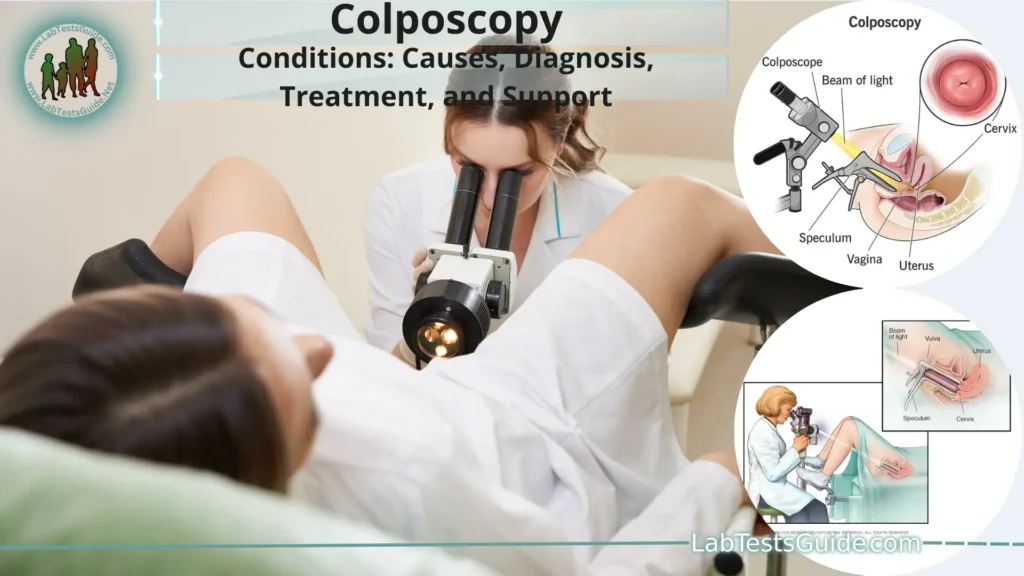
Colposcopy is a medical procedure used to closely examine the cervix, vagina, and vulva in order to identify any abnormalities or signs of disease, particularly in cases where a Pap smear or other tests have indicated potential issues. It is typically performed by a gynecologist or other healthcare provider who specializes in women’s reproductive health.
Definition of Colposcopy.
Colposcopy is a medical procedure that involves the visual examination and magnified inspection of the cervix, vagina, and vulva using a specialized instrument called a colposcope. This procedure allows healthcare providers, often gynecologists, to closely assess the tissues for any abnormalities, such as precancerous or cancerous changes, as well as other conditions that might be affecting these areas. By providing a detailed and enhanced view of the tissues, colposcopy assists in the early detection, diagnosis, and management of various gynecological conditions. It is commonly performed when there are abnormal Pap smear results, unexplained vaginal bleeding, or other indications of potential health issues. If abnormal areas are identified during the procedure, further diagnostic steps or treatments, such as biopsies or tissue removal, may be recommended based on the findings.
When and Why Colposcopy is Used:
Here are the common scenarios in which colposcopy is used and why.
- Abnormal Pap Smear Results: If a woman’s Pap smear (Pap test) results show abnormal cells, such as atypical squamous cells of undetermined significance (ASCUS), low-grade squamous intraepithelial lesions (LSIL), or high-grade squamous intraepithelial lesions (HSIL), a colposcopy may be recommended. The colposcopy helps determine the extent and severity of the abnormalities.
- HPV (Human Papillomavirus) Infection: Human papillomavirus is a common sexually transmitted infection that can lead to cervical changes and increase the risk of cervical cancer. If a woman tests positive for high-risk HPV types, particularly if accompanied by abnormal Pap smear results, colposcopy might be advised.
- Unexplained Vaginal Bleeding: Persistent or irregular vaginal bleeding that is not related to menstruation might prompt a colposcopy. This is done to investigate the cause of the bleeding and identify any underlying issues.
- Visible Abnormalities: If a healthcare provider identifies visible abnormalities during a pelvic exam, such as lesions, ulcers, or unusual growths, colposcopy can provide a closer examination to determine their nature and potential significance.
- Follow-Up for Previous Abnormalities: Women who have had previous abnormal Pap smears or colposcopy procedures might be recommended for routine colposcopy to monitor the status of the cervix and identify any changes.
- Genital Warts: Colposcopy can be used to examine and diagnose genital warts (condyloma) on the cervix, vagina, or vulva.
- Monitoring After Treatment: If a woman has undergone treatment for precancerous lesions (such as a loop electrosurgical excision procedure or LEEP), colposcopy may be used to monitor the healing process and check for recurrence.
- Evaluation Before Certain Procedures: Colposcopy might be performed before certain procedures, such as cervical biopsies or cervical conization, to guide the healthcare provider and ensure accurate targeting of abnormal areas.
Preparing for Colposcopy:
- Schedule an Appointment: Contact your healthcare provider to schedule the colposcopy. It’s best to schedule the procedure for a time when you are not menstruating, as blood can interfere with the examination.
- Share Relevant Information: Inform your healthcare provider about any medications you are taking, allergies, and any relevant medical history. This includes any history of abnormal Pap smears, previous colposcopies, or other gynecological issues.
- Avoid Certain Activities: In the days leading up to the colposcopy, your healthcare provider may recommend avoiding sexual intercourse, vaginal medications, tampons, and douching. These activities can affect the appearance of the cervical tissues and the accuracy of the examination.
- Discuss Concerns: If you are anxious about the procedure or have specific concerns, don’t hesitate to discuss them with your healthcare provider. They can provide information and address your questions to help ease any worries.
- Consider Pain Management: While colposcopy is generally well-tolerated, some women may experience mild discomfort during the procedure. If you have concerns about pain, you can discuss pain management options with your healthcare provider, such as taking over-the-counter pain relievers before the procedure.
- Arrange Transportation: If you anticipate feeling uneasy after the procedure or if any pain relief is used, consider arranging for someone to drive you home afterward.
- Wear Comfortable Clothing: On the day of the procedure, wear comfortable clothing that is easy to remove, as you will need to change into a gown before the colposcopy.
- Ask About Timing: Ask your healthcare provider how long the procedure is expected to take. This can help you plan your day and any work or other commitments accordingly.
- Eat and Drink Normally: In most cases, you can eat and drink normally before the colposcopy. However, if your healthcare provider provides specific instructions, be sure to follow them.
- Relaxation Techniques: If you’re feeling anxious, consider using relaxation techniques, such as deep breathing or meditation, to help you stay calm before and during the procedure.
The Colposcopy Procedure:
- Preparation: You will be asked to change into a gown and lie down on an examination table, similar to a pelvic exam.
- Positioning: Your feet will be placed in stirrups to allow for better access to the pelvic area. This position is similar to what you might experience during a routine gynecological exam.
- Application of Solution: A solution, usually acetic acid (vinegar), is applied to the cervix, vagina, and sometimes the vulva. This solution helps highlight any abnormal areas by causing them to turn white. It might cause a mild stinging or burning sensation.
- Colposcope Placement: The colposcope is a binocular microscope with a light attached. The healthcare provider positions the colposcope a short distance away from the vaginal opening. Some colposcopes are mounted on a stand, while others are handheld.
- Visual Examination: The colposcope allows the healthcare provider to view the cervix, vagina, and vulva in detail. It provides a magnified view that allows for a thorough assessment of the tissues. The provider may adjust the focus and magnification to get a clear image.
- Lighting and Filters: The colposcope might have different lighting settings and filters that can enhance the visualization of certain types of tissues. This helps the healthcare provider identify abnormalities more easily.
- Colposcopic Findings: The healthcare provider will carefully examine the tissues for any abnormal areas, such as color changes, blood vessel patterns, or irregularities in the surface. The appearance of these areas can help determine whether a biopsy is necessary.
- Biopsy (If Needed): If the healthcare provider identifies suspicious areas, they might decide to perform a biopsy. A biopsy involves taking a small sample of tissue from the abnormal area for further examination in a laboratory. The biopsy may cause some brief discomfort or a pinching sensation.
- Application of Solutions (Optional): In some cases, additional solutions might be applied to the cervix to help identify specific types of abnormalities.
- Post-Procedure: Once the examination is complete, you can expect to rest for a few minutes. You will be able to resume your normal activities afterward.
- Results and Follow-Up: The findings from the colposcopy, including any biopsies, will be sent to a pathologist for analysis. Depending on the results, your healthcare provider will discuss the next steps with you, which might include additional tests, treatments, or monitoring.
Understanding Colposcopic Findings:
- Normal vs. Abnormal Tissues: During colposcopy, the healthcare provider examines the cervix, vagina, and vulva for any visual changes. Normal tissues typically appear pink and uniform, while abnormal areas might show variations in color, texture, or blood vessel patterns.
- Abnormalities and Patterns: Abnormal areas may present with different patterns, which can provide insights into the likelihood of precancerous or cancerous changes. These patterns include mosaicism (patchy appearance), punctation (tiny red dots), and acetowhite areas (white areas after acetic acid application).
- Blood Vessel Patterns: The distribution and appearance of blood vessels on the cervix are important indicators. Atypical blood vessel patterns, such as increased or irregular vessels, might suggest the presence of abnormal cells.
- Acetowhite Changes: Applying acetic acid to the cervix causes normal cells to turn slightly white. However, abnormal areas might turn a more intense white due to increased cell density. The intensity and extent of acetowhite changes are considered in the evaluation.
- Margin Assessment: The clear demarcation between normal and abnormal tissues is important. Well-defined margins might indicate a less severe abnormality, while indistinct margins could suggest a more advanced issue.
- Location and Extent: The location and size of abnormal areas are crucial for determining the level of concern. Larger or more widespread abnormalities may require closer scrutiny and possibly biopsies.
- Biopsy Guidance: Colposcopic findings often guide the decision to perform biopsies. Suspicious areas that are visually abnormal or show concerning patterns may be biopsied to obtain a tissue sample for further analysis.
- Grading of Abnormalities: The provider might assign a grading to abnormal findings based on their severity. Common gradings include CIN (cervical intraepithelial neoplasia) grades, where CIN 1 is mild, CIN 2 is moderate, and CIN 3 is severe dysplasia or carcinoma in situ.
- Clinical Decision Making: The colposcopic findings, along with the patient’s medical history and previous test results, help the healthcare provider determine the appropriate course of action. This might include additional testing, further observation, or treatment.
- Communication with Patients: It’s important for the healthcare provider to explain the colposcopic findings to the patient in understandable terms. Clear communication helps the patient make informed decisions about their healthcare.
Biopsy and Tissue Sampling:
- Reasons for Biopsy: A biopsy is performed when the healthcare provider identifies suspicious or abnormal areas during the colposcopy. The goal is to obtain a tissue sample for a more detailed examination under a microscope (histopathology) to confirm the presence of abnormal cells and determine their severity.
Types of Biopsies:
There are different types of biopsies that can be performed during or after colposcopy.
- Cervical Biopsy: This is the most common type of biopsy during colposcopy. Small samples of tissue are taken from the cervix using specialized instruments, such as biopsy forceps or punch instruments.
- Endocervical Curettage (ECC): In this procedure, a small curette (scoop) is used to gently scrape the lining of the endocervical canal. It helps ensure that cells from inside the cervical canal are included in the sample.
- Vulvar or Vaginal Biopsy: In some cases, biopsies of the vulva or vagina might be necessary if abnormalities are present in these areas.
- Procedure: The biopsy procedure is usually performed using local anesthesia to minimize discomfort. The healthcare provider will use the colposcope to guide the biopsy instrument to the target area. A small piece of tissue is then removed and collected for analysis.
- Number of Biopsies: The number of biopsies taken can vary depending on the extent and location of the abnormalities. Sometimes, multiple biopsies are taken from different areas to ensure a comprehensive assessment.
- Discomfort and Recovery: The biopsy procedure might cause a brief pinching sensation or cramping. After the biopsy, you might experience mild bleeding or spotting, as well as some discomfort similar to menstrual cramps. Over-the-counter pain relievers and resting for a day or two can help manage any discomfort.
- Pathology Examination: The collected tissue samples are sent to a pathology laboratory. A pathologist examines the tissue under a microscope to determine the presence of abnormal cells, the type of abnormality, and the severity. This information helps guide further treatment decisions.
- Results and Follow-Up: Once the pathology results are available, your healthcare provider will discuss the findings with you. Depending on the results, you might be advised on further monitoring, additional tests, or treatment options.
Interpreting Biopsy Results:
- Histopathology Report: The results of the biopsy are provided in a histopathology report generated by a pathologist. This report includes a description of the tissue samples, microscopic observations, and an interpretation of the findings.
- Type of Abnormality: The report will indicate the type of abnormality present, such as squamous intraepithelial lesions (SIL), cervical intraepithelial neoplasia (CIN), or atypical glandular cells. These terms indicate the extent of cell changes, from mild to severe.
- Grading or Staging: Biopsies may be graded or staged to describe the severity of abnormal cell changes:
- CIN Grading: CIN 1 (mild dysplasia), CIN 2 (moderate dysplasia), and CIN 3 (severe dysplasia or carcinoma in situ) are terms used to categorize the level of abnormal cell changes in the cervix.
- Cervical Cancer Staging: If cancer is detected, the biopsy results may include staging information indicating the extent of cancer spread. Staging helps guide treatment decisions.
- Extent and Margins: The report might describe the size of the abnormal area and whether it is well-defined or has indistinct margins. This information helps determine the risk and management approach.
- Recommendations: Based on the biopsy results, the pathologist might make recommendations for further management, such as additional tests, follow-up procedures, or treatment options.
- Further Testing: Depending on the biopsy findings, your healthcare provider might recommend additional tests to gather more information about the extent of the abnormality or to rule out other conditions.
- Treatment Options: The biopsy results play a significant role in determining the appropriate treatment. Treatment options can range from close monitoring and follow-up to more invasive procedures for removing abnormal tissue.
- Patient Communication: Your healthcare provider will discuss the biopsy results with you, explaining what the findings mean and addressing any concerns or questions you might have.
Management and Treatment Options:
Observation and Follow-Up:
- Mild abnormalities might not require immediate treatment. Your healthcare provider may recommend regular follow-up colposcopies to monitor any changes over time.
Lifestyle Modifications:
- In cases of mild abnormalities, maintaining a healthy lifestyle, including quitting smoking and practicing safe sexual behaviors, can help reduce the risk of progression.
Cryotherapy:
- Cryotherapy involves freezing and destroying abnormal cervical tissue using extreme cold. It is often used for treating low-grade cervical lesions.
Laser Therapy:
- Laser therapy uses a focused beam of light to remove or vaporize abnormal tissue. It can be used for treating precancerous or small cancerous lesions.
Loop Electrosurgical Excision Procedure (LEEP):
- LEEP involves using an electrical wire loop to remove abnormal tissue from the cervix. It’s effective for treating precancerous lesions.
Cone Biopsy (Conization):
- This procedure involves removing a cone-shaped piece of cervical tissue that includes the abnormal area. It’s used for more severe abnormalities or to diagnose invasive cervical cancer.
Hysterectomy:
- In cases of severe abnormalities or cervical cancer, a hysterectomy (removal of the uterus) might be recommended, sometimes along with removal of surrounding tissues.
Vaccination:
- If the abnormality is linked to HPV infection, your healthcare provider might recommend HPV vaccination to prevent future infections with high-risk HPV types.
Chemotherapy and Radiation:
- For cases of cervical cancer, more advanced treatments like chemotherapy and radiation therapy might be necessary, depending on the stage of the cancer.
Patient Counseling:
- Regardless of the treatment chosen, your healthcare provider will discuss the risks, benefits, potential side effects, and expected outcomes with you.
Potential Complications and Risks:
Here are some potential complications to consider.
- Discomfort and Pain: Some women may experience mild discomfort, cramping, or pain during the colposcopy or after a biopsy. This discomfort is usually temporary and can be managed with over-the-counter pain relievers.
- Bleeding: After a biopsy or certain procedures, you might experience light bleeding or spotting. This is normal and should subside within a few days. However, if bleeding is heavy or persistent, contact your healthcare provider.
- Infection: Infection is a rare but possible complication. It’s important to follow post-procedure care instructions, such as avoiding tampons and sexual intercourse for a specified time, to minimize the risk of infection.
- Cervical Stenosis: In some cases, especially after multiple procedures, scarring or tissue changes can lead to cervical stenosis (narrowing of the cervix). This can affect menstruation and fertility.
- Perforation: Rarely, there is a risk of perforation (piercing) of the uterus or cervix during procedures like biopsy or dilation and curettage (D&C). This risk is higher in postmenopausal women.
- Anxiety and Emotional Impact: The process of undergoing colposcopy and dealing with the possibility of abnormal results can cause anxiety and emotional stress for some individuals.
- False Positives or Negatives: Like any medical test, colposcopy and biopsies are not 100% accurate. There is a possibility of false-positive (indicating a problem when there isn’t one) or false-negative (missing an existing problem) results.
- Premature Birth: Some research suggests that women who have had multiple cone biopsies might have a slightly increased risk of premature birth if they become pregnant. However, the overall risk is still low.
FAQs:
What is a colposcopy, and why is it done?
Colposcopy is a medical procedure that involves examining the cervix, vagina, and vulva using a colposcope. It is done to investigate abnormal Pap smear results, detect cervical abnormalities, and identify conditions like HPV infection or genital warts.
Is colposcopy painful?
Colposcopy is usually not painful, but some women may experience mild discomfort or cramping during the procedure. Biopsies taken during colposcopy might cause a brief pinching sensation.
How long does a colposcopy take?
A colposcopy typically takes around 10 to 20 minutes, but the duration can vary based on individual circumstances and the need for additional procedures like biopsies.
Will I need a biopsy during colposcopy?
Not all women undergoing colposcopy need a biopsy. Biopsies are taken when the healthcare provider identifies suspicious or abnormal areas that require further evaluation.
What is a cervical biopsy?
A cervical biopsy involves removing a small sample of tissue from the cervix for laboratory analysis. It helps determine the presence and severity of abnormal cells or changes.
Are there any risks associated with colposcopy and biopsy?
While complications are rare, potential risks include discomfort, bleeding, infection, and very rarely, perforation. It’s important to discuss potential risks with your healthcare provider.
Can I resume normal activities after colposcopy or biopsy?
Yes, you can usually resume normal activities after colposcopy and biopsy. Your healthcare provider will provide specific guidelines based on your situation.
What happens if the biopsy results show abnormalities?
If the biopsy results indicate abnormalities, your healthcare provider will discuss the findings with you and recommend appropriate follow-up steps, which might include further testing or treatment.
Will I need treatment for abnormal biopsy results?
The need for treatment depends on the nature and severity of the abnormalities. Mild abnormalities might only require observation, while more severe findings might warrant treatment.
Can I have sexual intercourse after colposcopy or biopsy?
It’s generally recommended to avoid sexual intercourse for a certain period after the procedure, as advised by your healthcare provider, to minimize the risk of infection or discomfort.
How often do I need colposcopies if I have abnormal results?
The frequency of colposcopies depends on the findings and recommendations of your healthcare provider. They will determine the appropriate schedule based on your individual situation.
Is colposcopy always necessary after an abnormal Pap smear?
Colposcopy is commonly recommended after abnormal Pap smear results to further evaluate the cervix. However, your healthcare provider will consider your specific case and history when making recommendations.
Conclusion:
In conclusion, colposcopy is a vital diagnostic procedure in women’s health that offers a magnified and detailed view of the cervix, vagina, and vulva, enabling healthcare providers to identify and assess abnormalities that might otherwise go undetected. With the aid of the colposcope, healthcare professionals can make informed decisions about the need for biopsies, further testing, or treatment based on the observed patterns, color changes, and blood vessel distribution. While the process might evoke concerns, colposcopy’s significance in early detection of conditions like cervical dysplasia, HPV infections, and even cervical cancer is crucial. Clear communication between healthcare providers and patients, coupled with understanding the implications of findings, ensures informed decision-making, paving the way for effective management and improved women’s health outcomes.