Anaphylaxis is a severe and potentially life-threatening allergic reaction that occurs rapidly after exposure to an allergen. An allergen is a substance that triggers an allergic response in some individuals. Common allergens that can trigger anaphylaxis include certain foods (such as peanuts, tree nuts, shellfish, and eggs), insect stings or bites (such as from bees or wasps), medications (especially antibiotics and nonsteroidal anti-inflammatory drugs), and latex.
Definition of Anaphylaxis.
Anaphylaxis is a severe and potentially life-threatening allergic reaction that occurs rapidly after exposure to an allergen. It is characterized by a wide range of symptoms that affect multiple systems of the body, including the skin, respiratory, cardiovascular, gastrointestinal, and sometimes the neurological system. Anaphylaxis can lead to a sudden drop in blood pressure, difficulty breathing, and other serious symptoms, and it requires immediate medical attention, often including the administration of epinephrine (adrenaline), to counteract the allergic reaction and prevent further complications.
Causes and Triggers of Anaphylaxis:
Common causes and triggers of anaphylaxis include.
- Foods: Certain foods are among the most common triggers of anaphylaxis. These may include peanuts, tree nuts (such as almonds, walnuts, and cashews), shellfish, fish, milk, eggs, soy, and wheat.
- Insect Stings: Insect stings or bites, particularly from bees, wasps, hornets, yellow jackets, and fire ants, can lead to anaphylactic reactions in susceptible individuals.
- Medications: Various medications can trigger anaphylaxis, with antibiotics (especially penicillin and related drugs) and nonsteroidal anti-inflammatory drugs (NSAIDs) being common culprits. Other medications, such as certain anesthetics and muscle relaxants, can also induce severe allergic reactions.
- Latex: Latex allergy can cause anaphylaxis in some individuals, particularly in healthcare workers or those with frequent exposure to latex products.
- Exercise: Exercise-induced anaphylaxis is a rare condition in which anaphylaxis occurs during or after physical activity, often in combination with certain foods or medications.
- Other Allergens: Less common allergens and triggers include allergens in the environment, such as pollen, latex, and animal dander. Allergens from specific sources, like certain fruits or vegetables (e.g., celery, strawberries), can also induce anaphylactic reactions, a condition known as oral allergy syndrome.
- Unknown Triggers: In some cases, the cause of anaphylaxis may remain unidentified, which is referred to as idiopathic anaphylaxis.
Signs and Symptoms of Anaphylaxis:
Common signs and symptoms of anaphylaxis include.
Skin Symptoms:
- Itching and hives (urticaria) on the skin, often accompanied by redness and warmth
- Swelling of the face, lips, tongue, or throat (angioedema)
Respiratory Symptoms:
- Shortness of breath and difficulty breathing
- Wheezing and persistent coughing
- Tightness or pain in the chest
- Nasal congestion or a runny nose
- Changes in voice, such as hoarseness
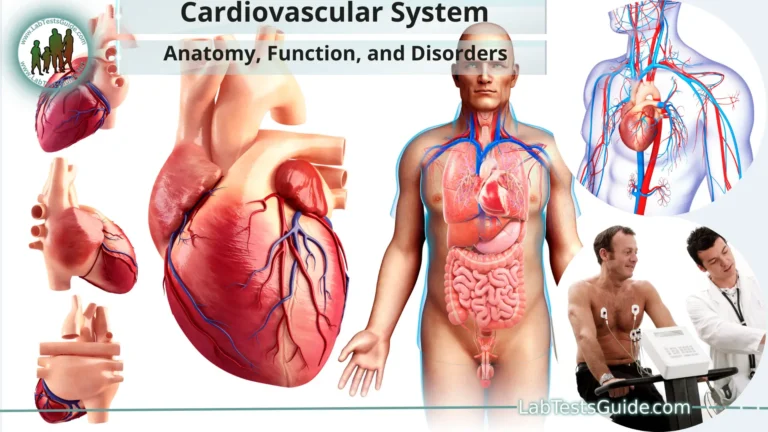
Cardiovascular Symptoms:
- Rapid, weak, or irregular heartbeat (palpitations)
- Low blood pressure, leading to dizziness, lightheadedness, or fainting
- Feeling of impending doom or anxiety
Gastrointestinal Symptoms:
- Nausea, vomiting, and/or diarrhea
- Abdominal pain and cramping
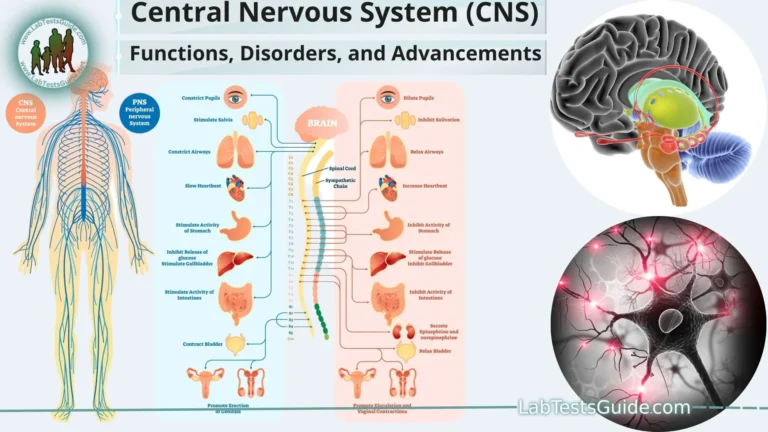
Neurological Symptoms:
- Confusion, disorientation, or mental fogginess
- Headache
- Feeling of a lump in the throat (globus sensation)
- Changes in consciousness, including a feeling of detachment
Other General Symptoms:
- Feeling of warmth or flushing
- Pallor (pale skin)
- Sense of unease or anxiety
- Sweating
Pathophysiology of Anaphylaxis:
Here is an overview of the pathophysiology of anaphylaxis.
- Exposure to Allergen: Anaphylaxis begins when an individual with a predisposition to allergies is exposed to an allergen. Allergens are typically harmless substances that the immune system mistakenly recognizes as a threat.
- Sensitization: In a previous encounter with the allergen, the person’s immune system produced specific antibodies, primarily immunoglobulin E (IgE), against the allergen. This process is called sensitization.
- Re-Exposure to Allergen: When the person is re-exposed to the same allergen, it can bind to the IgE antibodies attached to mast cells and basophils, which are immune cells found in tissues throughout the body, including the skin, respiratory tract, and gastrointestinal tract.
- Mast Cell Activation: The binding of allergen to IgE antibodies on mast cells triggers mast cell activation. Mast cells release a variety of chemical mediators, including histamine, leukotrienes, and prostaglandins.
Release of Chemical Mediators:
- Histamine is a key mediator in anaphylaxis and plays a central role in the development of symptoms. It causes blood vessels to dilate and become leaky, leading to increased permeability and swelling of tissues.
- Other chemical mediators, such as leukotrienes and prostaglandins, contribute to bronchoconstriction, smooth muscle contraction, and inflammation.
Systemic Effects:
- The release of these mediators results in a cascade of systemic effects, including.
- Vasodilation: This causes a drop in blood pressure, leading to lightheadedness, fainting, and shock.
- Bronchoconstriction: Constriction of the airways can lead to wheezing and severe difficulty breathing.
- Increased vascular permeability: This results in edema (swelling) of the skin and mucous membranes.
- Gastrointestinal effects: Increased permeability in the gut can cause nausea, vomiting, and diarrhea.
- Cardiac effects: The heart may beat irregularly due to the effects of these mediators.
- Multi-Organ Involvement: Anaphylaxis can affect multiple organ systems simultaneously, leading to a range of symptoms, including skin reactions, respiratory distress, cardiovascular collapse, and gastrointestinal disturbances.
- Rapid Onset: Anaphylaxis typically has a rapid onset, with symptoms appearing within minutes to hours of allergen exposure.
- Treatment: Epinephrine (adrenaline) is the primary treatment for anaphylaxis. It counteracts the effects of the chemical mediators by causing vasoconstriction, bronchodilation, and increased cardiac output, which helps reverse the life-threatening symptoms of anaphylaxis.
Diagnosis and Diagnostic Criteria:
Here are the key elements involved in diagnosing anaphylaxis.
Clinical Evaluation:
Healthcare professionals assess the individual’s symptoms, medical history, and the circumstances surrounding the suspected allergic reaction.
Diagnostic Criteria:
The criteria typically include the following.
- Acute onset: Anaphylaxis typically has a sudden and rapid onset of symptoms.
- Involvement of multiple systems: Anaphylaxis often involves multiple organ systems, such as skin, respiratory, cardiovascular, or gastrointestinal.
- Respiratory or cardiovascular symptoms: The presence of respiratory symptoms like difficulty breathing or cardiovascular symptoms like low blood pressure is highly suggestive of anaphylaxis.
- Skin or mucosal symptoms: Symptoms such as hives (urticaria), angioedema (swelling of the face or throat), or itching are common in anaphylaxis.
- Allergy Testing: After the acute episode is stabilized, allergy testing may be performed to identify the specific allergen responsible for the anaphylactic reaction. Common allergy tests include skin prick tests and blood tests (such as specific IgE antibody testing). Identifying the trigger allergen can help with future avoidance strategies.
- Differential Diagnosis: The healthcare provider will consider other conditions that may present with similar symptoms and signs, such as asthma exacerbations, panic attacks, or cardiovascular events. Distinguishing anaphylaxis from these conditions is essential for accurate diagnosis.
- Clinical History and Triggers: A detailed patient history is crucial to identify potential triggers. Asking about recent exposures to allergens, medications, insect stings, or other potential triggers is an important part of the diagnostic process.
- Response to Treatment: One of the most critical diagnostic criteria is the response to treatment with epinephrine. If a person experiences a rapid improvement in symptoms after receiving epinephrine, it strongly supports the diagnosis of anaphylaxis.
Prevention and Education:
Here are some important aspects of anaphylaxis prevention and education.
- Allergen Identification: Individuals at risk of anaphylaxis should identify their specific allergens through allergy testing. Knowing the trigger allergens is crucial for avoiding exposure.
- Avoidance Strategies: Once allergens are identified, individuals should take steps to avoid them. This may include reading food labels carefully, asking about ingredients when dining out, and being cautious about cross-contamination in kitchens.
- Medication Management: Individuals who have known allergies and are at risk of anaphylaxis may carry an epinephrine auto-injector (e.g., EpiPen) as prescribed by their healthcare provider. It’s essential to know how to use the auto-injector correctly and have it readily available at all times.
- Anaphylaxis Action Plan: Healthcare providers often work with individuals at risk of anaphylaxis to develop an anaphylaxis action plan. This plan outlines what to do in case of an allergic reaction, including when and how to use epinephrine and when to seek emergency medical help.
- Education and Awareness: Individuals at risk, their families, and caregivers should receive comprehensive education about anaphylaxis, its triggers, symptoms, and management. They should also be aware of their specific risk factors and any potential cross-reactivities between allergens.
- Training for Schools and Childcare Facilities: For children with severe allergies, schools and childcare facilities should have staff trained in recognizing and managing anaphylaxis. There should also be policies in place to accommodate the child’s needs, such as nut-free classrooms and meal options.
- Public Awareness: Public awareness campaigns can help educate the general population about anaphylaxis and how to respond in emergencies. This includes recognizing the signs of anaphylaxis and the importance of timely administration of epinephrine.
- Emergency Planning: Individuals at risk should have a plan in place for emergencies, including knowing the location of the nearest medical facility and how to call for emergency assistance.
- Travel Considerations: When traveling, individuals with allergies should plan ahead to ensure they have access to safe foods and medications. It’s also important to be aware of allergen labeling practices in different countries.
- Support Groups: Joining support groups or online communities for individuals with allergies and anaphylaxis can provide valuable information, resources, and emotional support.
Risk Factors and Prevalence:
Here are some key risk factors and prevalence considerations.
- History of Allergies: A significant risk factor for anaphylaxis is a history of allergies, particularly allergies to specific allergens such as peanuts, tree nuts, shellfish, insect stings, or certain medications.
- Previous Anaphylactic Episodes: Individuals who have previously experienced anaphylaxis are at higher risk of future episodes. The severity and unpredictability of allergic reactions can vary.
- Age: Anaphylaxis can occur at any age, but children, adolescents, and young adults are often more susceptible to severe allergic reactions. Food allergies, in particular, are common in children.
- Atopic Conditions: People with other allergic conditions, such as asthma, allergic rhinitis, or atopic dermatitis, may have an increased risk of anaphylaxis.
- Family History: Family history of allergies or anaphylaxis can increase an individual’s risk of developing allergies and experiencing anaphylactic reactions.
- Gender: Studies have shown that anaphylaxis appears to affect males and females equally, although some specific allergens may show gender differences in prevalence.
- Allergen Exposure: Exposure to specific allergens, especially in individuals who are sensitized to those allergens, is a key risk factor. For example, a person with a peanut allergy is at risk if they accidentally ingest peanuts.
- Medications: Some medications are more likely to cause anaphylaxis in susceptible individuals. For example, antibiotics like penicillin are known to be common triggers.
- Insect Stings: Reactions to insect stings, such as those from bees and wasps, can vary in severity. Individuals with a history of severe reactions are at higher risk.
- Occupational Exposure: Certain occupations, such as healthcare workers or laboratory technicians, may have an increased risk of latex-related anaphylaxis due to regular exposure to latex products.
Prevalence:
- The prevalence of anaphylaxis varies by geographic region and population. While anaphylaxis is relatively uncommon, its prevalence appears to be increasing in some parts of the world, particularly in developed countries.
- Food allergies, including those that can lead to anaphylaxis, are more prevalent in Western countries. Peanut and tree nut allergies are among the most common triggers.
- Insect stings are a common cause of anaphylaxis, with a higher prevalence in areas where stinging insects are more common.
- Medication-induced anaphylaxis varies depending on the frequency of medication use and the type of medication involved.
Anaphylaxis Management:
Here are the key steps in anaphylaxis management.
- Recognize Anaphylaxis: Early recognition of anaphylaxis is crucial. Be vigilant for the typical signs and symptoms, including skin reactions, difficulty breathing, swelling, and cardiovascular symptoms.
- Call for Help: Dial emergency services (911 or your local emergency number) immediately. Anaphylaxis is a medical emergency that requires professional medical assistance.
Administer Epinephrine (Adrenaline):
- Epinephrine is the first-line treatment for anaphylaxis and should be administered as soon as anaphylaxis is suspected, even before calling for help if necessary. Epinephrine helps counteract the allergic response by:
- Constricting blood vessels to raise blood pressure.
- Relaxing the airways to improve breathing.
- Reducing swelling and hives.
- Epinephrine is typically administered via an epinephrine auto-injector (such as an EpiPen) into the thigh muscle. Follow the instructions provided with the auto-injector or as advised by a healthcare professional.
- If the individual has their own prescribed epinephrine auto-injector, use it immediately.
- Position the Person: Have the individual lie down on their back with their legs elevated, if possible. This can help improve blood flow to vital organs.
- Monitor Vital Signs: Continuously monitor the person’s vital signs, including pulse and breathing rate. Be prepared to perform CPR if necessary.
- Provide Oxygen and Assist Breathing: If the person is having severe difficulty breathing or becomes unconscious, provide oxygen if available and be prepared to administer rescue breaths and perform CPR.
- Administer Additional Medications: In some cases, additional medications such as antihistamines (e.g., diphenhydramine) and corticosteroids (e.g., methylprednisolone) may be given to help control symptoms and prevent a delayed reaction.
- Prepare for Shock: Individuals with anaphylaxis are at risk of going into shock due to low blood pressure. Be prepared to manage shock, including keeping the person warm and elevating their legs (if appropriate).
- Transport to the Hospital: Even if the individual’s symptoms improve after epinephrine administration, it’s essential to transport them to the nearest hospital for further evaluation and monitoring. Anaphylaxis can sometimes have a biphasic (two-phase) reaction, with symptoms returning after an initial improvement.
- Inform Healthcare Providers: Provide the healthcare team with information about the allergen trigger, any previous allergic reactions, and the timing and treatment provided.
- Follow-Up Care: After anaphylaxis, individuals should follow up with an allergist or immunologist to identify the specific allergen and develop an anaphylaxis action plan. They may also receive recommendations for allergen avoidance and additional preventive measures.
Anaphylaxis in Special Populations:
Here are some specific considerations for anaphylaxis in these groups.
Anaphylaxis in Children:
- Children are at risk of anaphylaxis, especially due to food allergies. Common food allergens, such as peanuts, tree nuts, milk, and eggs, can trigger severe allergic reactions in children.
- School-aged children may be exposed to allergens in school settings. It’s crucial for schools to have anaphylaxis policies in place, including staff training and accommodations for children with allergies.
- Parents and caregivers of children with allergies should ensure that they carry epinephrine auto-injectors, and they should educate their children about allergen avoidance and how to use epinephrine when needed.
- Pediatric healthcare providers play a vital role in educating families about anaphylaxis management and creating individualized anaphylaxis action plans.
Anaphylaxis in Adults:
- Adults can develop new allergies or experience anaphylaxis even if they have not had severe allergic reactions in the past.
- Medications, such as antibiotics or nonsteroidal anti-inflammatory drugs (NSAIDs), are common triggers of anaphylaxis in adults.
- Adults with known allergies should always carry prescribed epinephrine auto-injectors and be aware of their triggers.
Anaphylaxis during Pregnancy:
- Anaphylaxis can occur during pregnancy, and it poses unique challenges. It’s essential for pregnant individuals with known allergies to manage their condition carefully.
- The safety of epinephrine use during pregnancy is generally well-established, and the benefits of treating anaphylaxis with epinephrine outweigh the risks.
- Healthcare providers should work closely with pregnant individuals to create an anaphylaxis management plan that considers the health and safety of both the mother and the developing fetus.
- Pregnant individuals should continue to avoid known allergens and carry their epinephrine auto-injector at all times.
Elderly Population:
- Anaphylaxis can affect elderly individuals, and they may have specific challenges in recognizing and managing symptoms. Elderly individuals may attribute symptoms to other medical conditions or medications.
- Healthcare providers should be aware of potential drug allergies and sensitivities in the elderly, as well as the importance of using epinephrine when necessary.
- Family members and caregivers of elderly individuals should be educated about anaphylaxis symptoms and the importance of immediate treatment.
Special Healthcare Needs:
- Individuals with developmental disabilities or special healthcare needs may require extra support and assistance in managing their allergies and anaphylaxis. Caregivers and support staff should receive training in recognizing and responding to anaphylactic reactions in these populations.
Complications and Long-Term Outlook:
Here are some potential complications and considerations related to the long-term outlook for individuals who have had anaphylaxis.
Biphasic Reactions:
- One potential complication of anaphylaxis is the occurrence of a biphasic reaction. After the initial symptoms are treated and appear to resolve, some individuals may experience a recurrence of anaphylaxis within hours or even days. It’s important for individuals to be aware of this possibility and continue monitoring their symptoms even after initial treatment.
Anxiety and Psychological Impact:
- Anaphylaxis can be a traumatic experience, and individuals who have experienced it may develop anxiety, fear, or post-traumatic stress related to future allergic reactions. This psychological impact can affect their quality of life and daily activities.
- Mental health support and counseling may be beneficial for individuals dealing with anxiety related to anaphylaxis.
Allergen Avoidance Challenges:
- Depending on the cause of anaphylaxis, individuals may face challenges in avoiding allergens in their daily lives. For example, those with food allergies must be vigilant about reading food labels, dining out, and managing potential cross-contamination.
- Allergen avoidance can sometimes be challenging and require significant lifestyle adjustments.
Allergy Testing and Allergen Identification:
- Following an anaphylactic episode, individuals may undergo allergy testing to identify the specific trigger allergen. Identifying the allergen is crucial for creating an effective anaphylaxis management plan.
- In some cases, allergy testing may reveal additional sensitivities or allergies that individuals were previously unaware of.
Post-Anaphylactic Syndrome:
- Some individuals may experience a condition known as post-anaphylactic syndrome. This involves lingering symptoms, such as fatigue, weakness, and altered mood, for several days following an anaphylactic episode.
- Post-anaphylactic syndrome is not fully understood, but it is a recognized phenomenon that may require supportive care.
Continuous Risk Management:
- Individuals who have had anaphylaxis must remain vigilant in managing their allergies and risks. This includes carrying and knowing how to use epinephrine auto-injectors, having an anaphylaxis action plan, and educating family members, friends, and caregivers about their condition.
Impact on Quality of Life:
- The long-term impact of anaphylaxis on an individual’s quality of life can be significant. It may affect their dietary choices, social activities, and travel plans.
- Support from healthcare providers, allergists, and support groups can help individuals adapt to their new reality and minimize the impact on their daily lives.
FAQs:
What is anaphylaxis?
Anaphylaxis is a severe and potentially life-threatening allergic reaction that occurs rapidly after exposure to an allergen. It can affect multiple systems in the body and requires immediate medical attention.
What are the common triggers of anaphylaxis?
Common triggers of anaphylaxis include foods (e.g., peanuts, tree nuts, shellfish), insect stings or bites, medications (e.g., antibiotics, NSAIDs), latex, and sometimes exercise.
What are the signs and symptoms of anaphylaxis?
Anaphylaxis can cause a wide range of symptoms, including skin reactions (hives, swelling), difficulty breathing, wheezing, low blood pressure, rapid heartbeat, nausea, vomiting, and confusion.
How is anaphylaxis treated?
The primary treatment for anaphylaxis is epinephrine (adrenaline), which is administered via an epinephrine auto-injector. Other medications like antihistamines and corticosteroids may be given, but epinephrine is the first-line treatment.
What should I do if I suspect someone is experiencing anaphylaxis?
If you suspect anaphylaxis, call 911 (or your local emergency number) immediately. Administer epinephrine if available, help the person lie down with legs elevated, and monitor their vital signs.
Can anaphylaxis be prevented?
While anaphylaxis can’t always be prevented, individuals with known allergies should identify their triggers, avoid allergens, and carry an epinephrine auto-injector. Education and awareness are key to prevention.
Can anaphylaxis occur in adults or only in children?
Anaphylaxis can occur in individuals of all ages, from infants to the elderly. It is not limited to any specific age group.
What is a biphasic reaction in anaphylaxis?
A biphasic reaction is a recurrence of anaphylactic symptoms after an initial improvement following treatment. This can happen hours or even days later, so continued vigilance is important.
Are there long-term effects of anaphylaxis?
Long-term effects can vary, but individuals who have experienced anaphylaxis may develop anxiety or post-traumatic stress related to future allergic reactions. Continuing to manage allergies and being prepared is important.
Is there a cure for anaphylaxis?
There is no cure for anaphylaxis, but it can be managed effectively with prompt treatment, allergen avoidance, and education. Epinephrine is the most important tool for managing acute reactions.
Conclusion:
In conclusion, anaphylaxis is a severe and potentially life-threatening allergic reaction that demands immediate recognition and intervention. With the right education, awareness, and preparedness, individuals at risk can effectively manage their allergies and reduce the risk of anaphylactic reactions. Ongoing research and advancements in anaphylaxis prevention, diagnosis, and treatment are improving the lives of those affected and increasing our understanding of this complex condition. Public awareness, access to epinephrine, and the development of individualized anaphylaxis action plans are key components in the effort to mitigate the risks associated with anaphylaxis and ensure the well-being of individuals with allergies.