Pap Stain: Introduction, Principle, Staining Procedure, Result Interpretation and Keynotes
The Papanicolaou Stain – PAP Stain is designed to differentiate between a variety of cells in vaginal smears for the detection of vaginal, uterine, and cervical cancer. Additionally, this procedure is valuable for staining a variety of other body secretions and cell smears. The procedure was developed in the early 1942s by George Papanicolaou.
While not originally designed to detect anything other than cancer, the Pap smear has proven useful in identifying other, unsuspected problems. Generally, the Pap smear detects about:
- 90% of cervical cancers,
- 50% of uterine cancers. and
- 10% of ovarian cancers
- It is a polychromatic stain that uses multiple dyes to differentially stain various components of cells.
- It is a histological and cytopathological staining technique used to differentiate cells in a smear preparation.
- It is the most common screening method for cervical cancer.
- Various samples can be used to prepare the Pap smear depending on the screening infection, including sputum, urine, cerebrospinal fluid, abdominal fluid, tumor biopsies, synovial fluid, fine-needle aspirates, pleural fluids.
- The technique was developed by George Papanicolaou in 1940.
Frequency of Pap Smears:
Until recently, most experts recommended annual screening with Pap tests for adult women. Based on experience gained from annual screening, some newer recommendations have been developed to improve the economic and medical efficiency of Pap testing. These recommendations (American Cancer Society) include:
- Evaluation must begin no later than age 21.
- Screening should begin before age 21 if the patient is sexually active. In this case, it should start 3 years after the start of vaginal intercourse.
- Once started, screening should be done annually if a traditional glass slide-based technique is used. If a liquid medium is used, the Pap test can be done every two years.
- After age 30, for women who have had 3 normal Pap tests in a row, the frequency of testing may be reduced to every two to three years.
- Women who are HIV-positive, immunocompromised due to illness or medication, or who are DES daughters should continue annual screening.
- Screening may be stopped after a total hysterectomy (including the cervix), if the patient is at low risk and has had three consecutive normal Pap tests in the past 10 years.
- High-risk patients, including those with a history of cervical cancer, DES exposure in utero, HIV positive, immunocompromised by medication, and those who have tested positive for HPV, should continue to be evaluated indefinitely.
- Screening can be stopped after age 70, if the patient is low risk and has had three normal Pap tests in the past 10 years.
- Screening may be skipped for women with life-threatening or other serious illnesses.
Take Sample:
Make a Thin Smear:

Spread the sample taken from the cervix on a glass slide. Try to make the smear as thin as possible since this makes it easier for the pathologist to read. Make sure the slide is labeled (using pencil on the frosted end).In your zeal to make a thin slide, don’t spend too much time or else the slide will dry, making it harder to read.
Spray Immediately:
Immediately spray the glass slide with cytological fixative.If the slide is not immediately sprayed (within about 10-15 seconds), the smear will dry out, making interpretation more difficult or impossible.If cytological spray is unavailable, any material that has a significant amount of acetone in it can be a reasonably good substitute. Hair spray works well.
PAP Staining Onjectives:
- To define the cell nucleus to aid in the identification of nuclear abnormalities of cancer cells.
- To stain the cytoplasm and make it transparent for viewing.
- To differentiate and identify certain types of cells such as acidophiles and basophils.
The Principle of PAP Stain:
Staining uses both basic and acidic dyes, so that the basic dye stains the acidic components of the cell while the acidic dyes stain the basic components of the cells. This is based on the ionic charges of the cell components with the principle of attraction and repulsion of ions and dyes. Five dyes in three solutions are used as the main reagents used in staining.
- Hematoxylin: This is a natural dye that stains the nuclear blue of the cell. The dye binds to sulfate groups on DNA because it has a high affinity for nuclear chromatin. The most common hematoxylin stains used are Harris’ hematoxylin, Gills’ H is the most common cytologically, although Gills’ hematoxylin and hematoxylin S.
- Orange Green 6: It is an acid counterstain that stains the cytoplasm of mature keratinized cells. Components of white are stained orange at different tint intensities.
- Eosin Azure: This is the second counterstain, a combination of eosin Y, light green SF, and Bismarck brown. Eosin Y stains the cytoplasm of mature squamous cells, nucleoli, red blood cells, and cilia pink. Commonly used eosin stains are EA 31 and EA 50, while EA 65. Light green SF stains the cytoplasm of active cells, such as columnar cells, parabasal squamous cells, and intermediate squamous cells blue. Bismarck Brown Y does not stain anything and is sometimes omitted.

Requirements for Pap Stain
Required reagent and equipment are-
- Harris’s alum hematoxylin
- 0.5% (v/v) hydrochloric acid in distilled water.
- 0.25% (v/v) hydrochloric acid in distilled water
- Orange G (OG) and EA- 36 or 50 (Eosin – Azure)
- Ethanol
- Alcohol
- Distilled water
- Xylene
- Glass Slides
- Timer
- Coverslip
- Mounting media
- Coplin jars
- Compound microscope
Reagents Compositions of PAP Stain:
Harris’ hematoxylin
| Hematoxylin | 2.5 grams |
| Ethanol | 25 ml |
| Potassium alum | 50 grams |
| Distilled water (50°C) | 500 ml |
| Mercuric oxide | 1-3 grams |
| Glacial acetic acid | 20 ml |
Orange G 6
| Orange G (10% aqueous) | 25 ml |
| Alcohol | 475 ml |
| Phosphotungstic acid | 0 – 8 grams |
EA 50
| 0.04 M light green SF | 5 ml |
| 0.3M eosin Y | 10 ml |
| Phosphotungstic acid | 1 gram |
| Alcohol | 365 ml |
| Methanol | 125 ml |
| Glacial acetic acid | 10 ml |
Procedures:
Fixation: Fix smear according to standard procedure. For example, 95% alcohol or 100% methanol.
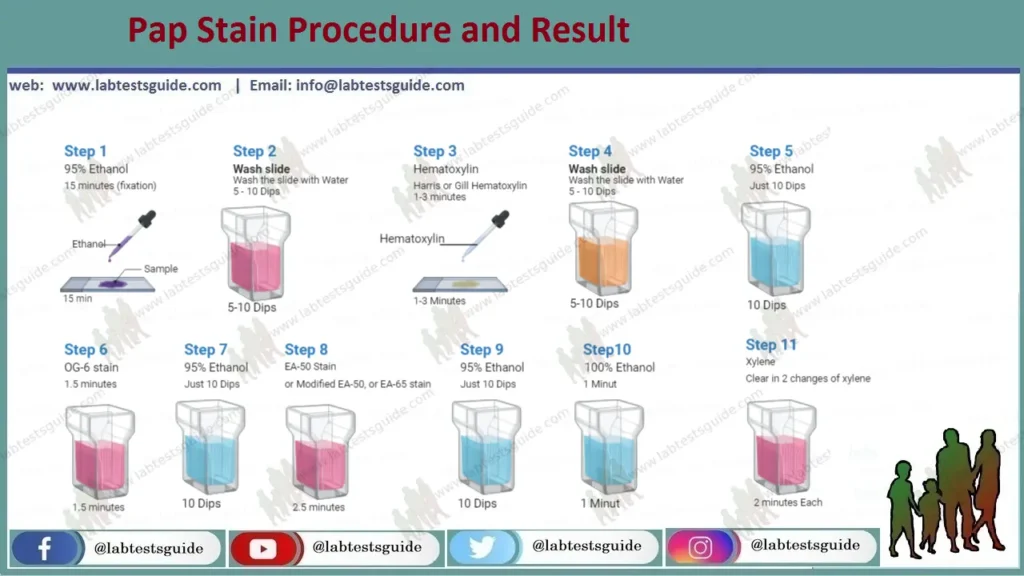
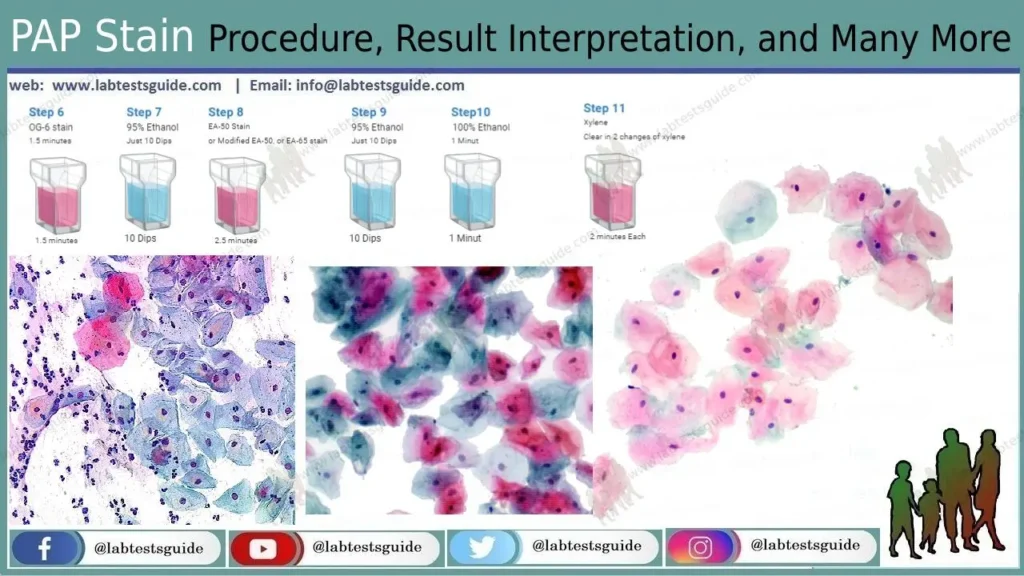
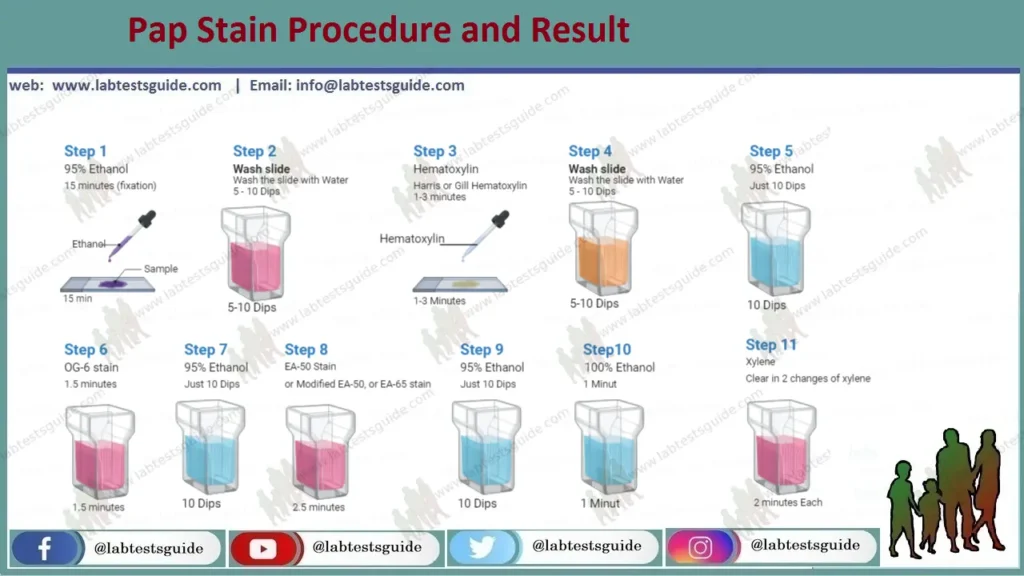
Procedure 1 (Standard Method):
- 95% Ethanol 15 minutes (fixation)
- Rinse in tap water
- Harris or Gill Hematoxylin 1-3 minutes (Time vary with selection of hematoxylin solution)
- Rinse in tap water or Scott’s tap water
- 95% Ethanol 10 dips
- OG-6 stain for 1.5 minutes.
- 95% Ethanol 10 dips
- EA-50, or Modified EA-50, or EA-65 stain for 2.5 minutes.
- 95% Ethanol 10 dips, 2 changes
- 100% Ethanol 1 minute
- Clear in 2 changes of xylene, 2 minutes each
- Mount with permanent mounting medium
Procedure 2 (Modified Pap Procedure):
- 95% Ethanol 15 minutes (fixation)
- Distilled water 10 dips, 2 changes
- Gill Hematoxylin 2 minutes
- Distilled water 10 dips
- Scott’s tap water 1 minute
- Distilled water 10 dips, 2 changes
- 95% Ethanol 10 dips, 2 changes
- OG-6 stain for 1-2 minutes
- 95% Ethanol 10 dips, 3 changes
- EA-50 or EA-65 stain for 6-10 minutes
- 95% Ethanol 20-30 dips, 3 changes
- Absolute ethanol 10 dips
- Clear in xylene
- Mount with permanent mounting medium
Procedure 3 (Rapid Economic, Acetic Acid, Papanicolaou Stain Method):
- 1% acetic acid 10 dips
- Harris’s Haematoxylin, preheated 60˚ C 10 dips
- Tap water 10dips
- 1% acetic acid 10 dips
- OG-6 10dips
- 1%acetic acid 10 dips
- EA-50 10 dips
- 1% acetic acid 10 dips
- Methanol 10 dips
- Xylene 10 dips
Interpretation:
PAP Stain Interpretation :
| Nuclei | Blue |
| Acidophilic cells | Red |
| Basophilic cells | Blue Green |
| High Keratin Cells | Orange |
| Eosinophil | Orange Red |
| Superficial Cells | Pink |
| Erythrocytes | Orange-red to Dark Pink |
| Parabasal Cells | Blue/Green |
| Intermediate Cells | Blue/Green |
| Metaplastic Cells | May contain both Blue/Green and Pink |
| Candida | Red |
| Trichomonas | Gray – green |
Keynote on Pap Staining:
- A Pap smear, often referred to as a Pap smear, is a screening technique for cervical cancer. Examines your cervix for the presence of precancerous or cancerous cells. The cervix is the opening of the uterus.
- There are two types of Pap smear procedures: a. Regressive method: first overstaining and then bleaching with hydrochloric acid for differentiation and is commonly used. b. Progressive method – stains are applied in a strict sequence. There is no need for washing or bleaching. It is applicable for samples that do not adhere well to glass.
- The clinical meanings of Pap smear are in Pap smear (Pap smear), cervical cancer screening, myeloma cancer cell examination of the liver, thyroid cancer screening, cellular carcinomas, examination and characterization of benign tumors, identification of Candida and Chlamydia trachomatis.
- Pap tests are useful only after age 21 and women who are at increased risk of cancer or infection, are HIV positive, have a weakened immune system from chemotherapy, or an organ transplant. Women age 65 with a history of normal Pap smear results may not need to be tested in the future.
- Do not allow smears to dry out and can be left in fixative for 3 days if necessary, but prolonged fixation affects staining reaction.
- Slides must be handled with care during rinsing and washing. Rough handling can wash out the sample.
- A good Pap smear should contain endocervical cells.