Agglutinins Test – Blood Antibody Test for Hemolytic Anemia & Infections
An agglutination test, particularly the cold agglutination test, looks for antibodies that cause red blood cells to clump together at low temperatures, helping to diagnose conditions such as autoimmune hemolytic anemia (AIHA) or certain infections (such as mycoplasma pneumonia) by detecting abnormal agglutination or destruction of red blood cells and guiding treatment of conditions in which red blood cells are destroyed by cold.

LTG Test Insight PRO
Advanced Clinical Interpretation Engine
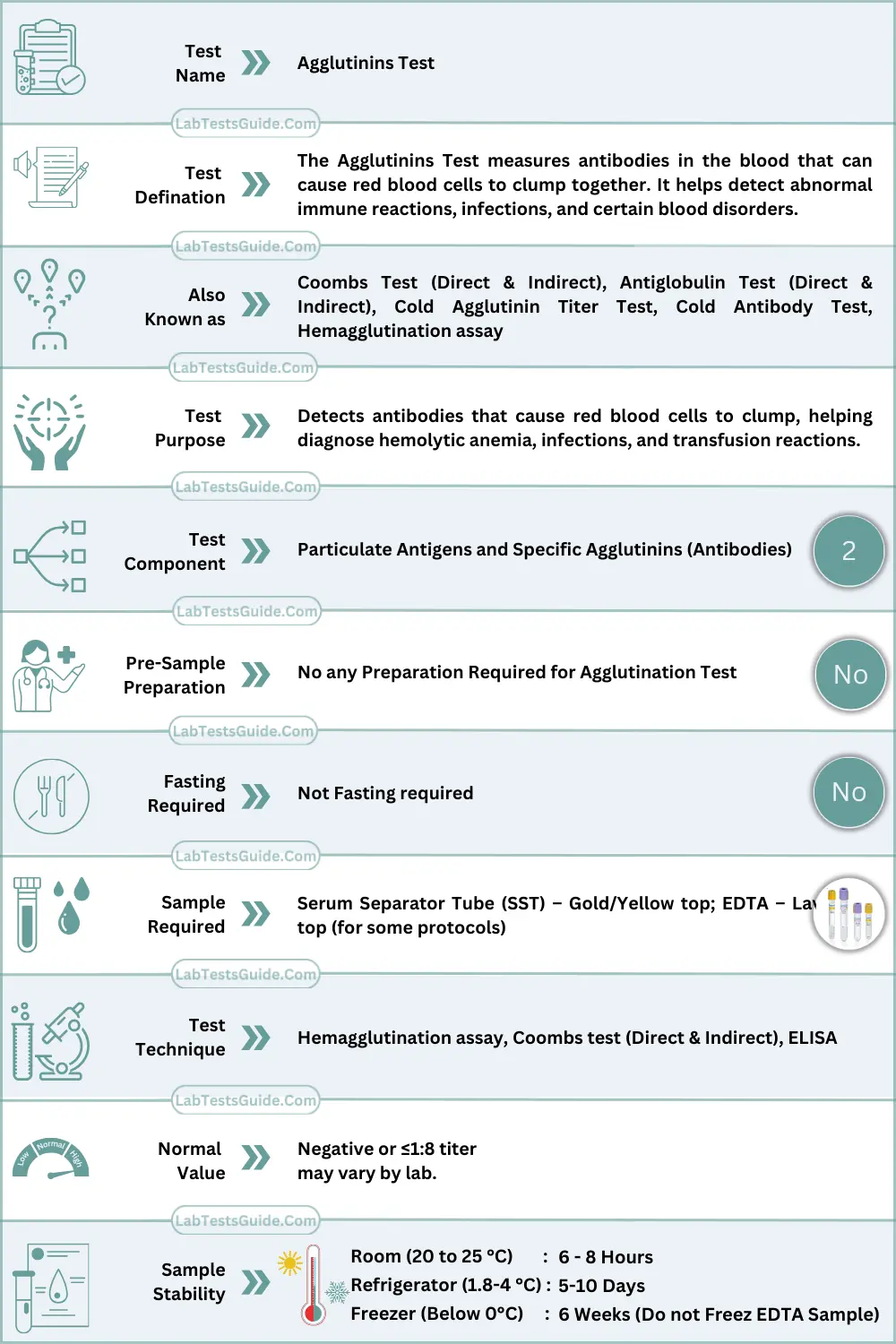
Agglutinins Test Quick Facts:
What is Agglutinins Test ?
The Agglutinins Test measures antibodies in the blood that can cause red blood cells to clump together. It helps detect abnormal immune reactions, infections, and certain blood disorders.
Why is Agglutinins Test Done? (Indications)
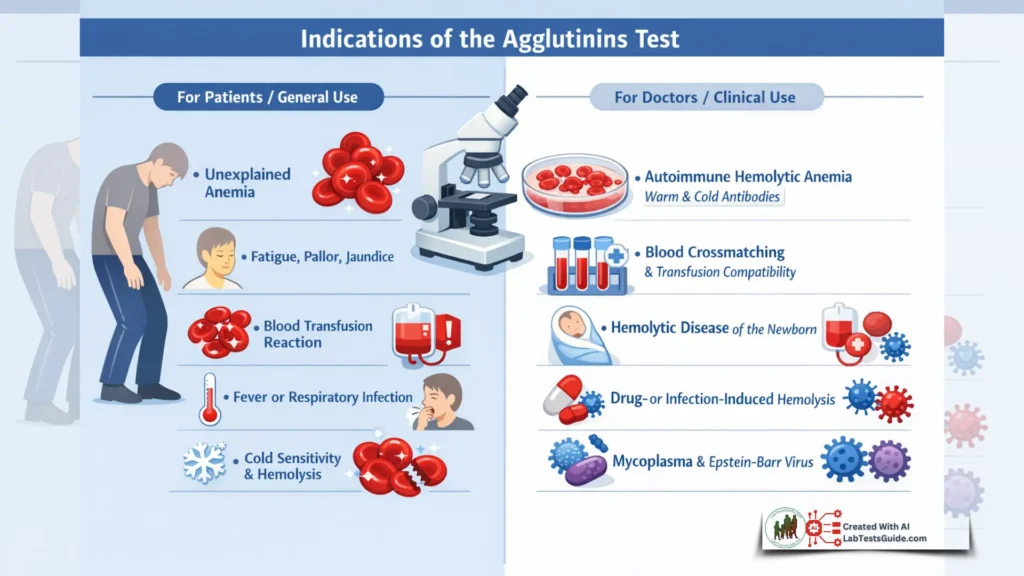
For Patients / General Use
- Unexplained anemia
- Fatigue, pallor, jaundice
- Recent transfusion reactions
- Signs of infection such as fever or respiratory symptoms
- Persistent cold sensitivity or hemolytic episodes
For Doctors / Clinical Use
- Diagnosing autoimmune hemolytic anemia (warm or cold antibody type)
- Evaluating transfusion compatibility (crossmatch)
- Monitoring hemolytic disease of the newborn
- Detecting post-infectious or drug-induced hemolysis
- Investigating Mycoplasma pneumoniae or Epstein-Barr virus infections
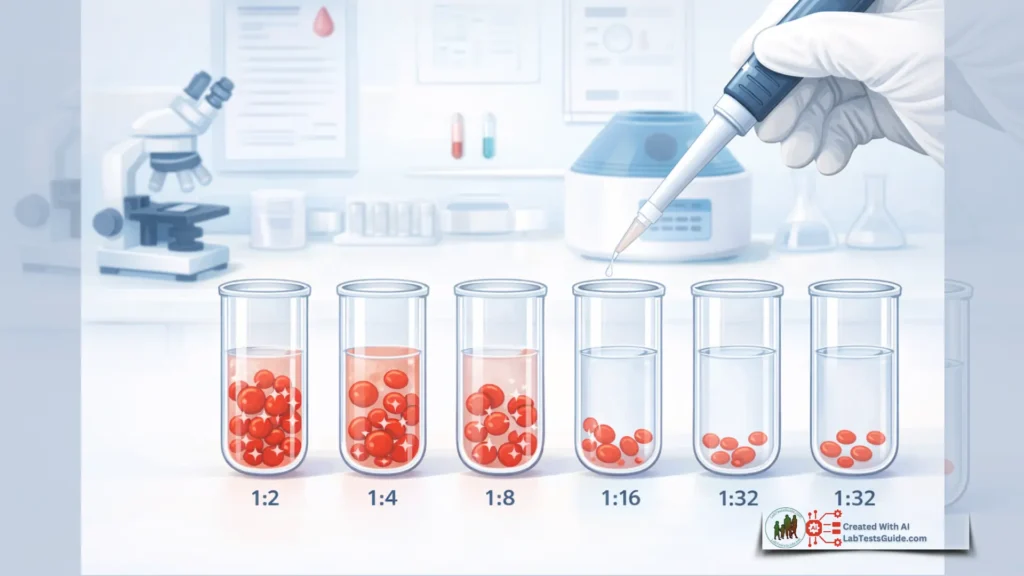
How the Agglutinins Test Works (Principle / Methodology)
Agglutinins are antibodies that bind to antigens on red blood cells, causing them to clump (agglutinate).
- Direct Coombs Test (DCT): Detects antibodies bound to patient RBCs.
- Indirect Coombs Test (ICT): Detects free antibodies in the serum.
- Hemagglutination assay: Measures antibody titers via visible clumping.
- ELISA or immunoassays: Quantitative detection of specific antibodies.
Agglutinins Test Specimen Requirements & Collection
| Parameter | Details |
|---|---|
| Specimen type | Serum or plasma |
| Tube type | SST – Gold/Yellow, EDTA – Lavender (if required) |
| Volume | 2–3 mL |
| Patient preparation | No fasting required; avoid hemolyzed samples |
| Collection steps | 1. Apply tourniquet. 2. Disinfect site. 3. Draw blood using standard phlebotomy technique. 4. Invert tube gently. |
| Transport & storage | Store serum at 2–8°C if testing within 24 hours; for longer storage, freeze at –20°C. Avoid repeated freeze-thaw cycles. |
Agglutinins Test Reference Ranges
| Population | Reference Range | Units |
|---|---|---|
| Adults | Negative or ≤1:8 titer | Titer |
| Pediatric | Negative or ≤1:8 titer | Titer |
| Pregnancy | Usually negative; clinical context needed | Titer |
Note: Reference ranges vary slightly depending on laboratory and method.
Agglutinins Test Interpretation of Results
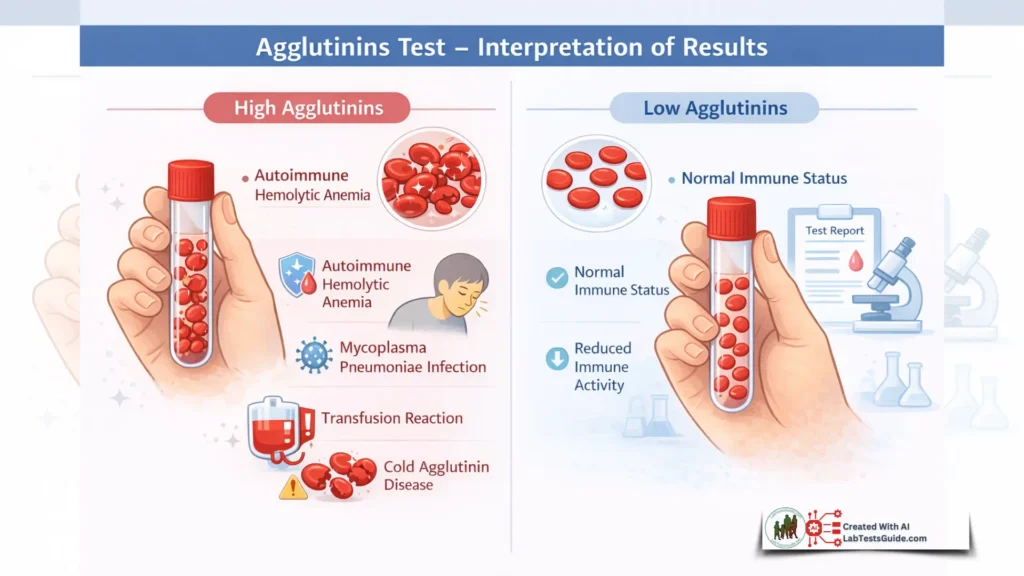
High Levels (Causes & Clinical Significance)
- Causes: Autoimmune hemolytic anemia, Mycoplasma pneumoniae infection, infectious mononucleosis, transfusion reactions, cold agglutinin disease
- Differential diagnoses: Hemolytic anemia, paroxysmal cold hemoglobinuria, drug-induced hemolysis
- Clinical relevance: High agglutinin titers may lead to RBC destruction, anemia, jaundice, and need for transfusion or immunosuppressive therapy
Low Levels (Causes & Clinical Significance)
- Causes: Normal variation, immunodeficiency, immunosuppressive therapy
- Differential diagnoses: Rare; generally not clinically significant unless symptomatic
- Clinical relevance: Low or absent agglutinins usually indicate normal status or reduced immune activity
Agglutinins Test Interfering Factors / Pre-Analytical Errors
- Hemolysis effect: May cause false positives or obscure results
- Lipemia: Can interfere with visual hemagglutination reading
- Icterus: Minimal effect; monitor for turbidity
- Medications: Immunosuppressants, monoclonal antibodies
- Sample handling issues: Delayed separation, temperature extremes
- Biological variations: Age, pregnancy, recent infections
Agglutinins Test Critical Values / PANIC Values
- High titer (e.g., >1:256) in symptomatic patients may be clinically urgent.
- Follow institution policy for urgent reporting.
Agglutinins Test Demo Lab Report Formate:
Agglutinins Test Nursing / Phlebotomy Notes
- Use correct tube (SST or EDTA)
- Properly label patient details
- Transport at 2–8°C
- Avoid hemolysis and contamination
- Document collection time and date
Lab Student Key Points
- Agglutinins = antibodies causing RBC clumping
- Direct vs. Indirect Coombs test
- Hemagglutination assay principle
- Cold vs. warm agglutinins
- Clinical relevance in autoimmune hemolysis
Do I need to fast for the test?
No, fasting is not required.
Can medications affect results?
Yes, immunosuppressants or certain antibodies may interfere.
Is this test painful?
Standard blood draw; minor discomfort possible.
How long to get results?
Usually 24–48 hours.
Does a high result mean disease?
Not always; clinical context is essential.
Can it detect infections?
Yes, some infections like Mycoplasma pneumoniae may elevate agglutinins.
Is it safe during pregnancy?
Yes, but interpretation may differ.