
- Serum: Serum is the liquid that remains after blood clots and the clotting factors have been removed. It’s similar to plasma but lacks clotting factors like fibrinogen. While serum contains electrolytes and proteins, it’s different from plasma, which is the liquid component before clotting occurs.
Plasma is distinct from platelets, red blood cells, and serum as it specifically refers to the liquid portion of blood that carries various substances throughout the body and includes water, electrolytes, and proteins like clotting factors and albumin.
- Which term refers to the percentage of blood volume occupied by red blood cells?
- Platelet count
- Hematocrit
- Hemoglobin
- Mean Corpuscular Volume (MCV)
Answer & Explanation
Answer: Hematocrit
Hematocrit measures the proportion of red blood cells in the total blood volume.
Incorrect options:
- Platelet count: This refers to the number of platelets in a given volume of blood. Platelets are responsible for blood clotting, not red blood cell percentage.
- Hemoglobin: Hemoglobin is a protein in red blood cells that carries oxygen. While it’s related to red blood cells, it doesn’t directly measure their volume percentage.
- Mean Corpuscular Volume (MCV): MCV measures the average volume of a red blood cell. It’s not the percentage of blood volume occupied by red blood cells but rather their average size.
- Which of the following is a normal response to acute infection or inflammation?
- Increased red blood cell count
- Decreased platelet count
- Decreased white blood cell count
- Elevated white blood cell count
Answer & Explanation
Answer: Elevated white blood cell count
In response to acute infection or inflammation, the body often increases the production of white blood cells to combat the invading pathogens or address the inflammatory process.
Incorrect options:
- Increased red blood cell count: This isn’t a typical response to acute infection or inflammation. Elevated red blood cell count is more associated with conditions like polycythemia, where there’s an excess production of red blood cells.
- Decreased platelet count: Infection or inflammation typically doesn’t cause a decrease in platelet count. A reduced platelet count (thrombocytopenia) can occur due to various other reasons but isn’t a typical immediate response to acute infection.
- Decreased white blood cell count: Acute infection usually triggers an increase, not a decrease, in white blood cell count as part of the body’s immune response. Decreased white blood cell count may indicate certain medical conditions but is not a common response to acute infection or inflammation.
- What is the primary function of red blood cells?
- Blood clotting
- Oxygen transport
- Antibody production
- Phagocytosis
Answer & Explanation
Answer: Oxygen transport
Red blood cells, through the hemoglobin they contain, primarily transport oxygen from the lungs to the body’s tissues and then carry carbon dioxide back to the lungs for exhalation.
Incorrect options:
- Blood clotting: Red blood cells don’t directly participate in blood clotting. Platelets and proteins called clotting factors are primarily responsible for blood clot formation.
- Antibody production: Red blood cells are not involved in the production of antibodies. Antibodies are generated by specialized white blood cells called B lymphocytes or B cells.
- Phagocytosis: Red blood cells are not equipped for phagocytosis, the process of engulfing and destroying pathogens or debris. Certain types of white blood cells, such as macrophages and neutrophils, perform phagocytosis as part of the immune response.
- In a CBC report, what does the term “differential” refer to?
- Red blood cell count
- Hemoglobin level
- Platelet count
- A detailed breakdown of white blood cell types
Answer & Explanation
Answer: A detailed breakdown of white blood cell types
In a CBC (Complete Blood Count) report, the “differential” provides the percentages and absolute counts of different types of white blood cells, such as neutrophils, lymphocytes, monocytes, eosinophils, and basophils, allowing for a detailed assessment of the immune system’s components.
Incorrect options:
- Red blood cell count: The differential in a CBC report doesn’t refer to red blood cell counts. Red blood cells are analyzed separately in a CBC, usually including measurements like hemoglobin, hematocrit, and red blood cell indices.
- Hemoglobin level: Hemoglobin levels are a part of the CBC but not specifically categorized under the differential. Hemoglobin levels are crucial for assessing oxygen-carrying capacity but aren’t part of the differential count.
- Platelet count: Platelet counts are also part of the CBC but aren’t encompassed in the differential. Platelet counts assess the number of platelets in the blood, which is important for clotting, but they’re not part of the differential count of white blood cell types.
- A decrease in platelet count may lead to:
- Leukocytosis
- Thrombocytosis
- Thrombocytopenia
- Anemia
Answer & Explanation
Answer: Thrombocytopenia
A decrease in platelet count leads to thrombocytopenia, which is a condition characterized by an abnormally low number of platelets in the blood. This can result in an increased risk of bleeding or easy bruising.
Incorrect options:
- Leukocytosis: This term refers to an elevated white blood cell count, not a decrease in platelet count.
- Thrombocytosis: Thrombocytosis is the opposite of thrombocytopenia; it’s an abnormal increase in platelet count, not a decrease.
- Anemia: Anemia is a condition characterized by a deficiency in red blood cells or hemoglobin, leading to reduced oxygen-carrying capacity. It is not directly related to platelet count decreases.
- Which condition is characterized by a deficiency of red blood cells or hemoglobin?
- Leukemia
- Hemophilia
- Thrombocytosis
- Anemia
Answer & Explanation
Answer: Anemia
Anemia is a condition marked by a lack of enough healthy red blood cells or hemoglobin, leading to reduced oxygen-carrying capacity in the blood and often causing fatigue, weakness, and other symptoms.
Incorrect options:
- Leukemia: Leukemia is a type of cancer that affects the blood and bone marrow, causing an overproduction of abnormal white blood cells, not a deficiency in red blood cells or hemoglobin.
- Hemophilia: Hemophilia is a genetic disorder that impairs the body’s ability to form blood clots properly due to a deficiency in certain clotting factors, particularly factors VIII or IX. It doesn’t directly involve a deficiency in red blood cells or hemoglobin.
- Thrombocytosis: Thrombocytosis is a condition characterized by an excess of platelets in the blood, not a deficiency in red blood cells or hemoglobin.
- What does an elevated eosinophil count often indicate?
- Fungal infection
- Viral infection
- Bacterial infection
- Allergic reaction
Answer & Explanation
Answer: Allergic reaction
An elevated eosinophil count often indicates an allergic reaction in the body. Eosinophils are a type of white blood cell involved in the immune response against parasites and in allergic reactions.
Incorrect options:
- Fungal infection: While eosinophils might be involved in certain fungal infections, an elevated count isn’t a definitive indication of a fungal infection. Other immune cells and diagnostic tests are typically used to confirm fungal infections.
- Viral infection: Viral infections can cause various changes in the white blood cell count, but an elevated eosinophil count isn’t a typical marker for viral infections. It’s more commonly associated with allergies or parasitic infections.
- Bacterial infection: Elevated eosinophil counts are not commonly associated with bacterial infections. Bacterial infections tend to trigger different types of white blood cell responses, such as neutrophil increases, rather than eosinophil elevation.
- What is the normal range for platelet count in adults?
- 3,000-7,000/mm³
- 150,000-450,000/mm³
- 50,000-100,000/mm³
- 12-16 g/dL
Answer & Explanation
Answer: 150,000-450,000/mm³
In adults, the normal range for platelet count typically falls between 150,000 to 450,000 platelets per microliter (mm³) of blood. Platelets are crucial for blood clotting and maintaining hemostasis.
Incorrect options:
- 3,000-7,000/mm³: This range is extremely low and indicates a severe deficiency in platelets. Such low platelet counts can lead to increased risk of bleeding and are considered dangerously low.
- 50,000-100,000/mm³: While slightly closer to the normal range, this range is still significantly below the typical adult platelet count range and could lead to an increased risk of bleeding.
- 12-16 g/dL: This range represents the normal levels for hemoglobin in grams per deciliter (g/dL) of blood and is not related to platelet counts.
- What is the normal range for neutrophil count in adults?
- 20-40%
- 40-70%
- 1-4%
- 2-8%
Answer & Explanation
Answer: 40-70%
In adults, the normal range for neutrophil count typically falls between 40% to 70% of the total white blood cell count. Neutrophils are a type of white blood cell crucial for fighting off bacterial infections.
Incorrect options:
- 20-40%: This range is below the typical normal range for neutrophil count in adults and might indicate a lower-than-normal level of neutrophils, potentially affecting the body’s ability to combat infections efficiently.
- 1-4%: This range is extremely low for neutrophil count and suggests a severe deficiency that could significantly compromise the immune system’s ability to fight infections.
- 2-8%: While slightly closer to the normal range, this range is still significantly below the typical adult neutrophil count range and might indicate a lower-than-optimal immune response to infections.
- Which of the following is a common anticoagulant used in blood collection tubes for CBC testing?
- Clopidogrel
- Warfarin
- Heparin
- EDTA
Answer & Explanation
Answer: EDTA
EDTA (Ethylenediaminetetraacetic acid) is a common anticoagulant used in blood collection tubes for Complete Blood Count (CBC) testing. It helps prevent blood clotting by binding to calcium ions, thereby preserving the blood sample for analysis.
Incorrect options:
- Clopidogrel: Clopidogrel is an antiplatelet medication used to prevent blood clots in individuals at risk for heart disease or stroke. It’s not typically used as an anticoagulant in blood collection tubes.
- Warfarin: Warfarin is an oral anticoagulant used to prevent blood clots in conditions like atrial fibrillation or deep vein thrombosis. It’s not used in blood collection tubes for routine CBC testing.
- Heparin: While heparin is an anticoagulant commonly used in medical settings, it’s not typically used in blood collection tubes for CBC testing. Heparin is often used in clinical settings like hospitals for preventing blood clots in intravenous lines or in certain medical procedures.
- What is the normal range for the total white blood cell count in adults?
- 150,000-450,000/mm³
- 4,000-11,000/mm³
- 12-16 g/dL
- 4-6 million/mm³
Answer & Explanation
Answer: 4,000-11,000/mm³
In adults, the normal range for the total white blood cell count typically falls between 4,000 to 11,000 white blood cells per microliter (mm³) of blood. White blood cells play a crucial role in the immune system’s defense against infections and diseases.
Incorrect options:
- 150,000-450,000/mm³: This range represents the normal range for platelet count, not the total white blood cell count. Platelets are crucial for blood clotting, but they are distinct from white blood cells.
- 12-16 g/dL: This range represents the normal levels for hemoglobin in grams per deciliter (g/dL) of blood, not the total white blood cell count. Hemoglobin carries oxygen in the blood and is not related to white blood cell count.
- 4-6 million/mm³: This range is related to the normal range for red blood cell count, which typically falls between 4 to 6 million red blood cells per microliter (mm³) of blood. Red blood cells are responsible for carrying oxygen to the body’s tissues.
- Which parameter provides information about the average size of red blood cells?
- Mean Corpuscular Volume (MCV)
- Mean Platelet Volume (MPV)
- White Blood Cell Count (WBC)
- Mean Corpuscular Hemoglobin (MCH)
Answer & Explanation
Answer: Mean Corpuscular Volume (MCV)
MCV measures the average volume or size of red blood cells in a blood sample. It’s an important parameter used to classify different types of anemia and understand the characteristics of red blood cells.
Incorrect options:
- Mean Platelet Volume (MPV): MPV measures the average size of platelets, not red blood cells. Platelets are crucial for blood clotting, and MPV helps assess their size and function.
- White Blood Cell Count (WBC): This parameter determines the total number of white blood cells in a given volume of blood. It doesn’t provide information about the size of red blood cells but rather the quantity and types of white blood cells present.
- Mean Corpuscular Hemoglobin (MCH): MCH refers to the average amount of hemoglobin in a red blood cell but does not directly measure the size or volume of the red blood cell itself. It’s the amount of hemoglobin within each red blood cell.
- Which blood cell type lacks a nucleus when mature?
- Red blood cell
- Neutrophil
- Lymphocyte
- Platelet
Answer & Explanation
Answer: Red blood cell
Mature red blood cells lack a nucleus. They lose their nucleus during their maturation process in the bone marrow to create more space for hemoglobin, the protein responsible for carrying oxygen.
Incorrect options:
- Neutrophil: Neutrophils are a type of white blood cell that retains their nucleus when mature. They are a crucial part of the immune system and have a multi-lobed nucleus.
- Lymphocyte: Lymphocytes, another type of white blood cell, also retain their nucleus when mature. They play a vital role in the immune response and can be identified by their large, round nucleus.
- Platelet: Platelets are cell fragments, not complete cells, and they lack a nucleus throughout their life cycle. They are derived from larger cells in the bone marrow called megakaryocytes.
- Which parameter measures the average amount of hemoglobin in a red blood cell?
- Mean Corpuscular Volume (MCV)
- Mean Corpuscular Hemoglobin (MCH)
- White Blood Cell Count (WBC)
- Mean Platelet Volume (MPV)
Answer & Explanation
Answer: Mean Corpuscular Hemoglobin (MCH)
MCH measures the average amount of hemoglobin in each red blood cell. It’s calculated by dividing the total amount of hemoglobin by the total number of red blood cells in a blood sample, providing insight into the hemoglobin content within individual red blood cells.
Incorrect options:
- Mean Corpuscular Volume (MCV): MCV measures the average volume or size of red blood cells, not the amount of hemoglobin within them. It helps classify different types of anemia based on the size of red blood cells.
- White Blood Cell Count (WBC): This parameter measures the total number of white blood cells in a given volume of blood. It does not provide information about the hemoglobin content within red blood cells.
- Mean Platelet Volume (MPV): MPV measures the average size of platelets, not the amount of hemoglobin in red blood cells. Platelets play a role in blood clotting, and MPV helps assess their size and function.
- What does a high mean corpuscular hemoglobin concentration (MCHC) indicate?
- Thalassemia
- Iron deficiency anemia
- Hemolysis
- Vitamin B12 deficiency
Answer & Explanation
Answer: Hemolysis
A high mean corpuscular hemoglobin concentration (MCHC) indicates an increased concentration of hemoglobin within red blood cells. This can occur in conditions involving hemolysis, where red blood cells break down prematurely, causing an elevation in the concentration of hemoglobin.
Incorrect options:
- Thalassemia: Thalassemia is a genetic disorder affecting the production of hemoglobin in red blood cells. It typically results in lower levels of hemoglobin and smaller red blood cells, so a high MCHC is not indicative of thalassemia.
- Iron deficiency anemia: Iron deficiency anemia results in smaller, paler red blood cells due to insufficient iron for hemoglobin production. It does not typically cause a high MCHC.
- Vitamin B12 deficiency: Vitamin B12 deficiency can lead to larger red blood cells (macrocytic anemia), but it doesn’t cause a high MCHC. Instead, it results in elevated mean corpuscular volume (MCV) due to the larger size of the red blood cells.
- What is the normal range for hemoglobin levels in adult males?
- 4,000-11,000/mm³
- 150,000-450,000/mm³
- 12-16 g/dL
- 4-6 million/mm³
Answer & Explanation
Answer: 12-16 g/dL
In adult males, the normal range for hemoglobin levels typically falls between 12 to 16 grams per deciliter (g/dL) of blood. Hemoglobin is a protein in red blood cells that carries oxygen throughout the body.
Incorrect options:
- 4,000-11,000/mm³: This range represents the normal range for the total white blood cell count, not hemoglobin levels. White blood cells play a role in the immune system’s defense against infections.
- 150,000-450,000/mm³: This range represents the normal range for platelet count, not hemoglobin levels. Platelets are important for blood clotting.
- 4-6 million/mm³: This range is related to the normal range for red blood cell count, which typically falls between 4 to 6 million red blood cells per microliter (mm³) of blood. Red blood cells are responsible for carrying oxygen to the body’s tissues.
- What is the primary function of platelets in the blood?
- Phagocytosis
- Antibody production
- Oxygen transport
- Blood clotting
Answer & Explanation
Answer: Blood clotting
Platelets play a crucial role in the blood clotting process, also known as hemostasis. When there’s an injury or damage to a blood vessel, platelets gather at the site to form a plug and initiate clot formation, preventing excessive bleeding.
Incorrect options:
- Phagocytosis: Phagocytosis is the process by which certain cells engulf and digest foreign particles or pathogens. Platelets are not primarily involved in this process; it’s a function mainly attributed to certain white blood cells like macrophages and neutrophils.
- Antibody production: Antibodies are produced by specialized white blood cells called B lymphocytes or B cells. Platelets are not involved in antibody production; their primary role is in blood clotting.
- Oxygen transport: Red blood cells, not platelets, are responsible for oxygen transport. Hemoglobin in red blood cells binds to oxygen in the lungs and carries it to the body’s tissues. Platelets do not participate in oxygen transport.
- Which white blood cell type is involved in the immune response and antibody production?
- Neutrophils
- Monocytes
- Lymphocytes
- Basophils
Answer & Explanation
Answer: Lymphocytes
Lymphocytes are a type of white blood cell involved in the adaptive immune response. They play a crucial role in antibody production and help coordinate the body’s immune response by recognizing specific pathogens and creating antibodies to fight them off.
Incorrect options:
- Neutrophils: Neutrophils are a type of white blood cell involved in the innate immune response. They are primarily responsible for attacking and engulfing pathogens, particularly bacteria, as part of the body’s initial defense against infections.
- Monocytes: Monocytes are another type of white blood cell involved in the immune response. They function as phagocytes, ingesting and breaking down pathogens and cellular debris. They can also differentiate into macrophages, which play a role in antigen presentation to lymphocytes.
- Basophils: Basophils are white blood cells that release histamine and other substances involved in allergic reactions and inflammation. They’re not primarily responsible for antibody production but rather for triggering inflammatory responses.
- Which organ is primarily responsible for the production of blood cells in the human body?
- Bone marrow
- Kidney
- Spleen
- Liver
Answer & Explanation
Answer: Bone marrow
Bone marrow, found in the cavities of bones, is primarily responsible for the production of blood cells in the human body. It produces red blood cells, white blood cells, and platelets through a process called hematopoiesis.
Incorrect options:
- Kidney: While the kidneys play a crucial role in filtering the blood and producing urine, they are not responsible for the production of blood cells. Their main function relates to fluid balance, waste removal, and hormone regulation.
- Spleen: The spleen is involved in filtering the blood, removing old or damaged blood cells, and is a part of the immune system, but it does not produce blood cells.
- Liver: The liver has multiple essential functions, including detoxification, metabolism, and production of proteins. However, it is not the primary site for the production of blood cells in the human body.
FAQs:
What is Haematology?
Haematology is the branch of medicine that deals with the study of blood and blood-forming tissues.
Why are Haematology MCQs important?
MCQs in Haematology help assess and reinforce understanding of key concepts in blood-related diseases and disorders.
What are the common topics covered in Haematology MCQs?
Topics include anemia, leukemia, coagulation disorders, blood cell morphology, transfusion medicine, and more.
How can I prepare for Haematology MCQs?
Regular study, reviewing textbooks, attending lectures, and practicing with MCQs are effective preparation methods.
What are the types of anemias discussed in Haematology MCQs?
Common types include iron-deficiency anemia, megaloblastic anemia, sickle cell anemia, and thalassemia.
What is the role of coagulation in Haematology?
Coagulation is the process by which blood forms clots, and it is crucial for preventing excessive bleeding.
How are blood disorders diagnosed in Haematology?
Diagnosis involves blood tests, bone marrow examination, and sometimes genetic testing.
What is the significance of blood cell morphology in Haematology?
Blood cell morphology helps identify and classify various blood disorders based on the appearance of blood cells under the microscope.
Are there any advancements in Haematology that I should be aware of?
Stay updated on new diagnostic techniques, treatment modalities, and research findings in Haematology.
What are the key components of a complete blood count (CBC)?
CBC includes red blood cell count, white blood cell count, hemoglobin level, hematocrit, and platelet count.
How are transfusions managed in Haematology?
Transfusions involve the administration of blood or blood products to patients with certain medical conditions, such as anemia or clotting disorders.
What is the significance of bone marrow in Haematology?
Bone marrow is responsible for the production of blood cells, and abnormalities in the bone marrow can lead to various blood disorders.
What are the major challenges in treating blood cancers?
Challenges include the heterogeneity of blood cancers, the need for personalized therapies, and potential complications from treatment.
How does the immune system relate to Haematology?
The immune system plays a role in conditions such as autoimmune hemolytic anemia and immune thrombocytopenia.
What are the risk factors for developing blood clotting disorders?
Risk factors include genetic predisposition, age, obesity, and certain medical conditions.
Can you recommend any resources for Haematology MCQ practice?
Textbooks, online question banks, and practice exams from reputable sources are useful for MCQ preparation.
How is the management of hemophilia approached in Haematology?
Treatment includes clotting factor replacement therapy, and management plans are tailored to the severity of the condition.
What are some preventive measures for blood disorders?
Preventive measures may include a healthy lifestyle, genetic counseling, and vaccinations.
How does Haematology intersect with other medical specialties?
Haematology is closely related to oncology, immunology, and internal medicine, among other specialties.
What are the future trends in Haematology research?
Keep an eye on advancements in gene therapy, targeted therapies, and precision medicine in the field of Haematology.





One Comment
Comments are closed.