Chapter 52 with our Microbiology MCQs and explanations! Test your knowledge and understanding of key concepts with our complete set of multiple choice questions with detailed explanations for each answer. Increase your confidence and understanding of the fascinating world of microorganisms!

Microbiology is the study of living organisms that are not visible to the naked eye. All microorganisms such as amoebae, protozoa, viruses, bacteria are studied in microbiology. Microbes play a major role in nutrient cycling, decomposition, food spoilage, disease control and causation, and biotechnology. Due to their versatile nature, they can be used for different purposes.
Below is a set of microbiology MCQs along with the answers for your reference. These will help students improve their conceptual knowledge.
Microbiology MCQs 2551 to 2600
- Which factor would interfere with the growth of a pathogen:
- appropriate nutrients
- darkness
- a moist environment
- an acidic pH
Answer and Explanation
Answer: an acidic pH
Most pathogens, like bacteria and fungi, thrive in neutral or slightly alkaline environments (pH 7-8). An acidic environment (pH below 7) disrupts their internal processes and can inhibit their growth or even kill them. This is why some preservation methods involve using acidic ingredients like vinegar or lemon juice.
The other options are incorrect:
- Appropriate nutrients: Pathogens require nutrients for growth and reproduction. Providing them with appropriate nutrients would actually facilitate their growth, not hinder it.
- Darkness: While some pathogens may have specific light requirements for certain functions, darkness alone wouldn’t necessarily interfere with their growth. Many pathogens can grow in the dark, especially if other suitable conditions are present.
- A moist environment: Moisture is often essential for the growth and survival of pathogens. A dry environment can actually be detrimental to them, as many pathogens require moisture to function properly.
- The purpose of heat fixing a bacterial smear is to:
- prevent cells from being washed off during staining
- causes the cells to absorb the stain more easily
- provide a warm temperature for the bacteria to grow
- make the cells visible under the microscope
Answer and Explanation
Answer: prevent cells from being washed off during staining
Heat fixing essentially “cooks” the bacterial cells onto the slide, denaturing their proteins and causing them to adhere firmly. This prevents them from being washed away during the subsequent staining processes, ensuring they are available for microscopic observation.
The other options are incorrect:
- Cause the cells to absorb the stain more easily: While heat fixation might play a minor role in stain penetration, it’s not the primary purpose. Specific chemicals used in the staining process are responsible for facilitating stain absorption by the bacterial cells.
- Provide a warm temperature for the bacteria to grow: Heat fixing involves a brief exposure to flame, not a sustained warm environment. This heat kills the bacteria and wouldn’t promote their growth.
- Make the cells visible under the microscope: Although heat-fixed bacteria become slightly more visible due to protein denaturation, they are still too small to be directly observed with the naked eye. They require staining to be visualized under a microscope with sufficient magnification.
- The site of a specimen must be written on a swab container:
- to warn staff about a possible pathogen
- only if time permits-it is always on the requisition
- to determine suitable agar and atmospheric requirements
- to determine the o.h.i.p. fee
Answer and Explanation
Answer: to determine suitable agar and atmospheric requirements
The site of the specimen directly affects the type of bacteria or other pathogens most likely present. This information helps the laboratory choose the appropriate agar and atmospheric conditions (e.g., oxygen availability) needed to cultivate and identify the specific microorganisms. For example, a throat swab would likely require different culture media and conditions compared to a stool sample.
The other options are incorrect:
- To warn staff about a possible pathogen: While the site of the specimen may suggest potential pathogens, the primary purpose of labeling is not to warn staff. Specific biohazard labeling procedures are already in place for handling potentially infectious materials.
- Only if time permits – it is always on the requisition: Labeling the specimen container directly with the site is crucial even if a requisition form is filled out. The container label serves as a readily accessible reference for lab personnel, whereas the requisition might be processed separately.
- To determine the o.h.i.p. fee (applicable to Canada): The o.h.i.p. (Ontario Health Insurance Plan) fee schedule is based on the specific test requested, not the specimen site. While the site might influence the test chosen, it’s not directly used for fee determination.
- Identify the correct sequence of steps on the gram stain procedure:
- primary stain, secondary stain, mordant, decolorizing
- mordant, primary stain, decolorizing, counterstain
- counterstain, mordant, primary stain, decolorizing
- primary stain, mordant, decolorizing, counterstain
Answer and Explanation
Answer: primary stain, mordant, decolorizing, counterstain
The Gram stain procedure follows a specific order to differentiate between Gram-positive and Gram-negative bacteria based on their cell wall structure. Here’s a breakdown of the steps.
- Primary stain (usually crystal violet)
- Mordant (usually iodine)
- Decolorizing agent (usually alcohol or acetone)
- Counterstain (usually safranin)
The other options are incorrect:
- Mordant, primary stain, decolorizing, counterstain: This order places the mordant before the primary stain, which wouldn’t allow the mordant to enhance crystal violet penetration.
- Counterstain, mordant, primary stain, decolorizing: This order illogically places the counterstain before the primary stain and mordant, staining unstained cells and potentially affecting the primary stain’s effectiveness.
- Secondary stain is not a typical term used in the Gram stain procedure. While safranin is a counterstain, it’s not referred to as a secondary stain in this context.
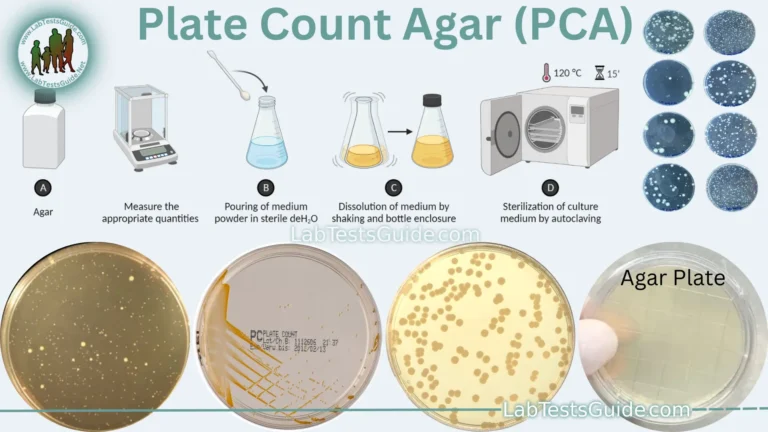
- How should commercially prepared culture plates be stored:
- inverted to prevent condensation dripping on the media
- at a temperature of 2C – 4C
- in the freezer until several hours before use
- Option inverted to prevent condensation dripping on the media and at a temperature of 2C – 4C
Answer and Explanation
Answer: Option inverted to prevent condensation dripping on the media and at a temperature of 2C – 4C
Commercially prepared culture plates should be stored inverted to prevent condensation from dripping onto the agar surface, which can interfere with bacterial growth and interpretation of results. Additionally, these plates should be stored at a temperature of 2°C – 4°C (refrigerated conditions) to maintain the viability and integrity of the included microorganisms.
The other options are incorrect:
- Freezer storage: Freezing the media can cause the water in the agar to expand and damage the gel structure, rendering it unsuitable for bacterial growth.
- Temperature not specified: While not explicitly stated in the incorrect options, storing plates at room temperature is generally not recommended as it can accelerate media dehydration and potentially compromise sterility.
- Which Gram stain reagent acts as a mordant to bind the stain to the bacteria:
- Lugol’s iodine
- safranin
- acetone-alcohol
- Gram’s iodine
Answer and Explanation
Answer: Gram’s iodine
Gram’s iodine is a key component of the Gram staining process. It acts as a mordant, which means it enhances the binding of the primary stain (crystal violet) to the bacterial cell wall. This step is crucial for differentiating Gram-positive and Gram-negative bacteria based on their cell wall structure.
The other options are incorrect:
- Lugol’s iodine: While similar in name, Lugol’s iodine often refers to a weaker iodine solution used in other applications. In the Gram stain, specifically Gram’s iodine is used due to its specific formulation and concentration.
- Safranin: This is a counterstain used in the Gram stain to visualize Gram-negative bacteria after they are decolorized with an alcohol-acetone solution. It doesn’t act as a mordant.
- Acetone-alcohol: This is the decolorizing agent used in the Gram stain procedure. It removes the crystal violet-iodine complex from the cell walls of Gram-negative bacteria, but it doesn’t function as a mordant.
- Identify the false statement regarding blood culture collection:
- the site is cleaned with betadine and alcohol
- an arterial sample is collected
- an aerobic specimen is required
- blood culture tubes are always drawn first
Answer and Explanation
Answer: an arterial sample is collected
Blood cultures are never collected from arteries. Arteries carry oxygenated blood away from the heart to the rest of the body, and puncturing an artery is a risky procedure not typically performed for blood cultures. Veins, which carry deoxygenated blood back to the heart, are the preferred route for blood culture collection.
The other options are incorrect:
- The site is cleaned with betadine and alcohol: While povidone-iodine (betadine) is not always the preferred choice (depending on facility protocols), cleaning the venipuncture site with an antiseptic solution like betadine or alcohol is a standard practice to minimize the risk of contamination.
- An aerobic specimen is required: Blood cultures typically involve collecting two sets of blood culture bottles, one aerobic and one anaerobic, to capture a wider range of potential bacteria.
- Blood culture tubes are always drawn first: While it’s recommended to draw blood cultures before starting antibiotic therapy to avoid interfering with bacterial growth, drawing blood cultures first is not always feasible depending on the clinical context. Other blood tests might be necessary simultaneously.
- Susceptibility testing:
- identifies the types of micro-organisms in the specimen
- determines growth requirements of organisms
- produces a pure culture
- identifies the appropriate antibiotic needed to kill the micro-organism
Answer and Explanation
Answer: identifies the appropriate antibiotic needed to kill the micro-organism
Susceptibility testing is a laboratory procedure used to determine the effectiveness of different antibiotics against a specific microorganism (bacteria, fungus, etc.) isolated from a patient’s sample. It helps healthcare providers choose the most appropriate antibiotic for treatment, considering factors like:
The other options are incorrect:
- Identifies the types of micro-organisms in the specimen: While this might be an initial step in the diagnostic process, susceptibility testing typically focuses on a specific microorganism already identified through other methods like culturing and staining.
- Determines growth requirements of organisms: This information might be obtained through preliminary culture observations, but it’s not the primary purpose of susceptibility testing.
- Produces a pure culture: This is the function of isolation procedures using selective and differential media, not susceptibility testing. While a pure culture is often needed before susceptibility testing, it’s a separate step.
- The autoclave is set at _ for small loads:
- 121°C for 50min at 6 p.s.i.
- 130°C for 30min at 30 p.s.i.
- 121°C for 15min at 15 p.s.i.
- 121°C for 45min at 15 p.s.i.
Answer and Explanation
Answer: 121°C for 15min at 15 p.s.i.
Standard sterilization cycles for autoclaves usually involve a temperature of 121°C (250°F) for a minimum of 15 minutes at a pressure of 15 psi (pounds per square inch). This combination of temperature, time, and pressure ensures effective sterilization of most microorganisms, including bacteria, viruses, and fungi.
The other options are incorrect:
- 130°C for 30min at 30 p.s.i.: This setting, while potentially effective for sterilization, is generally not the standard for most autoclaves. Higher temperatures and pressures are typically reserved for specific purposes like prion decontamination or for specific types of equipment that can withstand the harsher conditions.
- 121°C for 50min at 6 p.s.i.: While the temperature here is within the standard range, the lower pressure (6 psi) and longer time (50 minutes) are not typical for efficient sterilization cycles. Standard cycles prioritize shorter times while maintaining sufficient pressure and temperature for effective microbial killing.
- Pus cells or fat in urine would cause this color:
- red
- yellow-brown
- greenish-blue
- milky-white
Answer and Explanation
Answer: milky-white
Pus, which is a collection of white blood cells and dead tissue, can cause urine to appear milky-white or cloudy. This is due to the high concentration of white blood cells and other cellular debris in the urine.
The other options are incorrect:
- Red: Red urine can be caused by blood in the urine, also known as hematuria. This can be due to various factors like urinary tract infections, kidney stones, or certain medications.
- Yellow-brown: This is the typical color of normal urine and can vary depending on hydration levels. Dehydration can lead to darker yellow urine, while increased fluid intake can make it lighter.
- Greenish-blue: While uncommon, greenish-blue urine can occur due to certain medications, infections with specific bacteria like Pseudomonas, or high levels of bilirubin in the blood (which can happen in liver diseases).
- Which statement is true regarding the use of reagent dipsticks:
- timing of each reagent area is not necessary
- reagent sticks are held vertically when reading
- all reagent sticks tests do specific gravity
- reagent strips should be tested daily with control
Answer and Explanation
Answer: reagent strips should be tested daily with control
Daily quality control testing with a control solution ensures the accuracy and reliability of reagent strip results. This helps identify potential issues with the strips themselves or the testing procedure.
The other options are incorrect:
- Timing of each reagent area is not necessary: Each test area on a reagent strip has a specific timeframe for color development. Reading the results too early or too late can lead to inaccurate interpretations.
- Reagent sticks are held vertically when reading: Reagent strips are typically read horizontally compared to a color chart provided by the manufacturer. Holding them vertically can cause color variations due to uneven liquid distribution.
- All reagent sticks test specific gravity: While some reagent strips may include a test for specific gravity, it’s not a universal feature.
- A 1/8 dilution of urine is:
- 1-part water and 8 parts urine
- 1-part urine and 8 parts water
- 1-part urine and 7 parts water
- 1-part water and 7 parts urine
Answer and Explanation
Answer: 1-part urine and 7 parts water
A 1/8 dilution of urine means that 1 part of urine is mixed with 7 parts of water. This ratio represents the proportion of the original solution (urine) to the diluent (water) in the dilution process.
The other options are incorrect:
- 1-part water and 8 parts urine: This is not the correct dilution. A 1/8 dilution means there are more parts of water than urine.
- 1-part urine and 8 parts water: This is not the correct dilution. A 1/8 dilution means there are more parts of water than urine.
- 1-part urine and 7 parts water: This is the correct dilution. It represents a 1/8 dilution where there is 1 part urine and 7 parts water.
- Before performing an R & M on a specimen, the urine would be;
- brought to room temperature
- well-mixed
- filtered
- Both brought to room temperature and well-mixed
Answer and Explanation
Answer: Option brought to room temperature and well-mixed
Before performing a Routine and Microscopic (R & M) examination on a urine specimen, it is recommended to bring the urine to room temperature and ensure it is well-mixed. Bringing the urine to room temperature and thorough mixing help in obtaining a representative and accurate analysis of the urine’s components.
The other options are incorrect:
- Filtered: While filtering might be used in specific situations, it’s generally not a routine step before performing an R&M on a urine sample. Filtering can remove some cells, potentially affecting the accuracy of the cell count. Additionally, R&M tests are designed to analyze both intact cells and some cellular debris, and filtering might remove this relevant information.
- A backup test(s) to confirm a positive protein in urine would be:
- SSA test
- TCA test
- ictotest
- Both SSA test and TCA test
Answer and Explanation
Answer: Both SSA test and TCA test
To confirm a positive protein result in urine, a backup test can be performed using the SSA (Sulfosalicylic acid) test and the TCA (Trichloroacetic acid) test. These tests are used to verify the presence of protein by causing precipitation, helping to confirm the initial positive protein finding.
The other options are incorrect:
- Ictotest: The Ictotest is used for the detection of bilirubin in urine, not for confirming protein. It is not a suitable backup test for protein confirmation.
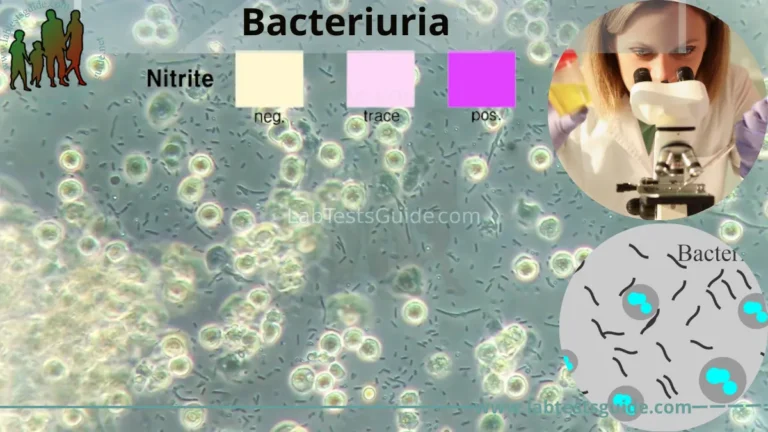
- Which test result would increase in a urine specimen sitting at room temperature for 3 hours:
- bilirubin
- nitrite
- leukocyte
- urobilinogen
Answer and Explanation
Answer: nitrite
Nitrite is a byproduct of the nitrate reduction pathway used by certain bacteria, particularly gram-negative bacteria like Escherichia coli (E. coli), a common culprit in urinary tract infections (UTIs). When a urine sample containing these bacteria sits at room temperature, they may continue to metabolize nitrates present in the urine, leading to an increase in nitrite levels.
The other options are incorrect:
- Bilirubin: Bilirubin levels in urine are not typically affected by storage time at room temperature for short periods like 3 hours.
- Leukocyte: Leukocyte (white blood cell) count in urine might decrease slightly over time due to cell degeneration, but it’s unlikely to show a significant increase within 3 hours at room temperature.
- Urobilinogen: Similar to bilirubin, urobilinogen levels in urine are not expected to change significantly within a short storage time at room temperature.
- What is the color of Gram Positive Bacteria in gram stain ?
- Pink
- Purple
- Green
- None
Answer and Explanation
Answer: Purple
In the Gram staining technique, Gram-positive bacteria appear purple under a microscope. This is due to their thicker peptidoglycan cell wall, which retains the crystal violet stain used in the first step of the procedure.
The other options are incorrect:
- Pink: This color is typically associated with Gram-negative bacteria, which have a thinner peptidoglycan layer and are decolorized with an alcohol-acetone solution, subsequently taking up the counterstain (safranin) and appearing pink.
- Green: Green is not a typical color observed in Gram staining. It’s possible for bacteria to exhibit various colors depending on specific techniques or dyes used, but in the standard Gram stain, green wouldn’t be indicative of either Gram-positive or Gram-negative bacteria.
- None: Bacteria would appear in some color under a microscope after staining, and the Gram stain specifically differentiates them into purple (Gram-positive) and pink (Gram-negative) based on their cell wall structure.
- Which media is commonly used for fungle culture ?
- SDA
- Blood Culture
- Nutrient agar
- Chocolate Agar
Answer and Explanation
Answer: SDA
Sabouraud Dextrose Agar (SDA) is commonly used for fungal culture. This specialized medium provides an environment that supports the growth of fungi while inhibiting the growth of bacteria. It typically contains dextrose and agar as nutrients for fungal growth.
The other options are incorrect:
- Blood Culture: This medium is specifically formulated for the growth of bacteria present in the bloodstream and is not suitable for fungal culture.
- Nutrient agar: While this general-purpose medium can support the growth of some fungi, it’s not as selective or optimal for fungal growth compared to SDA.
- Chocolate agar: This enriched medium is primarily used for the growth of fastidious bacteria (those requiring specific growth conditions) and is not suitable for routine fungal culture.
- Best medium for urine culture ?
- Blood Agar
- Nutrient Agar
- CLED Agar
- Chocolate Agar
Answer and Explanation
Answer: CLED Agar
CLED (Cystine Lactose Electrolyte Deficient) Agar is commonly used for urine culture. It is a selective and differential medium that supports the growth of urinary bacteria while inhibiting the swarming of Proteus species. CLED Agar helps in the isolation and identification of urinary tract pathogens.
The other options are incorrect:
- Blood Agar: Blood Agar is a general-purpose medium that supports the growth of a wide range of microorganisms, including both bacteria and fungi. However, it is not specifically designed for urine culture.
- Nutrient Agar: Nutrient Agar is a general-purpose medium that supports the growth of various microorganisms but is not selective for urinary pathogens. It is not commonly used for urine culture.
- Chocolate Agar: Chocolate Agar is an enriched medium used for the cultivation of fastidious bacteria, especially Haemophilus influenzae. It is not specifically designed for urine culture.
- Which stain used for capsule ?
- India ink
- Negative Stain
- India ink & Negative Stain Both
- Crystal Violet
Answer and Explanation
Answer: India ink & Negative Stain Both
Both India ink and Negative Stain techniques are commonly used for the visualization of bacterial capsules. These staining methods do not stain the capsules but create a contrast between the capsule and the background, making the capsules visible under the microscope.
The other options are incorrect:
- Crystal Violet: Crystal Violet is not typically used for capsule staining. It is a primary stain in the Gram stain procedure and is not suitable for highlighting bacterial capsules.
- Negative Stain: This is part of the correct answer. Negative staining techniques, such as using Congo red or Nigrosin, are used for capsule visualization by creating a dark background around the capsules.
- India Ink: This is part of the correct answer. India ink is a common method for capsule staining, as it does not penetrate the capsule but surrounds it, making the capsule visible against the dark background.
- Which Stain is Not a category of Romanaworasky ?
- Giemsa Stain
- Wright’s Stain
- Leishman Stain
- ZN Stain
Answer and Explanation
Answer: ZN Stain
While all the other options are Romanowsky stains or closely related, ZN Stain (Ziehl-Neelsen Stain) is a different staining technique used specifically for identifying acid-fast bacteria like Mycobacterium tuberculosis, the causative agent of tuberculosis.
The other options are incorrect:
- Giemsa stain: A commonly used Romanowsky stain for staining blood films, tissue sections, and other biological samples.
- Wright’s stain: A modification of the Romanowsky stain, often used for peripheral blood smears to differentiate various types of blood cells.
- Leishman stain: Another Romanowsky stain used for blood films and other samples, particularly useful for parasites and protozoa.
- Widal Test Use for Which Organism ?
- Salmonella
- Vibrio Cholera
- Staphylococcus
- Shigella
Answer and Explanation
Answer: Salmonella
The Widal test is used for the detection of antibodies against Salmonella bacteria. It is a serological test that helps in the diagnosis of typhoid fever and other infections caused by Salmonella species.
The other options are incorrect:
- Vibrio Cholera: The Widal test is not used for Vibrio cholera. Vibrio cholera is associated with cholera, and different diagnostic methods are employed for detecting this organism.
- Staphylococcus: The Widal test is not used for Staphylococcus. Staphylococcus is a different genus of bacteria, and the Widal test is specific to Salmonella.
- Shigella: The Widal test is not used for Shigella. Shigella is a different genus of bacteria, and the Widal test is designed for the detection of antibodies against Salmonella.
- 121°C for 15 mint in Sterilization for ?
- Hot air oven
- Water Bath
- Autoclave
- Incubator
Answer and Explanation
Answer: Autoclave
An autoclave is a specialized device that uses steam under pressure to achieve sterilization, typically at a temperature of 121°C (250°F) for 15 minutes. This combination of high temperature and pressure effectively kills microorganisms, including bacteria, viruses, and fungi.
The other options are incorrect:
- Hot air oven: While hot air ovens can be used for sterilization at lower temperatures (typically around 160-180°C), they are not as effective as autoclaves for killing highly resistant microorganisms due to the lack of pressure and lower temperatures used.
- Water bath: Water baths are not typically used for sterilization. They are commonly used for temperature-controlled incubation or warming of solutions but do not provide the high-temperature, high-pressure conditions necessary for sterilization.
- Incubator: Incubators are designed to provide a controlled environment with specific temperature and humidity conditions for growing microorganisms, not for sterilization.
- Candle Jar Method used for ?
- Aerobic Bacteria
- Anaerobic Bacteria
- 1 & 2 Both
- Capnophilic Bacteria
Answer and Explanation
Answer: Aerobic Bacteria
The candle jar method is a low-cost and simple technique used to create an anaerobic environment for cultivating anaerobic bacteria. These bacteria require an environment devoid of oxygen for growth and survival.
The other options are incorrect:
- Aerobic Bacteria: Aerobic bacteria require oxygen for their growth and cannot survive in an anaerobic environment created by the candle jar method.
- Capnophilic Bacteria: While capnophilic bacteria thrive in environments with increased carbon dioxide (CO2) compared to the atmosphere, they can still tolerate some oxygen and wouldn’t necessarily require the strictly anaerobic environment created by the candle jar method.
- 1 & 2 Both: The candle jar method is specifically used for anaerobic bacteria, not for both aerobic and anaerobic bacteria.
- Bacteria Having Flagella All over the body called as ?
- Monotrichous
- Peritrichous
- Lophotrichous
- Amphitrichous
Answer and Explanation
Answer: Peritrichous
Bacteria with flagella distributed over their entire body are called peritrichous. This term comes from the Greek words “peri” meaning “around” and “trichos” meaning “hair,” referring to the hair-like flagella surrounding the bacterial cell.
The other options are incorrect:
- Monotrichous: Bacteria with a single flagellum at one end.
- Lophotrichous: Bacteria with a tuft of flagella at one or both ends.
- Amphitrichous: Bacteria with a single or multiple flagella at both ends.
- Metachromatic granules associated with ?
- Clostridium
- Staphylococcus
- Corynebacterium
- Vibrio
Answer and Explanation
Answer: Corynebacterium
Metachromatic granules are associated with Corynebacterium species. These granules are composed of a polymer called metachromatic granule phosphate (also known as volutin or polyphosphate). Corynebacterium diphtheriae, for example, is a bacterium known for containing metachromatic granules.
The other options are incorrect:
- Clostridium: Metachromatic granules are not typically associated with Clostridium species. Clostridia are known for their ability to form endospores, but metachromatic granules are not a characteristic feature.
- Staphylococcus: Staphylococcus species do not typically contain metachromatic granules. Staphylococci are Gram-positive bacteria, and their characteristics differ from those of Corynebacterium.
- Vibrio: Metachromatic granules are not associated with Vibrio species. Vibrio bacteria are known for their curved shape and may possess polar flagella, but they do not exhibit metachromatic granules.
- Which of the following is not a DNA Virus ?
- Adenoviridae
- Poxviridae
- Papovaviridae
- Orthomyxoviridae
Answer and Explanation
Answer: Orthomyxoviridae
While all the other options listed belong to the category of DNA viruses, Orthomyxoviridae is a family of RNA viruses. They are known for containing single-stranded, negative-sense RNA as their genetic material.
The other options are incorrect:
- Adenoviridae: This family includes viruses like adenoviruses, which cause respiratory illnesses and conjunctivitis. They are classified as DNA viruses.
- Poxviridae: This family includes viruses like the variola virus (smallpox) and vaccinia virus (used in the smallpox vaccine). They are also classified as DNA viruses.
- Papovaviridae: This family includes viruses like human papillomavirus (HPV) and simian virus 40 (SV40). They are classified as DNA viruses.
- Which of the following is not a florescent dyes ?
- Auramine
- Calcoflour
- Rhodamine
- Methylene blue
Answer and Explanation
Answer: Methylene blue
Methylene Blue is not a fluorescent dye. It is a common biological stain used in microbiology for general staining purposes but does not exhibit fluorescence under UV light.
The other options are incorrect:
- Auramine: Auramine is a fluorescent dye commonly used in fluorescence microscopy, particularly for the detection of acid-fast bacteria.
- Calcofluor: Calcofluor is a fluorescent brightener and is used for the detection of fungal elements, cellulose, and chitin. It is widely employed in fluorescence microscopy.
- Rhodamine: Rhodamine is a group of fluorescent dyes frequently used in various applications, including fluorescence microscopy and flow cytometry, for labeling biological specimens.
- True about malarial capsule following except ?
- Lost by repeated subculture
- Stain by Gram stain
- Protect bacteria by lytic enzymes
- Prevent phagocytosis
Answer and Explanation
Answer: Stain by Gram stain
The statement “Stain by Gram stain” is incorrect regarding malarial capsules. Malarial parasites, such as Plasmodium species, do not have a typical Gram-negative or Gram-positive bacterial cell wall, and their structures do not stain with the Gram stain.
The other options are incorrect:
- Lost by repeated subculture: Capsules can be lost by repeated subculture as the process may select for strains that do not produce capsules.
- Protect bacteria by lytic enzymes: Capsules can help protect bacteria from the action of lytic enzymes by acting as a physical barrier.
- Prevent phagocytosis: Capsules are known for preventing phagocytosis by immune cells. They create a slippery layer that makes it difficult for phagocytes to engulf the bacterial cells.
- Which anticoagulant present in blood culture bottle ?
- SPS
- Heparin
- Doubal Oxalate
- None of above
Answer and Explanation
Answer: SPS
Sodium Polyanetholesulfonate (SPS) is the most commonly used anticoagulant in blood culture bottles. It works by preventing the formation of blood clots, allowing for even distribution of the blood sample throughout the culture medium and facilitating the growth of any potential microorganisms present.
The other options are incorrect:
- Heparin: While heparin is a common anticoagulant used in various clinical settings, it’s typically not used in blood culture bottles due to its potential effects on certain bacteria and their growth.
- Double Oxalate: Sodium oxalate and potassium oxalate are sometimes used as anticoagulants in specific situations, but they are not the preferred choice for blood cultures due to their potential inhibitory effects on some bacteria.
- None of the above: As explained earlier, an anticoagulant is essential in blood culture bottles to prevent clotting and allow for microbial growth detection. SPS is the most commonly used option for this purpose.
- Antimicrobial agent that kill the bacteria are called ?
- Bacteriostatic
- Antibiotic
- Bacteriocidal
- Bacterial Killer
Answer and Explanation
Answer: Bacteriocidal
Antimicrobial agents that kill bacteria are called bacteriocidal. These agents have the ability to directly kill bacterial cells, leading to their death.
The other options are incorrect:
- Bacteriostatic: Bacteriostatic agents inhibit the growth and reproduction of bacteria without necessarily causing their death. They create conditions that prevent further bacterial multiplication.
- Antibiotic: Antibiotics are a broad category of antimicrobial agents that can be either bacteriostatic or bacteriocidal. The term “antibiotic” does not specifically imply killing; it refers to substances that can inhibit or kill bacteria.
- Bacterial Killer: This is a colloquial term. While it conveys the idea of killing bacteria, the more precise term used in microbiology is “bacteriocidal.”
- In Florescent mocroscope, what is used ?
- Electrone beam
- U.V Rays
- Simple light
- Sunlighte
Answer and Explanation
Answer: U.V Rays
In a fluorescence microscope, ultraviolet (UV) rays are used to excite fluorescent molecules in the sample. These excited molecules then emit light at a longer wavelength, which is visible through the eyepieces of the microscope. This allows for the visualization of specific structures or substances within the sample that may not be readily visible under normal light microscopy.
The other options are incorrect:
- Electron beam: Electron beams are used in electron microscopes, not fluorescence microscopes.
- Simple light: While some fluorescence microscopes may have a setting for transmitted light observation, the defining characteristic of a fluorescence microscope is the use of UV light to excite fluorophores.
- Sunlight: Sunlight is not a controlled light source and contains a broad spectrum of wavelengths, including UV rays. However, it’s not typically used in fluorescence microscopy due to its lack of control and potential safety concerns.
- What indicate if report say retrovirus positive ?
- Herpes
- HIV
- Hepatitis
- Robies
Answer and Explanation
Answer: HIV
If a report indicates “retrovirus positive,” it typically refers to the detection of a retrovirus, and one of the well-known retroviruses in humans is HIV (Human Immunodeficiency Virus). HIV is the virus that causes acquired immunodeficiency syndrome (AIDS).
The other options are incorrect:
- Herpes: While herpes simplex virus (HSV) and varicella-zoster virus (VZV) are both viruses, they belong to the Herpesviridae family, not the Retroviridae family, which includes HIV. Therefore, a “retrovirus positive” report wouldn’t indicate the presence of herpes.
- Hepatitis: Hepatitis refers to inflammation of the liver, often caused by viruses. However, several different viruses can cause hepatitis, including hepatitis A, B, and C, which are not retroviruses. A “retrovirus positive” report wouldn’t necessarily indicate any specific type of hepatitis.
- Robies: This is likely a misspelling of “Rubies,” which is not a virus or a medical term.
- Peplomers present on which site in virus ?
- Nucleic acid
- Envelope
- Capsid
- Nucleocapsid
Answer and Explanation
Answer: Envelope
Peplomers, also known as spikes or glycoproteins, are present on the envelope of a virus. These structures play a crucial role in the attachment of the virus to host cells and in the entry of the virus into host cells.
The other options are incorrect:
- Nucleic acid: The nucleic acid of a virus is its genetic material, either DNA or RNA, and it is located inside the capsid or nucleocapsid, not on the surface where peplomers are found.
- Capsid:The capsid is the protein coat surrounding the nucleic acid of a virus. While it provides protection to the genetic material, peplomers are not located on the capsid.
- Nucleocapsid: The nucleocapsid is a complex formed by the combination of the nucleic acid and the capsid. Peplomers are typically found on the envelope, not on the nucleocapsid itself.
- What do you mean by polyuria ?
- Increase amount of urea
- Increase amount of Uric Acid
- Increase amount of Urine
- Increase amount of urea in Urine
Answer and Explanation
Answer: Increase amount of Urine
Polyuria refers to the condition characterized by an abnormally increased volume of urine production. It is often associated with an increase in the frequency and quantity of urination.
The other options are incorrect:
- Increase amount of urea: While urea is a waste product excreted in urine, polyuria specifically refers to the volume of urine, not the concentration of specific components.
- Increase amount of Uric Acid: Similar to urea, uric acid is another waste product eliminated through urine. However, increased uric acid levels are associated with gout, not necessarily polyuria.
- Increase amount of urea in Urine: This statement is partially true, as urine does contain urea. However, polyuria focuses on the overall volume, not the specific components present in the urine.
- Mycobacterium laprae resist decolourization from ?
- 20% Sulphuric acid
- 5% Sulphuric acid
- 25% Sulphuric acid
- 3% Sulphuric acid
Answer and Explanation
Answer: 5% Sulphuric acid
Mycobacterium leprae, the causative agent of leprosy, is known to resist decolorization during acid-fast staining procedures. The acid-fast stain, such as the Ziehl-Neelsen stain or the Fite-Faraco stain, involves the use of strong acids to remove the stain from non-acid-fast bacteria, leaving the acid-fast organisms (like Mycobacterium leprae) stained.
The other options are incorrect:
- 20% Sulphuric acid: This concentration is higher than the typically used concentration in acid-fast staining procedures and may lead to excessive decolorization of acid-fast bacteria.
- 25% Sulphuric acid: This concentration is higher than the commonly used concentration and may result in over-decolorization, affecting the staining of Mycobacterium leprae.
- 3% Sulphuric acid: This concentration is lower than the commonly used concentration in acid-fast staining procedures and may not effectively decolorize non-acid-fast bacteria, leading to false-positive results.
- Dick test is assosiated with ?
- Staphylococus albus
- Streptococci pyogenes
- Streptococci Viridance
- Staphylococus Aureus
Answer and Explanation
Answer: Streptococci pyogenes
The Dick test was developed specifically to determine susceptibility to scarlet fever, which is caused by Streptococcus pyogenes bacteria. This test involved injecting a diluted toxin produced by S. pyogenes and observing the skin reaction. A positive reaction indicated susceptibility to the disease.
The other options are incorrect:
- Staphylococcus albus: This bacteria is not typically associated with scarlet fever and wouldn’t give a positive Dick test.
- Streptococcus Viridans: This group of bacteria encompasses various species, some of which can cause minor infections but are not linked to scarlet fever.
- Staphylococcus aureus: While S. aureus is a common pathogen, it doesn’t cause scarlet fever and wouldn’t be detected by the Dick test.
- Flaming is done in following for sterilization except ?
- Glass Slides
- Mouth of tubes
- Forceps
- Flask Mouth
Answer and Explanation
Answer: Flask Mouth
Flaming is a method of sterilization using an open flame to kill or remove microorganisms from surfaces. However, the flask mouth is typically not flamed directly, as the intense heat could crack or damage the glass. Instead, the mouth of flasks is usually covered with a sterile cotton plug or aluminum foil, and the flaming is applied to items like glass slides, tubes, and forceps.
The other options are incorrect:
- Glass Slides: These are often sterilized by flaming, especially when used for preparing bacterial smears.
- Mouth of tubes: Similar to inoculation loops, the mouth of tubes containing culture media or samples is frequently sterilized by flaming.
- Forceps: As mentioned earlier, flaming is a common method to sterilize forceps used in microbiology practices.
- What is correct order for bacteria growth ?
- Log, Lag, Stationary, decline
- Lag, Stationary, Log, Decline
- Lag, Log, Stationary, Decline
- Log, Lag, Decline, Stationary
Answer and Explanation
Answer: Lag, Log, Stationary, Decline
Bacterial growth follows a predictable pattern with four distinct phases:
- Lag phase: Following introduction into a new environment, bacteria adapt and synthesize essential molecules before actively dividing. This initial lag in growth is reflected in the name.
- Log (exponential) phase: This is the phase of rapid and exponential cell division. The bacterial population increases at its fastest rate during this stage.
- Stationary phase: As nutrients become depleted and waste products accumulate, the growth rate slows down. The number of dividing cells equals the number dying, leading to a stable population size.
- Decline phase: With continued resource depletion and waste accumulation, the bacterial population begins to decline as the death rate exceeds the division rate.
The other options are incorrect:
- Log, Lag, Stationary, decline: This order is incorrect because the lag phase always precedes the exponential growth (log phase).
- Lag, Stationary, Log, Decline: This is incorrect as the stationary phase wouldn’t occur before the log phase where the population actively grows.
- Log, Lag, Decline, Stationary: This sequence disrupts the natural progression. The lag phase precedes the log phase, and the decline phase follows the stationary phase, not vice versa.
- Who is known as ‘father of microbiology’
- Louis Pasteur
- Robert Koch
- Alexander Fleming
- Edward Jenner
Answer and Explanation
Answer: Louis Pasteur
Louis Pasteur is known as the “father of microbiology.” He made significant contributions to the field, including the development of the germ theory of disease, the process of pasteurization, and the development of vaccines for diseases such as rabies.
The other options are incorrect:
- Robert Koch: Robert Koch made important contributions to microbiology, including the identification of specific bacteria causing diseases (Koch’s postulates), but he is not referred to as the “father of microbiology.”
- Alexander Fleming: Alexander Fleming discovered penicillin, the first antibiotic, which was a crucial development in medicine. However, he is not considered the “father of microbiology.”
- Edward Jenner: Edward Jenner is known for developing the smallpox vaccine, a significant contribution to immunology, but he is not considered the “father of microbiology.”
- All the following are motile bacteria except
- E.Coli
- Klebsiella
- Vibrio
- Proteus
Answer and Explanation
Answer: Klebsiella
Klebsiella is a non-motile bacterium. Unlike Escherichia coli (E. coli), Vibrio, and Proteus, which are motile bacteria and have structures like flagella for movement, Klebsiella lacks flagella and is generally non-motile.
The other options are incorrect:
- E. Coli: Escherichia coli (E. coli) is a motile bacterium that possesses flagella, allowing it to move in liquid environments.
- Vibrio: Vibrio species, such as Vibrio cholerae, are motile bacteria with a curved shape and polar flagella, enabling them to move in liquid environments.
- Proteus: Proteus species are highly motile bacteria with a unique swarming ability. They exhibit rapid movement, often associated with their flagellar structure.
- Solidifying agent of a culture media is
- peptone
- meat extract
- sodium chloride
- agar
Answer and Explanation
Answer: agar
Agar is the solidifying agent commonly used in culture media. It is a gelatinous substance derived from seaweed and is added to liquid media to solidify it. Agar provides a solid surface for the growth of microorganisms and allows for the isolation and study of individual colonies.
The other options are incorrect:
- Peptone: This is a complex mixture of proteins and amino acids that serves as a nutrient source for bacteria in the culture media, not a solidifying agent.
- Meat extract: Similar to peptone, meat extract is another source of nutrients, providing essential components for bacterial growth, but doesn’t contribute to solidification.
- Sodium chloride: While sodium chloride (table salt) can play a role in maintaining the osmotic pressure of the media and can sometimes be used to differentiate between bacterial species based on their tolerance, it doesn’t have gelling properties and cannot solidify the media.
- ____is added to Mac Conkeys agar to inhibit the growth of gram positive bacteria.
- Bile salt
- Peptone
- Neutral red
- Agar
Answer and Explanation
Answer: Bile salt
Bile salt is added to MacConkey agar to inhibit the growth of Gram-positive bacteria. MacConkey agar is a selective and differential medium primarily used for the isolation and differentiation of Gram-negative enteric bacteria based on their ability to ferment lactose.
The other options are incorrect:
- Peptone: This is a complex mixture of proteins and amino acids that serves as a nutrient source for various bacteria, including both gram-positive and gram-negative, and doesn’t inhibit their growth.
- Neutral red: While this dye plays a crucial role in differentiating lactose-fermenting and non-fermenting bacteria by changing color based on the pH, it doesn’t have any inhibitory properties towards bacterial growth.
- Agar: As mentioned previously, agar is the solidifying agent present in the media and doesn’t contribute to selective inhibition of any bacterial group.
- All the following are examples of transport media except
- VR medium
- Thioglycollate medium
- Stuarts medium
- Amies medium
Answer and Explanation
Answer: VR medium
VR medium, or viral transport medium, specifically supports the survival and viability of viruses during transport to a laboratory for testing. Thioglycollate, Stuart’s, and Amies media are all designed for bacterial and fungal cultures, not viruses.
The other options are incorrect:
- Thioglycollate medium:Supports the growth of a wide range of bacteria, including both aerobic and anaerobic types. It is commonly used for blood cultures.
- Stuart’s medium:Enriched transport medium used for the collection and transportation of various clinical specimens suspected to contain bacteria, especially Neisseria and Haemophilus species.
- Amies medium: Universal transport medium used for collecting and transporting various clinical specimens for bacterial and fungal cultures. It contains ingredients to maintain the viability of the organisms and suppress the growth of contaminating flora.
- All the following are examples of transport media except
- VR medium
- Thioglycollate medium
- Stuarts medium
- Amies medium
Answer and Explanation
Answer: Thioglycollate medium
While all the listed options are transport media used for various purposes, thioglycollate medium specifically supports the growth of a wide range of microorganisms, including both aerobic and anaerobic bacteria. This makes it ideal for transporting and culturing a diverse range of potential pathogens from clinical samples.
The other options are incorrect:
- VR medium (Vancomycin Reistance medium): This medium is selective, meaning it is designed to inhibit the growth of certain bacteria while allowing specific resistant strains to grow. This makes it unsuitable for general transport purposes where a wide range of microorganisms might be present.
- Stuarts medium: This is a transport medium specifically used for transporting and isolating Neisseria species, such as Neisseria gonorrhoeae (the cause of gonorrhea). While it is a transport medium, its limited application excludes it from being a general transport medium for various types of samples.
- Amies medium: This is a universal transport medium, similar to thioglycollate, used for collecting and transporting a wide range of clinical specimens. It is designed to maintain the viability of various bacteria during transport to the laboratory for further analysis.
- Which of the following tests come under IMViC tests ?
- Coagulase test
- Catalase test
- Citrate utilisation test
- None of above
Answer and Explanation
Answer: Citrate utilisation test
The IMViC test stands for Indole, Methyl Red, Voges-Proskauer, and Citrate utilization tests. These are a series of biochemical tests used to differentiate between various Enterobacteriaceae, a family of Gram-negative bacteria that includes common pathogens like Escherichia coli and Salmonella enterica. The Citrate utilization test specifically assesses a bacterium’s ability to utilize citrate as a sole carbon source for growth.
The other options are incorrect:
- Coagulase test: This test identifies bacteria that produce the enzyme coagulase, which can clot plasma. It is used to differentiate between Staphylococcus aureus (positive test) and other Staphylococcus species (negative test).
- Catalase test: This test detects the presence of the enzyme catalase, which breaks down hydrogen peroxide into water and oxygen. It is a general test used to differentiate between aerobic and anaerobic bacteria.
- The bacteria which require ‘X’ and ‘V’ factors for its growth is
- staphylococcus
- haemophilus
- brucella
- salmonella
Answer and Explanation
Answer: haemophilus
Haemophilus species, particularly Haemophilus influenzae, require both “X” and “V” factors for growth. The “X” factor is typically hemin or protoporphyrin IX, which is an essential component for their cytochrome system. The “V” factor is nicotinamide adenine dinucleotide (NAD) or nicotinamide adenine dinucleotide phosphate (NADP), which are coenzymes crucial for various metabolic processes.
The other options are incorrect:
- Staphylococcus: Most Staphylococcus species are not dependent on “X” and “V” factors for growth. They are generally auxotrophic for some vitamins and amino acids, but they can synthesize their own heme and NAD.
- Brucella: Brucella species are also not dependent on “X” and “V” factors. They have all the necessary enzymes to synthesize their own heme and NAD.
- Salmonella: While Salmonella does require some specific nutrients for growth, “X” and “V” factors are not essential for their survival. They can synthesize these components themselves.
- ‘Mycology’ means the study of
- bacteria
- immunity
- parasites
- fungus
Answer and Explanation
Answer: fungus
Mycology is the branch of biology specifically dedicated to the study of fungi, including their taxonomy, structure, physiology, ecology, and impact on human health and the environment. Fungi are a diverse group of eukaryotic organisms distinct from bacteria, plants, and animals.
The other options are incorrect:
- Bacteria: Bacteriology is the field of study focused on bacteria, including their characteristics, growth, and role in disease.
- Immunity: Immunology is the branch of biology concerned with the immune system, the body’s defense mechanism against pathogens like bacteria, viruses, and fungi.
- Parasites: Parasitology focuses on the study of parasites, organisms that live on or in another organism (host) and obtain nutrients from it. While some fungi can be parasitic, mycology encompasses a broader range of fungal forms and functions beyond parasitism.
- The bacteria showing swarming growth is
- E.coli
- Salmonella
- Proteus
- All the above
Answer and Explanation
Answer: Proteus
The bacteria that typically exhibit swarming growth on solid agar surfaces are members of the genus Proteus. Swarming is a type of rapid and coordinated multicellular movement across a surface, and Proteus species are known for this characteristic.
The other options are incorrect:
- E. coli: Escherichia coli (E. coli) does not typically exhibit swarming growth. E. coli colonies on solid media are usually more discrete.
- Salmonella: Salmonella species do not generally display swarming growth. They have different characteristics in terms of colony morphology on solid agar.
- All the above: The correct answer is Proteus. While E. coli and Salmonella do not commonly show swarming growth, Proteus species are known for this behavior.
- The resolution of an Electron microscope is expressed in
- Millimeters
- Micrometers
- Nanometers
- Centimeters
Answer and Explanation
Answer: Nanometers
The resolution of an electron microscope, which refers to its ability to distinguish between two closely spaced points, is measured in nanometers (nm). This is because the wavelength of electrons used in electron microscopy is significantly smaller than the wavelength of visible light used in light microscopes. Smaller wavelengths allow for resolving finer details, hence the use of nanometers in electron microscopy.
The other options are incorrect:
- Millimeters (mm): Millimeters are too large a unit for measuring the resolution of an electron microscope. They are typically used for macroscopic objects visible to the naked eye.
- Micrometers (µm): While some biological structures are measured in micrometers, electron microscopes can achieve much higher resolutions, reaching the realm of nanometers.
- Centimeters (cm): Similar to millimeters, centimeters are even larger units unsuitable for expressing the resolution of an electron microscope.
- TORCH infections are best analysed by
- Capture ELISA
- Competitive ELISA
- Immuno capture ELISA
- Streptavidin-Biotin ELISA
Answer and Explanation
Answer: Capture ELISA
TORCH infections (Toxoplasmosis, Other agents, Rubella, Cytomegalovirus, and Herpes simplex) are best analyzed using Capture ELISA (Enzyme-Linked Immunosorbent Assay). In Capture ELISA, a specific antibody is immobilized on the solid phase to capture and detect antigens related to TORCH infections.
The other options are incorrect:
- Competitive ELISA: Competitive ELISA is not typically used for the analysis of TORCH infections. It involves competition between labeled and unlabeled antigens for binding to a limited number of antibody sites.
- Immuno capture ELISA: Immuno capture ELISA is not the most common method for analyzing TORCH infections. In immuno capture ELISA, an immobilized antibody captures an antigen, similar to Capture ELISA.
- Streptavidin-Biotin ELISA: Streptavidin-Biotin ELISA involves the use of streptavidin and biotin for signal amplification and detection. It is not the preferred method for analyzing TORCH infections, which is better suited for Capture ELISA.
The questions are typically designed to assess the technical skills and knowledge required for the laboratory profession, including the ability to analyze laboratory test results, perform laboratory procedures, and maintain laboratory equipment.
To prepare for these MCQs, candidates should have a thorough understanding of the key concepts and principles of laboratory science. They should also be familiar with common laboratory equipment and procedures, as well as laboratory safety protocols.
Candidates may also benefit from studying specific laboratory science textbooks or taking online courses that cover the material tested in the MCQs. Additionally, practicing sample MCQs and reviewing the answers can help candidates identify areas where they may need to improve their knowledge or skills.
Overall, the MCQs for lab technologists are designed to be challenging and comprehensive, requiring candidates to demonstrate a high level of proficiency in the field of laboratory science.