Chemiluminescence immunoassay (CLIA) is a highly sensitive and widely used laboratory technique for detecting specific analytes, such as proteins, hormones, antibodies, drugs, and other biomolecules. It is a type of immunoassay, which means it relies on the binding specificity of antibodies to antigens to detect and quantify substances of interest in a biological sample.

What is CLIA?
CLIA stands for Chemiluminescence Immunoassay. It is a sensitive laboratory technique used to detect specific analytes in biological samples by generating light through a chemical reaction involving antibodies and labeled molecules. CLIA is widely used in clinical diagnostics, research, and drug testing due to its high sensitivity and ability to detect low concentrations of target substances.
Principles of CLIA:
The principles of Chemiluminescence Immunoassay (CLIA) are based on the specific binding between antibodies and antigens, combined with the generation of light through a chemical reaction. Here are the key principles of CLIA:
- Immunoassay Principle: CLIA is a type of immunoassay, which means it relies on the interaction between antibodies and antigens. Antibodies are proteins produced by the immune system in response to the presence of foreign substances (antigens) in the body. In CLIA, specific antibodies are used to target and bind to the analyte (substance of interest) in the biological sample.
- Solid Surface Immobilization: The surface of a solid support, such as a test tube, microplate, or membrane, is coated with immobilized antibodies. These antibodies are selected to be highly specific to the target analyte.
- Formation of a Sandwich Complex: In a typical CLIA, the sample containing the analyte is added to the coated surface. If the analyte is present in the sample, it binds to the immobilized antibodies, forming an antigen-antibody complex.
- Labeled Antibodies: Labeled antibodies are also introduced into the system. These antibodies are specific to the same analyte as the immobilized antibodies. They are attached to a molecule that can generate light through a chemical reaction, such as an enzyme like horseradish peroxidase or alkaline phosphatase.
- Chemical Reaction and Light Emission: After any unbound substances are washed away, a chemical substrate is added to initiate a reaction catalyzed by the labeled enzyme. The reaction leads to the release of energy, which is in the form of light (chemiluminescence).
- Detection and Quantification: The emitted light is measured using a sensitive detector, such as a photomultiplier tube or a charged-coupled device (CCD) camera. The intensity of the light is directly proportional to the amount of analyte present in the sample. The light emission is quantified, allowing for the determination of the analyte’s concentration.
- Calibration and Standardization: To obtain accurate and reliable results, CLIA instruments are calibrated using known standards with known concentrations of the analyte. These calibration curves help in converting the detected light signal into quantitative values.
Advantages of CLIA:
Chemiluminescence Immunoassay (CLIA) offers several advantages that make it a preferred choice for many applications in clinical diagnostics, research, and drug testing. Some of the key advantages of CLIA include:
- High Sensitivity: CLIA is exceptionally sensitive and capable of detecting analytes at very low concentrations. This attribute is crucial for identifying biomarkers and substances that may be present in trace amounts, making it effective for early disease detection and monitoring.
- Wide Analyte Range: CLIA can be used to detect a broad range of analytes, including proteins, hormones, drugs, antibodies, and various biomolecules. Its versatility allows for the assessment of multiple parameters in a single test, making it efficient and cost-effective.
- Specificity: The use of specific antibodies in CLIA ensures high target specificity. This specificity reduces the chances of cross-reactivity with other substances, leading to accurate and reliable results.
- Speed and Automation: CLIA can be automated, making it ideal for high-throughput analysis in clinical laboratories. The automated systems save time and reduce the risk of human errors, improving overall efficiency and productivity.
- Quantitative Analysis: CLIA provides quantitative measurements of analyte concentrations, allowing for precise and reproducible results. This information is valuable in determining disease progression, treatment efficacy, and overall patient management.
- Stability of Reagents: CLIA reagents, especially those involved in the chemiluminescent reaction, often have good stability. This stability reduces the need for frequent reagent preparation and helps extend the shelf life of the assay components.
- Lower Sample Volume: CLIA requires smaller sample volumes compared to some other immunoassay techniques. This feature is particularly beneficial when dealing with limited sample volumes, such as pediatric or neonatal samples.
- Minimal Interference: CLIA exhibits reduced interference from various substances present in biological samples. This advantage ensures that the assay results are less affected by sample matrix effects.
- Reduced Exposure to Radioactivity: Unlike some earlier immunoassay techniques like radioimmunoassay (RIA), CLIA does not involve the use of radioactive isotopes, making it safer for laboratory personnel and the environment.
- Clinical Relevance: CLIA is widely accepted and established in clinical practice. It is routinely used for diagnosing various diseases, assessing hormone levels, detecting infectious agents, and monitoring therapeutic drug levels.
DisAdvantages of CLIA:
While Chemiluminescence Immunoassay (CLIA) offers numerous advantages, it also has some disadvantages and limitations that should be considered. Some of the disadvantages of CLIA include:
- Cost: CLIA can be relatively expensive due to the need for specialized equipment, reagents, and instrumentation. The initial setup cost and ongoing maintenance expenses might pose financial challenges for smaller laboratories or healthcare facilities.
- Complexity: CLIA requires a certain level of technical expertise and training to operate and interpret the results accurately. The complexity of the assay may limit its use in settings where skilled personnel are not readily available.
- Cross-Reactivity: Although CLIA is designed to be highly specific, there can still be a possibility of cross-reactivity with similar substances or analytes with structural similarities. This may lead to false-positive or false-negative results in some cases.
- Limited Multiplexing: While CLIA can measure a wide range of analytes in a single sample, it may have limitations in multiplexing capabilities compared to some other techniques like multiplex bead-based assays.
- Matrix Effects: Biological samples can contain various interfering substances that may affect the assay’s accuracy and sensitivity. The presence of certain substances or matrices might require additional sample preparation steps or the use of specialized assays.
- Turnaround Time: Although CLIA is generally faster than some other immunoassay techniques, it may still have a longer turnaround time compared to rapid point-of-care tests, which provide results on the spot.
- Sensitivity to Environmental Factors: The performance of CLIA can be influenced by environmental factors, such as temperature and humidity. Careful control and monitoring of these conditions are necessary to maintain assay reliability.
- Limited Dynamic Range: While CLIA has excellent sensitivity for detecting low concentrations of analytes, its dynamic range (the range of concentrations it can accurately quantify) may be limited, especially for very high or very low concentrations.
- Reagent Stability: Despite the generally good stability of chemiluminescent reagents, some components may still have limited shelf life, requiring regular reagent replacement or quality control checks.
- Interference from Endogenous Substances: Some naturally occurring substances in biological samples can interfere with the chemiluminescent reaction, potentially affecting the accuracy of the results.
Applications of CLIA:
Chemiluminescence Immunoassay (CLIA) has a wide range of applications in clinical diagnostics, research, and drug testing due to its high sensitivity, specificity, and ability to detect low concentrations of analytes. Some of the key applications of CLIA include:
- Clinical Diagnostics: CLIA is extensively used in clinical laboratories to diagnose various diseases and medical conditions. It can measure biomarkers, hormones, antibodies, and other analytes indicative of specific diseases, such as cardiac markers for heart attacks, tumor markers for cancer, and infectious disease markers.
- Endocrinology: CLIA plays a crucial role in endocrinology by measuring hormone levels in the blood. It is commonly used to assess thyroid function, reproductive hormone levels, and adrenal hormone levels, aiding in the diagnosis and management of endocrine disorders.
- Therapeutic Drug Monitoring (TDM): CLIA is employed in TDM to measure drug concentrations in the blood, ensuring that medications are within the optimal therapeutic range. This helps healthcare providers adjust dosages for individual patients to achieve effective treatment and avoid toxicity.
- Allergy and Immunology: CLIA is used to detect allergen-specific IgE antibodies in the blood, aiding in the diagnosis of allergies. It is also utilized to assess immune response and antibody levels in various immunological disorders.
- Infectious Disease Testing: CLIA is widely used for detecting infectious agents, such as viruses, bacteria, and parasites, in clinical samples. It is crucial for diagnosing and managing infectious diseases, including HIV, hepatitis, and sexually transmitted infections.
- Autoimmune Disease Testing: CLIA is used to detect autoantibodies associated with autoimmune diseases, such as rheumatoid arthritis, systemic lupus erythematosus, and multiple sclerosis, aiding in early diagnosis and disease monitoring.
- Oncology and Cancer Biomarkers: CLIA is applied in oncology to detect tumor markers and cancer-specific antigens. It helps in cancer screening, diagnosis, and monitoring treatment responses in cancer patients.
- Reproductive Health: CLIA is used in reproductive health to measure hormones related to fertility and pregnancy, such as human chorionic gonadotropin (hCG) and progesterone.
- Drug Testing: CLIA is employed in drug testing programs, workplace drug screening, and forensic toxicology to detect drugs of abuse or therapeutic drugs in biological samples, such as urine and blood.
- Medical Research: CLIA is an essential tool in medical research for quantifying biomolecules and studying disease mechanisms. It aids in understanding disease progression, identifying new biomarkers, and evaluating potential therapeutic interventions.
Classification of CLIA:
Chemiluminescence Immunoassay (CLIA) can be classified as follows:
1. Based on the Type of Label:
- Direct CLIA: Chemiluminescent label directly attached to antigen/antibody.
- Indirect CLIA: Secondary antibody or molecule carries the label, amplifying the signal.
2. Based on the Nature of the Signal:
- Competitive CLIA: Analyte and labeled antigen compete for antibodies; signal inversely proportional to analyte concentration.
- Non-competitive CLIA (Sandwich): Analyte captured between two antibodies; signal directly proportional to analyte concentration.
3. Based on the Detection Method:
- Flash CLIA: Rapid light burst, requires sensitive detectors.
- Glow CLIA: Sustained light emission, easier measurement.
4. Based on the Chemiluminescent Substrate:
- Enzyme-Linked CLIA (CLEIA): Enzymes as labels; substrate reactions produce light.
- Direct Chemiluminescent Labeling: Chemiluminescent molecules directly attached to antigen/antibody.
- Electrochemiluminescence (ECLIA): Light generated through electrochemical reactions.
5. Based on Format:
- Competitive Immunoassay: Labeled and unlabeled antigens compete for binding sites.
- Sandwich Immunoassay: Large antigens captured between two antibodies.
6. Based on Solid Phase:
- Microplate-based CLIA: Uses microplates for high-throughput screening.
- Bead-based CLIA: Uses beads, often magnetic, for separation and washing.
- Magnetic Particle CLIA: Magnetic particles enhance separation and automation.
7. Based on Application:
- Hormone Assays: Measures hormone levels.
- Tumor Marker Assays: Detects cancer biomarkers.
- Infectious Disease Assays: Diagnoses infectious diseases.
- Drug Monitoring: Monitors therapeutic drug levels.
Types of Immunoassays:
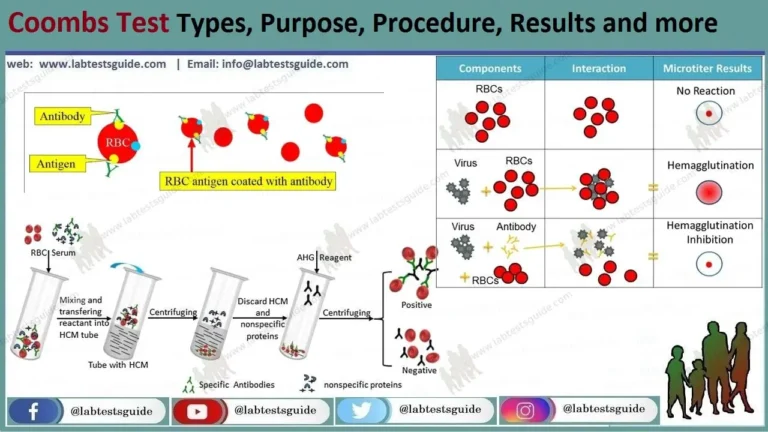
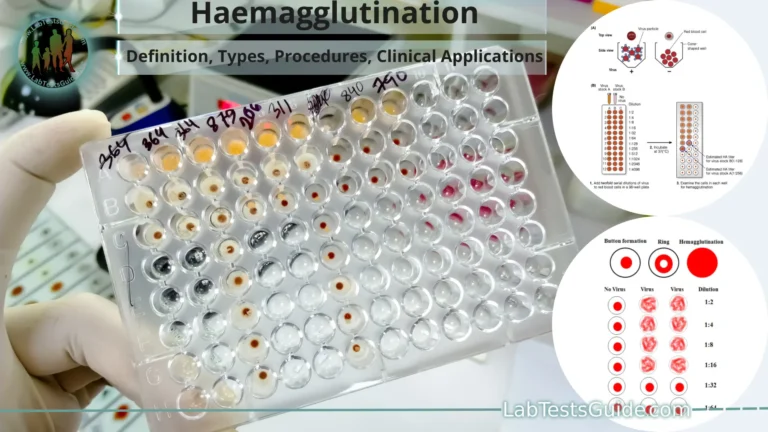
There are several types of immunoassays, each utilizing different methods to detect and quantify specific analytes. The main types of immunoassays include:
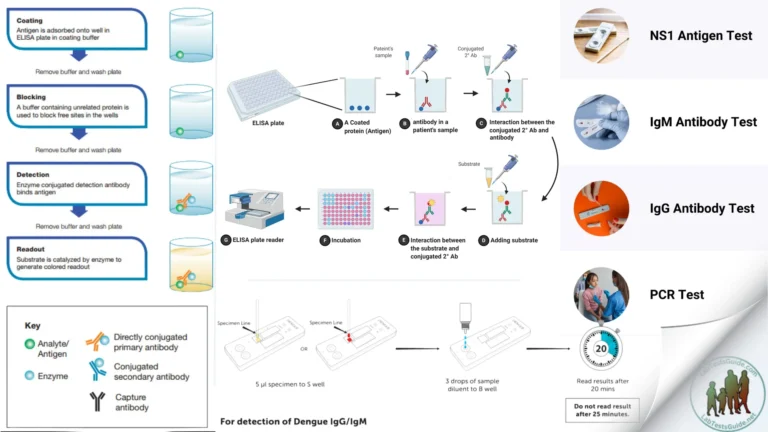
- Enzyme-Linked Immunosorbent Assay (ELISA): ELISA is one of the most widely used immunoassays. It involves the use of an enzyme-linked antibody to detect the presence of an analyte. The enzyme generates a colored or fluorescent signal upon interaction with a substrate, indicating the presence and quantity of the target analyte.
- Radioimmunoassay (RIA): RIA was one of the earliest immunoassay techniques. It uses radioactive isotopes as labels to measure the binding of an antigen to its specific antibody. The amount of radioactivity detected is proportional to the concentration of the analyte in the sample.
- Chemiluminescence Immunoassay (CLIA): As discussed earlier, CLIA uses a chemiluminescent reaction to generate light, which is measured to determine the presence and concentration of the target analyte. It offers high sensitivity and is widely used in clinical diagnostics.
- Fluorescence Immunoassay: Fluorescence immunoassays use fluorescent labels instead of enzymes or radioisotopes. When the labeled antibody binds to the analyte, it emits fluorescence, which is measured to quantify the concentration of the target substance.
- Immunofluorescence Assay (IFA): IFA is a technique that uses fluorescently labeled antibodies to visualize the presence of specific antigens in cells or tissues. It is commonly used in immunology and diagnostic pathology.
- Immunochromatographic Assay (ICA): ICA, also known as lateral flow immunoassay, is a simple and rapid immunoassay format commonly used in point-of-care testing. It employs colored particles to visualize the binding of analytes to specific antibodies.
- Particle-Enhanced Turbidimetric Immunoassay (PETIA): PETIA measures the change in turbidity caused by the formation of antigen-antibody complexes. It is often used in clinical laboratories for quantifying small molecule analytes.
- Homogeneous Immunoassays: Homogeneous immunoassays do not require separation steps as they rely on changes in signal properties due to antigen-antibody interactions. Examples include homogeneous enzyme immunoassays (HEIA) and homogeneous fluorescence immunoassays (HFIA).
- Enzyme Multiplied Immunoassay Technique (EMIT): EMIT is a type of competitive immunoassay that uses enzymes to generate a signal. It is commonly used in drug testing and therapeutic drug monitoring.
- Electrochemiluminescence Immunoassay (ECLIA): ECLIA combines elements of chemiluminescence and electrochemistry. It uses electrically generated species to initiate a chemiluminescent reaction, offering enhanced sensitivity.
Comparison with Other Immunoassay:
| Immunoassay Technique | Label Type | Detection Method | Sensitivity | Turnaround Time | Automation Potential | Cost | Clinical Applications |
|---|---|---|---|---|---|---|---|
| Chemiluminescence Immunoassay (CLIA) | Chemiluminescent | Light Emission | High sensitivity | Fast (generally short) | Highly automated | Moderate to High | Clinical diagnostics, TDM, infectious diseases |
| Enzyme-Linked Immunosorbent Assay (ELISA) | Enzyme | Color Change/F luorescence | Moderate to High | Moderate | Automatable | Moderate | Clinical diagnostics, research, drug testing |
| Radioimmunoassay (RIA) | Radioisotope (e.g., I-125) | Radioactivity measurement | High sensitivity | Moderate | Less automatable | High (radioactive isotopes) | Hormone assays, research, therapeutic drug monitoring |
| Fluorescence Immunoassay | Fluorescent | Fluorescence measurement | High sensitivity | Moderate | Automatable | Moderate | Research, diagnostics, cell imaging |
| Immunochromatographic Assay (ICA) | Colored particles | Visual detection | Moderate sensitivity | Rapid (few minutes) | Highly automated | Low to Moderate | Point-of-care testing, rapid diagnostics |
Components of CLIA:
Chemiluminescence Immunoassay (CLIA) involves several essential components that work together to detect and quantify specific analytes in biological samples. The key components of CLIA include:
- Solid Surface: The CLIA test is typically performed on a solid surface, such as a microplate, test tube, or membrane. This surface is coated with specific antibodies that are highly specific to the target analyte of interest.
- Immobilized Antibodies: Specific antibodies are immobilized or attached to the solid surface. These antibodies act as the capture reagents and are selected to bind exclusively to the target analyte when present in the sample.
- Sample: The biological sample, such as blood, serum, plasma, urine, or other bodily fluids, contains the target analyte. The sample is added to the solid surface to allow the interaction between the immobilized antibodies and the analyte.
- Labeled Antibodies: Labeled antibodies are specific to the same analyte as the immobilized antibodies. These labeled antibodies are conjugated with a molecule that generates light during a chemical reaction, such as an enzyme like horseradish peroxidase or alkaline phosphatase.
- Chemical Substrate: A chemical substrate is added to initiate the chemiluminescent reaction. This substrate interacts with the labeled enzyme to produce light when the labeled antibodies bind to the analyte.
- Light Emission System: The chemiluminescent reaction leads to the emission of light. The emitted light is measured using a sensitive detector, such as a photomultiplier tube or a charged-coupled device (CCD) camera.
- Wash Solution: To remove any unbound or nonspecifically bound components, a wash solution is used. It helps to eliminate interfering substances and improve assay specificity.
- Calibration Standards: Known concentrations of the analyte are used to calibrate the CLIA instrument. These calibration standards create a standard curve, allowing the conversion of light intensity into quantitative measurements of the analyte concentration in the sample.
- Quality Control Samples: Quality control samples with known analyte concentrations are used to assess the performance and accuracy of the CLIA system. These control samples are analyzed alongside the patient samples to monitor assay performance over time.
- Data Analysis Software: Specialized software is used to analyze the raw data obtained from the detector and convert it into quantitative results. The software assists in calculating the concentration of the target analyte based on the calibration curve.
Procedure of CLIA:
The procedure of Chemiluminescence Immunoassay (CLIA) involves several steps to detect and quantify specific analytes in a biological sample. Here’s a general overview of the CLIA procedure:
- Sample Preparation: The first step is to prepare the biological sample, such as blood, serum, plasma, urine, or other bodily fluids. The sample may need to undergo specific pre-treatment steps, such as dilution or centrifugation, to ensure it is suitable for the assay.
- Solid Surface Coating: A solid surface, such as a microplate, test tube, or membrane, is coated with specific antibodies that are highly specific to the target analyte. This coating process is performed in advance and involves immobilizing the antibodies on the surface.
- Incubation and Binding of Analyte: The prepared sample is added to the solid surface, and the plate or tube is incubated to allow the target analyte, if present in the sample, to bind to the immobilized antibodies on the surface. The incubation time is usually optimized to maximize the binding efficiency.
- Addition of Labeled Antibodies: After the incubation, labeled antibodies are introduced into the system. These labeled antibodies are specific to the same analyte as the immobilized antibodies. The labeled antibodies are conjugated with a molecule (e.g., an enzyme) that can produce light during a chemical reaction.
- Formation of Sandwich Complex: If the target analyte is present in the sample, the labeled antibodies bind to the analyte, forming a “sandwich complex” with the immobilized antibodies. This complex now consists of two antibodies bound to the same analyte.
- Chemical Reaction and Light Emission: After any unbound substances are washed away to remove interference, a chemical substrate is added to initiate a chemiluminescent reaction. The labeled enzyme catalyzes the reaction, leading to the emission of light (chemiluminescence).
- Detection and Quantification: The emitted light is measured using a sensitive detector, such as a photomultiplier tube or a charged-coupled device (CCD) camera. The intensity of the light is directly proportional to the amount of analyte present in the sample.
- Calibration and Data Analysis: The CLIA instrument is calibrated using known standards with known concentrations of the analyte. The calibration curve is used to convert the detected light signal into quantitative values. Data analysis software assists in calculating the concentration of the target analyte based on the calibration curve.
- Quality Control: Quality control samples with known analyte concentrations are run alongside patient samples to monitor assay performance and ensure accuracy and reliability.
- Reporting Results: The final step involves reporting the quantitative results of the CLIA assay, providing information on the concentration of the target analyte in the patient sample.
Factors Affecting CLIA Performance:
- Specificity of Antibodies: The specificity of the antibodies used in the assay is critical. If the antibodies cross-react with similar substances or show nonspecific binding, it can lead to false-positive or false-negative results, reducing assay accuracy.
- Sensitivity of Reagents: The sensitivity of the chemiluminescent reagents, including the labeled antibodies and the chemical substrate, plays a significant role in the detection of low analyte concentrations. High-quality, sensitive reagents are essential for achieving reliable results.
- Sample Matrix Effects: Biological samples, such as blood, serum, plasma, and urine, contain various endogenous substances that can interfere with the assay. Matrix effects can affect the binding of antibodies, leading to inaccurate quantification of the analyte.
- Sample Handling and Storage: Proper sample handling and storage are critical to maintaining sample integrity. Improper handling, contamination, or degradation of samples can compromise assay results.
- Calibration and Standardization: Accurate calibration using known standards with known concentrations of the analyte is essential for generating a reliable calibration curve. Calibration ensures that the CLIA instrument can accurately quantify the analyte concentrations in patient samples.
- Interference: Interference from substances other than the target analyte can affect assay specificity and sensitivity. Interference may arise from endogenous substances, medications, or contaminants present in the sample.
- Temperature and Time: The temperature and incubation time during the assay can impact the binding kinetics of the antibodies and analyte. Optimal temperature and incubation times must be determined to ensure reliable results.
- Instrumentation: The performance and accuracy of the CLIA instrument play a crucial role in obtaining reliable results. Regular maintenance, calibration, and quality control checks are necessary to ensure the instrument functions properly.
- Quality Control: Proper implementation of quality control measures, including the use of quality control samples with known analyte concentrations, helps monitor the assay’s accuracy and precision over time.
- Operator Variation: Operator technique and experience can influence assay performance. Proper training and adherence to standard operating procedures (SOPs) are essential to minimize operator-related variations.
- Cross-Reactivity: Some analytes may share structural similarities with the target analyte, leading to cross-reactivity with the antibodies. It is essential to consider potential cross-reactivity and account for it in the assay design.
Quality Control and Assurance in CLIA:
- Calibration: Regular calibration of the CLIA instrument is essential to establish a standard curve that relates the detected light signal to known concentrations of the analyte. Calibration ensures that the instrument is accurately quantifying the analyte concentrations in patient samples.
- Quality Control Samples: Quality control (QC) samples with known analyte concentrations are run alongside patient samples during each assay batch. These QC samples help monitor the accuracy and precision of the assay over time. They act as internal standards to verify the performance of the assay and the instrument.
- Control Charts: Control charts, such as Levey-Jennings plots, are used to monitor the performance of the assay and instrument over time. The control chart displays the QC results as they vary from day to day, allowing for the identification of trends or shifts in performance.
- Acceptance Criteria: Acceptance criteria are established based on the expected assay performance. QC results falling within the predefined acceptable ranges indicate that the assay is performing satisfactorily. If results fall outside the acceptable range, corrective action is taken to investigate and address potential issues.
- Troubleshooting and Corrective Action: When QC results deviate from the expected ranges, troubleshooting is performed to identify and resolve potential causes of the issue. Corrective action may involve recalibration, reagent replacement, or troubleshooting the instrumentation.
- External Quality Assessment (EQA): Participating in external quality assessment or proficiency testing programs is an essential part of CLIA quality assurance. These programs involve sending samples to external organizations for blind testing. The laboratory’s results are compared to other participants’ results to assess the accuracy and reliability of the assay.
- Standard Operating Procedures (SOPs): Laboratories should have well-documented SOPs for CLIA procedures. SOPs outline the standardized processes and protocols for each step of the assay, ensuring consistency and minimizing variation between operators.
- Training and Competency Assessment: Proper training of laboratory personnel is crucial for accurate and reliable CLIA results. Periodic competency assessments ensure that operators are proficient in performing the assay and adhering to quality control practices.
- Instrument Maintenance and Quality Checks: Regular maintenance and quality checks of the CLIA instrument are necessary to ensure its proper functioning. Routine maintenance activities include cleaning, calibration verification, and performance checks.
- Documented Records: Comprehensive record-keeping is essential for documenting all aspects of CLIA performance, including calibration data, QC results, troubleshooting, and corrective actions taken. Proper documentation facilitates auditing and helps identify any patterns of deviation.
Future Trends in CLIA:
As technology continues to advance, several future trends are expected to impact the field of Chemiluminescence Immunoassay (CLIA). These trends aim to enhance the sensitivity, efficiency, and versatility of CLIA assays, making them even more valuable in clinical diagnostics and research. Some of the future trends in CLIA include:
- Enhanced Sensitivity: Ongoing developments in assay reagents and detection systems are expected to further improve the sensitivity of CLIA. This will enable the detection of even lower concentrations of analytes, making CLIA even more valuable in early disease detection and monitoring.
- Multiplexing Capabilities: Future CLIA platforms are likely to offer increased multiplexing capabilities, allowing the simultaneous measurement of multiple analytes in a single sample. Multiplex CLIA will streamline testing processes, reduce sample volume requirements, and improve efficiency.
- Point-of-Care Applications: Advances in miniaturization and portable CLIA instrumentation may enable its implementation at the point-of-care settings, such as doctor’s offices, clinics, or remote areas. Point-of-care CLIA can provide rapid and accurate diagnostic results, facilitating timely patient management.
- Integration with Molecular Diagnostics: Combining CLIA with molecular diagnostic techniques, such as nucleic acid amplification assays, will allow for a comprehensive assessment of diseases by simultaneously measuring proteins and nucleic acids associated with specific conditions.
- Automation and High-Throughput Systems: Continuous progress in automation technology will further streamline CLIA processes, increasing throughput and reducing the hands-on time required. High-throughput CLIA systems will enable laboratories to handle a large volume of samples efficiently.
- Digital and Connectivity Integration: Future CLIA instruments may incorporate digital interfaces and connectivity features, allowing for real-time data analysis, remote monitoring, and seamless integration with laboratory information systems (LIS) for streamlined data management.
- Artificial Intelligence (AI) Applications: Integration of AI algorithms in CLIA data analysis can enhance result interpretation and assist in pattern recognition, leading to more accurate diagnosis and personalized treatment recommendations.
- Bioinformatics and Big Data Analysis: The generation of large-scale data from multiplexed CLIA assays will drive the need for advanced bioinformatics tools and data analysis methods to extract meaningful insights from complex datasets.
- Customization and Personalized Assays: Tailoring CLIA assays to specific patient needs or research requirements will become more feasible with advances in reagent customization and assay development services.
- Environmental and Food Safety Monitoring: CLIA’s high sensitivity and specificity make it suitable for environmental and food safety monitoring, enabling rapid and accurate detection of contaminants or toxins.
FAQs:
What is Chemiluminescence Immunoassay (CLIA)?
CLIA is a laboratory technique used to detect specific analytes in biological samples by generating light through a chemical reaction involving antibodies and labeled molecules. It is widely used in clinical diagnostics and research due to its high sensitivity and ability to detect low concentrations of target substances.
How does CLIA differ from ELISA?
CLIA and ELISA are both immunoassay techniques, but they differ in the method of signal generation. CLIA generates light through a chemiluminescent reaction, while ELISA uses an enzyme-linked antibody to produce a color change or fluorescence signal. CLIA is generally more sensitive than ELISA.
What are the advantages of CLIA over other immunoassay methods?
CLIA offers high sensitivity, wide analyte range, specific results, and automation potential. It has better sensitivity than some other immunoassay techniques like ELISA and is safer than radioimmunoassay (RIA) due to the absence of radioactive isotopes.
What are the main clinical applications of CLIA?
CLIA is used in clinical diagnostics for disease detection, monitoring treatment effectiveness, measuring hormone levels, and detecting infectious agents. It is also employed in therapeutic drug monitoring and drug testing.
Can CLIA be used in point-of-care settings?
Yes, advances in miniaturization and automation have made it possible to implement CLIA in point-of-care settings, providing rapid and accurate diagnostic results without the need for centralized laboratories.
How is CLIA quality controlled?
CLIA is quality controlled through regular calibration of instruments, use of quality control samples with known analyte concentrations, and the analysis of control charts to monitor assay performance over time.
What are the limitations of CLIA?
CLIA can be relatively expensive due to the need for specialized equipment and reagents. It may also have limitations in multiplexing capabilities compared to some other immunoassay techniques.
What factors can affect CLIA performance?
Factors affecting CLIA performance include the specificity of antibodies, sensitivity of reagents, sample matrix effects, calibration, interference, and proper sample handling and storage.
What are the future trends in CLIA?
Future trends in CLIA include enhanced sensitivity, increased multiplexing capabilities, point-of-care applications, integration with molecular diagnostics, automation, AI applications, and personalized assay development. These trends aim to improve CLIA’s efficiency, accuracy, and versatility in clinical diagnostics and research.
Conclusion:
In conclusion, Chemiluminescence Immunoassay (CLIA) is a powerful laboratory technique used to detect and quantify specific analytes in biological samples. Its ability to generate light through a chemiluminescent reaction, combined with the specificity of antibodies, makes it highly sensitive and effective in diagnosing diseases, monitoring treatments, and conducting medical research.



It is benifit information and I hope to explain classification of chemiluminescence if it possible.
Thank you for your comment! I’m glad you found the information helpful. I’ve updated the article to include a short explanation of the classification of chemiluminescence.