Yersinia Selective Agar (YSA) is a specialized type of agar used in microbiology to selectively culture and identify Yersinia species, which are a group of bacteria known for causing various diseases in humans and animals, including Yersinia enterocolitica and Yersinia pseudotuberculosis.
- YSA: YSA stands for Yersinia Selective Agar. It is used for the selective isolation and identification of Yersinia species, particularly Yersinia enterocolitica and Yersinia pseudotuberculosis.
- CIN: CIN stands for Cefsulodin-Irgasan-Novobiocin Agar. This medium is used to isolate and identify Yersinia enterocolitica specifically. It contains cefsulodin, irgasan, and novobiocin to inhibit the growth of other bacteria while allowing Yersinia enterocolitica to grow. Read more >>

Key Points:
- Purpose: YSA is a specialized agar medium used in microbiology to selectively culture and identify Yersinia species of bacteria.
- Yersinia Species: It is primarily designed for the isolation and identification of Yersinia species, such as Yersinia enterocolitica and Yersinia pseudotuberculosis.
- Selective Medium: YSA is selective because it encourages the growth of Yersinia while inhibiting the growth of other bacteria.
- Components: It contains specific components, including bile salts, crystal violet, cefsulodin, mannitol, and sodium deoxycholate, which contribute to its selectivity.
- Bile Salts: Bile salts suppress the growth of many Gram-positive bacteria and some Gram-negative bacteria.
- Crystal Violet: Crystal violet is a dye that further inhibits the growth of competing bacteria.
- Cefsulodin: Cefsulodin is an antibiotic that specifically targets Yersinia species.
- Mannitol: Mannitol is included as a carbohydrate source for Yersinia species, and it can be fermented by some Yersinia strains.
- Sodium Deoxycholate: Sodium deoxycholate helps differentiate between Yersinia enterocolitica and Yersinia pseudotuberculosis based on their ability to ferment mannitol and produce acid.
- Isolation: YSA facilitates the isolation of Yersinia colonies from clinical specimens (e.g., stool samples) or environmental samples (e.g., food or water).
- Identification: Once isolated on YSA, Yersinia colonies can be further identified using various biochemical tests, serological assays, or molecular techniques.
- Virulence Factors: Identification may also involve testing for the presence of specific virulence factors that could indicate the pathogenic potential of the Yersinia strain.
- Safety Precautions: Due to the potential pathogenicity of Yersinia species, laboratories must adhere to strict biosafety protocols when working with YSA and Yersinia cultures.
- Clinical Significance: Yersinia species are associated with various diseases in humans, including gastroenteritis, so YSA is commonly used in clinical microbiology labs.
- Environmental Applications: YSA can also be employed in environmental monitoring to detect the presence of Yersinia in food, water, or other environmental samples, especially in outbreaks or contamination investigations.
Defination of Yersinia Selective Agar (YSA):
Yersinia Selective Agar (YSA) is a specialized microbiological medium for isolating and identifying Yersinia bacteria while inhibiting the growth of other microorganisms.
History and Modifications of YSA:
- Development: YSA was initially developed as a specialized agar medium for Yersinia species in the mid-20th century.
- Early Formulation: Early versions of YSA primarily contained bile salts and crystal violet to inhibit the growth of non-Yersinia bacteria.
- Cefsulodin Inclusion: Later modifications introduced the antibiotic cefsulodin to enhance selectivity for Yersinia.
- Mannitol Addition: Some formulations include mannitol as a carbohydrate source, aiding in the differentiation of Yersinia species based on their ability to ferment mannitol.
- Sodium Deoxycholate: Sodium deoxycholate may be included to distinguish between Yersinia enterocolitica and Yersinia pseudotuberculosis.
- Research and Optimization: Ongoing research and optimization have led to various YSA formulations tailored for specific Yersinia species and improved diagnostic accuracy.
- Safety Measures: Modifications also consider biosafety precautions, given the potential pathogenicity of Yersinia species.
- Environmental Applications: YSA has been adapted for environmental monitoring to detect Yersinia contamination in food, water, and other samples.
- Public Health Significance: Its evolution reflects the importance of YSA in public health efforts to identify and control Yersinia-related diseases.
Purpose and Significance of YSA:
The purpose and significance of Yersinia Selective Agar (YSA) in microbiology and public health are as follows:
Purpose:
- Selective Isolation: YSA is specifically designed to selectively isolate Yersinia species, including Yersinia enterocolitica and Yersinia pseudotuberculosis, from complex clinical and environmental samples.
- Suppressing Other Bacteria: It contains selective components like bile salts, crystal violet, and cefsulodin, which inhibit the growth of competing bacteria, allowing Yersinia colonies to dominate.
- Differentiation: YSA may include mannitol and sodium deoxycholate to differentiate between Yersinia species based on their biochemical reactions, aiding in species identification.
- Enhanced Detection: YSA enhances the recovery and detection of Yersinia species, particularly in samples where they may be present in low numbers.
Significance:
- Disease Diagnosis: YSA plays a crucial role in clinical microbiology for diagnosing Yersinia-related infections, such as gastroenteritis caused by Yersinia enterocolitica, allowing for targeted treatment.
- Outbreak Investigations: In cases of foodborne or waterborne outbreaks, YSA is used to identify and confirm the presence of Yersinia species, helping public health officials trace the source of contamination.
- Environmental Monitoring: YSA is employed in environmental monitoring programs to assess the prevalence of Yersinia in food, water, and environmental samples, contributing to food safety and public health.
- Research and Surveillance: YSA aids in the surveillance of Yersinia-related diseases, enabling researchers to study the prevalence, distribution, and virulence of Yersinia species.
- Biosafety: Its significance also lies in adhering to biosafety protocols when working with potentially pathogenic Yersinia species, minimizing the risk of laboratory-acquired infections.
- Public Health Response: YSA’s ability to selectively culture Yersinia species is vital for early detection and rapid response to outbreaks, reducing the impact on public health.
Importance of Agar in Microbiology:
Yersinia Selective Agar (YSA) holds significant importance in the field of microbiology, particularly in the isolation and identification of Yersinia species. Here are the key reasons for its importance:
- Selective Isolation: YSA is specifically formulated to selectively isolate Yersinia species while inhibiting the growth of other bacteria. This selectivity is crucial when dealing with complex clinical or environmental samples containing various microorganisms.
- Disease Diagnosis: Yersinia species, such as Yersinia enterocolitica and Yersinia pseudotuberculosis, are responsible for causing gastrointestinal infections in humans. YSA enables the isolation of these pathogens from clinical specimens, aiding in disease diagnosis and treatment.
- Outbreak Investigations: YSA is instrumental in outbreak investigations. During foodborne or waterborne outbreaks, it helps identify and confirm the presence of Yersinia species, assisting public health officials in tracing the source of contamination and implementing control measures.
- Environmental Monitoring: YSA is used in environmental monitoring programs to assess the prevalence of Yersinia in food, water, and environmental samples. This is essential for ensuring food safety and public health.
- Research: YSA supports research efforts aimed at understanding the prevalence, distribution, and virulence factors of Yersinia species. It contributes to our knowledge of these bacteria and their role in various environments.
- Biosafety: Yersinia species can be potentially pathogenic, and YSA provides a controlled and safe environment for working with these microorganisms in the laboratory. It helps minimize the risk of laboratory-acquired infections.
- Public Health Response: YSA’s ability to selectively culture Yersinia species is critical for early detection and rapid response to outbreaks. Timely identification of these pathogens can significantly reduce the impact on public health.
- Identification: Once Yersinia colonies grow on YSA, they can be further identified using various biochemical tests, serological assays, or molecular techniques, allowing for the differentiation of different Yersinia species and potential virulence factors.
- Clinical Microbiology: YSA is a staple in clinical microbiology laboratories, aiding in the diagnosis and management of Yersinia-related infections, particularly in cases of gastroenteritis.
Short Overview about Yersinia species:
Yersinia species are a group of bacteria known for their pathogenic potential in humans and animals. Here’s a short overview:
- Pathogenic Members: The most well-known pathogenic Yersinia species include Yersinia pestis, which causes bubonic and pneumonic plague; Yersinia enterocolitica and Yersinia pseudotuberculosis, which cause gastrointestinal infections; and Yersinia ruckeri, responsible for fish diseases.
- Transmission: Yersinia species are typically transmitted through contaminated food, water, or contact with infected animals. Y. pestis is also transmitted through flea bites.
- Symptoms: Infections can lead to a range of symptoms, including fever, abdominal pain, diarrhea, and, in the case of Y. pestis, severe systemic illness with swollen lymph nodes (buboes).
- Virulence Factors: Yersinia species possess various virulence factors, including adhesins, toxins, and a type III secretion system, which allows them to evade the host immune system and cause disease.
- Public Health Importance: Y. pestis is infamous for causing historical pandemics such as the Black Death. Y. enterocolitica and Y. pseudotuberculosis are significant causes of foodborne illnesses.
- Laboratory Identification: Identification of Yersinia species often involves microbiological culture, biochemical tests, serological assays, and molecular techniques. Selective media like Yersinia Selective Agar (YSA) aid in their isolation.
- Treatment: Antibiotics are used to treat Yersinia infections, but early diagnosis and treatment are crucial, especially in the case of Y. pestis infections, which can be life-threatening.
- Prevention: Preventive measures include proper food handling and hygiene to reduce the risk of infection. Vaccines are available for Y. pestis, primarily for at-risk populations.
Principles of YSA:
The principles of Yersinia Selective Agar (YSA) are based on its selective and differential properties, which allow for the isolation and identification of Yersinia species while inhibiting the growth of other microorganisms. Here are the key principles of YSA:
- Selective Growth: YSA is designed to selectively encourage the growth of Yersinia species while suppressing the growth of other bacteria that may be present in the sample. This selectivity is achieved through the inclusion of specific components.
- Selective Components: YSA contains various selective components, which may include bile salts, crystal violet, cefsulodin, mannitol, and sodium deoxycholate. These components inhibit the growth of competing bacteria, providing a favorable environment for Yersinia growth.
- Differential Properties: YSA can also serve as a differential medium. Depending on its formulation, it may include mannitol as a carbohydrate source. Yersinia species that can ferment mannitol and produce acid will display specific growth characteristics and colony appearances, aiding in their differentiation.
- Identification: Once Yersinia colonies grow on YSA, they can be further identified using various biochemical tests, serological assays, or molecular techniques. These tests help differentiate between different Yersinia species and may also assess the presence of virulence factors.
- Isolation: YSA facilitates the isolation of Yersinia colonies from complex clinical or environmental samples. This is essential for studying these bacteria and confirming their presence in various settings.
- Safety Precautions: Working with Yersinia species, which can be potentially pathogenic, requires adherence to strict biosafety protocols to prevent the spread of infection in the laboratory.
- Clinical and Environmental Applications: YSA is used in clinical microbiology laboratories to diagnose Yersinia-related infections, particularly in cases of gastroenteritis. It is also employed in environmental monitoring to detect the presence of Yersinia in food, water, and other environmental samples.
Clinical Applications of YSA:
Yersinia Selective Agar (YSA) has several important clinical applications in microbiology and clinical diagnostics. Here are some of the key clinical uses of YSA:
- Isolation of Yersinia Species: YSA is primarily used to isolate Yersinia species, such as Yersinia enterocolitica and Yersinia pseudotuberculosis, from clinical specimens. These bacteria are responsible for causing gastrointestinal infections in humans.
- Disease Diagnosis: YSA plays a crucial role in diagnosing Yersinia-related infections. When clinical specimens (e.g., stool samples) are plated on YSA, it allows for the selective growth and isolation of Yersinia colonies, which can then be further characterized.
- Outbreak Investigations: During outbreaks of foodborne or waterborne diseases caused by Yersinia species, YSA is employed to identify and confirm the presence of these pathogens in patient samples. This aids in tracing the source of contamination and implementing control measures.
- Differential Diagnosis: YSA can help differentiate between various Yersinia species and potentially identify the specific strain responsible for an infection. This information is important for patient management and treatment.
- Research and Epidemiology: YSA is used in research to study the prevalence, distribution, and virulence factors of Yersinia species. It contributes to our understanding of these bacteria and their impact on public health.
- Antimicrobial Susceptibility Testing: Isolates obtained on YSA can be subjected to antimicrobial susceptibility testing to determine the most effective antibiotics for treating Yersinia infections.
- Public Health Surveillance: YSA is a valuable tool in public health surveillance programs. It helps monitor the incidence of Yersinia-related diseases, allowing health authorities to identify trends and take preventive actions.
- Biosafety: YSA provides a controlled environment for working with potentially pathogenic Yersinia species, minimizing the risk of laboratory-acquired infections and ensuring the safety of laboratory personnel.
Ingredients, Materials and composition of YSA:
The specific formulation of Yersinia Selective Agar (YSA) can vary between manufacturers and laboratories, but generally, it contains ingredients and materials designed to create a selective environment for the isolation and identification of Yersinia species while inhibiting the growth of other microorganisms. Here’s a typical composition and materials used in YSA:
Ingredients:
- Peptone: Peptone is a source of nitrogen and essential nutrients that support the growth of microorganisms.
- Special: The term “special” is not specific, and its role in the medium may vary depending on the manufacturer or laboratory. It could refer to a proprietary or specific component tailored to enhance the medium’s selectivity.
- Yeast Extract: Yeast extract provides a source of vitamins, minerals, and amino acids, contributing to the nutritional requirements of microorganisms.
- Mannitol: Mannitol is a carbohydrate source that can be fermented by certain Yersinia species. The ability of Yersinia to ferment mannitol and produce acid is often used for differentiation.
- Sodium Pyruvate: Sodium pyruvate is sometimes added to the medium to support the growth of Yersinia species by providing additional nutrients.
- Sodium Chloride: Sodium chloride (salt) is a component that contributes to the overall osmolarity of the medium and affects microbial growth.
- Magnesium Sulfate: Magnesium sulfate provides essential ions required for bacterial growth and metabolism.
- Sodium Deoxycholate: Sodium deoxycholate is an ingredient that helps differentiate between Yersinia enterocolitica and Yersinia pseudotuberculosis based on their reactions with this compound.
- Neutral Red: Neutral red is a pH indicator that can help detect acid production, which is useful for differentiating Yersinia species.
- Crystal Violet: Crystal violet is a dye that further suppresses the growth of competing microorganisms.
- Agar: Agar is the solidifying agent that gives the medium its gel-like texture, providing a solid surface for microbial growth.
Materials:
- Agar Plates: YSA is typically prepared as solid agar plates. These plates provide a solid surface for microbial growth and are made of sterile plastic or glass.
- Sterile Water: Sterile water is used to dissolve and prepare the agar medium.
- Autoclave: An autoclave is used to sterilize the agar medium and ensure that it is free from contaminants.
- Laboratory Equipment: Standard laboratory equipment such as beakers, stirring rods, and pipettes are used in the preparation and dispensing of YSA.
Composition of Yersinia Selective Agar (YSA):
The exact composition and preparation method of YSA may vary depending on the specific laboratory’s protocols and the manufacturer’s instructions. It’s important to follow established procedures and quality control measures to ensure the reliability and consistency of the medium for microbiological applications.
| Ingredient | Quantity (per liter) | Purpose |
|---|---|---|
| Peptone | 10-20 grams | Nutrient source for microbial growth |
| Yeast Extract | 3-5 grams | Provides vitamins, minerals, amino acids |
| Mannitol | 2 grams | Carbohydrate source, fermentation indicator |
| Sodium Pyruvate | 0.3 grams | Nutritional support for Yersinia |
| Sodium Chloride | 5-10 grams | Osmolarity control, affecting microbial growth |
| Magnesium Sulfate | 0.2 grams | Provides essential magnesium ions |
| Sodium Deoxycholate | 0.1 grams | Differentiates Yersinia species based on reactions |
| Neutral Red | A few milligrams | pH indicator, detects acid production |
| Crystal Violet | A few milligrams | Suppresses the growth of competing bacteria |
| Agar | 15-20 grams | Solidifying agent for the medium |
| Water | To make up to 1 liter | Solvent for dissolving ingredients |
Please note that the specific quantities and formulations may vary slightly depending on the laboratory’s protocols or the manufacturer’s instructions. The above table provides a general guideline for the composition of YSA and the purposes of its individual ingredients in creating a selective and differential environment for Yersinia species.
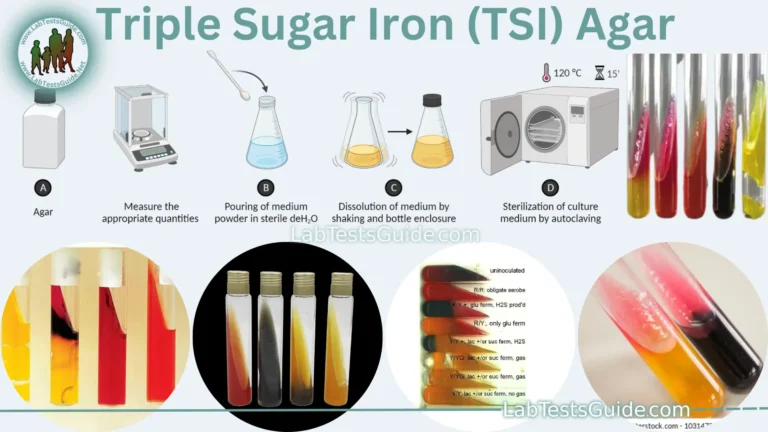
Preparation of Yersinia Selective Agar (YSA):
- Gather Ingredients: Collect the required ingredients, including peptone, yeast extract, mannitol, sodium pyruvate, sodium chloride, magnesium sulfate, sodium deoxycholate, neutral red, crystal violet, agar, and water.
- Measure Ingredients: Weigh the ingredients according to the specified quantities for your YSA recipe.
- Dissolve in Water: Add the ingredients to water and heat the mixture to dissolve them, creating a homogenous solution.
- Adjust pH: Adjust the pH of the solution to the specified range, typically around 7.4, using an appropriate pH indicator or meter.
- Sterilize: Autoclave (15 lbs pressure (121°C) for 15 minutes) the solution to sterilize it, ensuring that it is free from contaminants.
- Cool to 45-50°C and aseptically add reconstituted contents of 1 vial of Yersinia Selective Supplement or aseptically add 10 mL of a sterilized aqueous solution containing 4 mg of Cefsulodin and 2.5 mg of Novobiocin.
- Pour into Petri Dishes: Pour the sterilized YSA medium into sterile Petri dishes and allow it to solidify.
- Label and Store: Label the Petri dishes with necessary information (e.g., date, medium name) and store them in a cool, dry place until needed for microbiological work.
Required Specimins for Culturing:
To culture specimens on Yersinia Selective Agar (YSA), you would typically use clinical or environmental samples that may contain Yersinia species or related pathogens. Here are some examples of the types of specimens that can be cultured on YSA:
- Stool Samples: Stool specimens are commonly cultured on YSA to detect Yersinia species responsible for gastrointestinal infections. This is especially relevant in cases of suspected foodborne illnesses.
- Rectal Swabs: Rectal swabs are used to collect samples from individuals suspected of carrying Yersinia species asymptomatically or during disease outbreaks.
- Environmental Samples: YSA can be used to culture environmental samples from various sources, such as food, water, and soil, when investigating potential sources of Yersinia contamination or outbreaks.
- Clinical Tissue Samples: Tissue samples from infected sites, such as lymph nodes or intestinal tissues, may be cultured on YSA when investigating deeper infections.
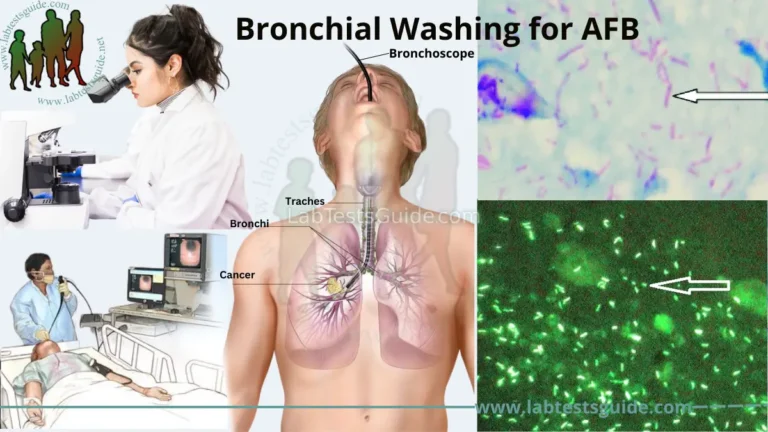
- Respiratory Samples: In some cases, respiratory specimens like sputum or throat swabs may be cultured on YSA, although this is less common.
- Blood Samples: For detecting systemic Yersinia infections, blood cultures may be performed using specialized culture media rather than YSA.
Usage Procedure of YSA:
The usage procedure of Yersinia Selective Agar (YSA) in a microbiological laboratory involves several steps to culture, isolate, and identify Yersinia species. Here is a general usage procedure:
Materials Needed:
- YSA plates
- Specimens (e.g., stool, swabs, environmental samples)
- Incubator (set to appropriate temperature)
- Sterile inoculating loop or swab
- Bunsen burner or incinerator
- Sterile gloves
- Biohazard waste disposal
Procedure:
- Preparation:
- Ensure that YSA plates are at room temperature before use.
- Put on sterile gloves to maintain aseptic conditions.
- Sterilize the inoculating loop or swab by passing it through a flame until it glows red. Allow it to cool briefly before use.
- Sample Collection:
- Collect the clinical or environmental specimen using appropriate methods and sampling techniques.
- Label the specimen container with necessary information, including the source, date, and any relevant patient or sample details.
- Inoculation:
- Aseptically streak or swab the specimen onto the surface of the YSA plate.
- Streaking for isolation can be done using the quadrant streak method or another appropriate technique to obtain isolated colonies.
- If testing multiple specimens, use a separate quadrant of the plate for each specimen.
- Incubation:
- Incubate the YSA plates at the appropriate temperature, typically around 30-37°C (86-98.6°F), depending on the Yersinia species being targeted. Incubation times may vary, but 24-48 hours is common.
- Yersinia colonies should grow and appear as pinpoint, translucent, or slightly raised colonies with a red center. The colonies’ appearance may vary based on the specific species and the YSA formulation.
- Examination:
- Examine the YSA plates for the presence of Yersinia colonies. The colonies may display specific characteristics, such as mannitol fermentation (change in colony color) and other biochemical reactions.
- Record colony morphology and any relevant observations.
- Identification:
- For further identification of Yersinia species, perform biochemical tests, serological assays, or molecular techniques as needed.
- Follow laboratory procedures and guidelines for species identification.
- Data Recording:
- Document all relevant information, including specimen source, colony characteristics, and any identification results.
- Safety Precautions:
- Dispose of used materials and biohazard waste properly, following laboratory safety protocols.
- Decontaminate any contaminated equipment and surfaces.
- Reporting:
- Report the results to relevant healthcare professionals or authorities, especially in cases of clinical diagnosis or outbreak investigations.
Result Interpretation of YSA:
| Observation | Interpretation | Further Steps (if applicable) |
|---|---|---|
| Small, translucent, pinpoint colonies with a Dark Pink center | Presumptive for Yersinia | Perform additional tests for confirmation and species identification. |
| No growth | Negative for Yersinia | No further steps required. |
| Growth of other bacteria, no Yersinia colonies | Negative for Yersinia | No further steps required. |
| Growth of colonies with different characteristics | May indicate mixed culture or contamination | Subculture and retest for Yersinia. |
| Growth with mannitol fermentation (color change) | May indicate Yersinia species capable of mannitol fermentation | Perform species-specific tests for identification. |
Coloney Characteristics of Yersinia species:
Source 1:
| Colony Characteristic | Interpretation |
|---|---|
| Small, circular, convex | Typical Yersinia appearance on YSA. |
| Translucent to slightly opaque | Yersinia colonies often appear translucent. |
| Entire colony may be red or red center with a yellowish outer edge | Mannitol-fermenting Yersinia species may produce colonies with this coloration. |
| May have a bull’s-eye appearance | Some Yersinia colonies, especially Yersinia enterocolitica, can exhibit a characteristic bull’s-eye or “target” appearance. |
| Variable in size | Colonies may vary in size, but they are generally small to pinpoint in appearance. |
| Smooth or slightly rough | Yersinia colonies are typically smooth or slightly rough in texture. |
Source 2:
| Yersinia species | Colony size | Colony color | Colony appearance |
|---|---|---|---|
| Yersinia enterocolitica | 1-2 mm | Pink to red-centred colonies surrounded by a transparent border | Bulls-eye appearance |
| Yersinia pseudotuberculosis | 1-2 mm | Gray-white to slightly yellow | Irregular, raised, “fried egg” appearance |
| Yersinia pestis | 1-2 mm | Gray-white to slightly yellow | Small, pinpoint colonies |
| Yersinia bercovieri | 1-2 mm | Pink to red-centred colonies surrounded by a transparent border | Bulls-eye appearance |
| Yersinia frederiksenii | 1-2 mm | Pink to red-centred colonies surrounded by a transparent border | Bulls-eye appearance |
Growth Other Bacterias on YSA:
When using Yersinia Selective Agar (YSA), it’s possible to observe the growth of other bacteria alongside Yersinia species. This can happen due to variations in the selectivity of the medium or the presence of contaminants. Here’s a simplified table to help interpret the growth of other bacteria on YSA:
| Observation | Interpretation | Further Steps (if applicable) |
|---|---|---|
| Growth of other bacteria, no Yersinia colonies | Negative for Yersinia | No further steps required. |
| Growth of non-Yersinia colonies | Presence of other bacteria or contaminants | Subculture and retest for Yersinia. |
| Mixed culture with both Yersinia and non-Yersinia colonies | Possible contamination or mixed sample | Subculture and retest for Yersinia. Identify and isolate non-Yersinia colonies for further study. |
It’s important to maintain strict laboratory practices to minimize the likelihood of contamination when working with YSA and to ensure accurate results when trying to culture and isolate Yersinia species. Subculturing and additional tests may be necessary to confirm the presence or absence of Yersinia species.
Limitations of YSA:
Yersinia Selective Agar (YSA) is a valuable medium for the selective isolation and identification of Yersinia species, but it also has limitations and potential drawbacks. Some of the limitations of YSA include:
- Selective Nature: While the selective components of YSA inhibit the growth of many competing bacteria, it may not completely eliminate all potential contaminants. Some fastidious or atypical strains may still grow on YSA.
- Species Variability: Different Yersinia species may have varying growth patterns and colony appearances on YSA, making it challenging to rely solely on colony morphology for species identification.
- Non-Yersinia Growth: YSA is not specific to Yersinia species. It can support the growth of certain other bacteria, especially if the medium is not used under optimal conditions.
- Complex Interpretation: Interpreting YSA results can be complex, especially when mixed cultures or unusual colony morphologies are present. Further testing is often required for accurate identification.
- False Positives and Negatives: YSA may yield false-positive or false-negative results. False positives can occur if non-Yersinia bacteria with similar colony appearances grow on the medium. False negatives can occur if the YSA formulation or incubation conditions do not support the growth of certain Yersinia strains.
- Limited to Yersinia: YSA is specifically designed for Yersinia species and may not be suitable for the isolation of other bacterial pathogens. Using YSA for non-Yersinia organisms may lead to incorrect results.
- Inhibitory to Some Yersinia Strains: In some cases, certain Yersinia strains may not grow well on YSA due to variations in their biochemical characteristics.
- Complex Preparation: Preparing YSA can be labor-intensive and requires precise measurements and careful handling of components. Variations in the preparation process can affect the medium’s selectivity and performance.
- Quality Control: Quality control measures are essential to ensure that YSA performs as intended. Inconsistent batches or improper storage can lead to unreliable results.
- Additional Testing: YSA is typically used as an initial screening medium. To confirm the presence and identify specific Yersinia species, additional tests such as biochemical assays, serological testing, or molecular techniques are often required.
Safety Considerations of YSA:
Working with Yersinia Selective Agar (YSA) in a laboratory setting requires careful attention to safety considerations due to the potential pathogenicity of Yersinia species and the need to prevent laboratory-acquired infections. Here are some safety considerations when handling YSA:
- Personal Protective Equipment (PPE):
- Wear appropriate PPE, including lab coats, gloves, and safety goggles or face shields to protect against potential splashes or aerosols.
- Biosafety Level: Determine the appropriate biosafety level (BSL) for handling Yersinia species based on the specific strains being used. Yersinia enterocolitica and Yersinia pseudotuberculosis are typically handled at BSL-2, while Yersinia pestis (the causative agent of plague) requires BSL-3 containment.
- Contaminated Materials: Handle all materials, including cultures and waste, as potentially contaminated with Yersinia. Properly label and dispose of biohazardous waste in accordance with established protocols.
- Hand Hygiene: Practice thorough handwashing with soap and water after handling YSA and potential Yersinia-contaminated materials. Hand sanitizers may not be sufficient for decontamination.
- Aseptic Technique: Use aseptic technique when inoculating YSA plates to prevent contamination of the medium and the laboratory environment.
- Autoclaving: Sterilize all equipment and materials before and after use, including inoculating loops, swabs, and media, using an autoclave or appropriate sterilization methods.
- Incubation: Incubate YSA plates in designated incubators at the recommended temperature for Yersinia growth, and label them clearly to prevent accidental exposure.
- Laboratory Design: Ensure that the laboratory has appropriate containment facilities and safety equipment, such as biological safety cabinets, to work with Yersinia species safely.
- Emergency Response: Familiarize laboratory personnel with emergency response procedures in case of spills, accidents, or exposures. Know the location of safety showers and eyewash stations.
- Training and Education: All laboratory personnel should receive training in the handling of Yersinia species, biosafety procedures, and the use of YSA. Regular refresher training is essential.
- Reporting: Report any accidents, exposures, or breaches of containment to laboratory management and follow the appropriate reporting and incident response procedures.
- Vaccination: For laboratories working with Yersinia pestis, consider vaccination of personnel with the appropriate plague vaccine and follow medical surveillance and vaccination protocols as required.
- Risk Assessment: Perform a risk assessment for each Yersinia species being handled to determine the appropriate safety precautions, containment levels, and laboratory practices.
Comparison with Other Microbiological Media:
Selective agents | Differential agents | Purpose | |
|---|---|---|---|
| Yersinia selective agar | Sodium oxalate, yersinia-specific antibodies, mannitol | Mannitol fermentation | Isolation and identification of Yersinia bacteria |
| MacConkey agar | Bile salts, crystal violet | Lactose fermentation | Isolation and differentiation of gram-negative bacteria |
| Hektoen enteric agar | Sodium desoxycholate, bile salts, lactose, sucrose | Lactose and sucrose fermentation, pH indicator | Isolation and differentiation of gram-negative bacteria |
| CIN agar (cefsulodin-irgasan-novobiocin agar) | Cefsulodin, irgasan, novobiocin | Mannitol fermentation | Isolation and identification of Yersinia bacteria |
| YECA (Yersinia enterocolitica agar) | Yersinia-specific chromogenic substrate | Mannitol fermentation, pH indicator | Isolation and identification of Yersinia enterocolitica |
Future Trends in Yersinia species Detection:
The field of Yersinia species detection is continually evolving as new technologies and research techniques emerge. Future trends in Yersinia species detection are likely to focus on several key areas:
- Rapid Molecular Detection: Molecular techniques such as polymerase chain reaction (PCR), next-generation sequencing (NGS), and loop-mediated isothermal amplification (LAMP) are becoming increasingly popular for the rapid and accurate detection of Yersinia species. These methods offer high sensitivity and specificity and can provide results in a matter of hours.
- Point-of-Care Testing: Advances in miniaturized and portable diagnostic devices are expected to lead to the development of point-of-care tests for Yersinia species detection. These tests will enable rapid diagnosis in clinical settings, especially in resource-limited areas and during outbreaks.
- Biosensors: The development of biosensors and microfluidic devices for Yersinia detection holds promise for real-time monitoring and field surveillance. These technologies can be used in environmental monitoring and food safety applications.
- High-Throughput Screening: Automation and robotics are likely to play a significant role in high-throughput screening of clinical and environmental samples for Yersinia species. This can improve the efficiency and speed of detection.
- Whole Genome Sequencing (WGS): WGS allows for the comprehensive analysis of Yersinia genomes, enabling not only species identification but also detailed characterization of strains, including virulence factors, antimicrobial resistance, and phylogenetic relationships.
- Bioinformatics and Data Analysis: Advanced bioinformatics tools will be crucial for handling and interpreting large-scale genomic data generated from Yersinia isolates. Machine learning and artificial intelligence may help identify unique genetic markers and patterns associated with virulent strains.
- One Health Approach: Future trends in Yersinia detection will likely incorporate a One Health approach, considering the interconnectedness of human, animal, and environmental health. Surveillance systems will become more integrated to detect and monitor Yersinia infections and outbreaks across multiple domains.
- Vaccines and Therapeutics: Research into Yersinia vaccines and therapeutics will continue, with a focus on developing more effective preventive and treatment options. Advances in understanding the biology and pathogenesis of Yersinia species may lead to novel targets for intervention.
- Antibiotic Resistance Monitoring: The surveillance of antibiotic resistance in Yersinia species will become increasingly important as antibiotic resistance continues to be a global health concern. Monitoring programs will help guide treatment strategies.
- Public Health Preparedness: Governments and health organizations will continue to invest in preparedness measures for Yersinia-related outbreaks, including the development of rapid response protocols, stockpiling of necessary supplies, and training of healthcare and laboratory personnel.
FAQs:
1. What are Yersinia species?
Yersinia species are a group of bacteria that can cause a range of diseases in humans and animals. The three most well-known species are Yersinia pestis (causes bubonic and pneumonic plague), Yersinia enterocolitica (causes gastrointestinal infections), and Yersinia pseudotuberculosis (also causes gastrointestinal infections).
2. What is Yersinia Selective Agar (YSA) used for?
Yersinia Selective Agar is a specialized culture medium used in microbiology laboratories to selectively isolate and identify Yersinia species from clinical and environmental samples. It provides an environment that encourages the growth of Yersinia while inhibiting the growth of other bacteria.
3. How does YSA work?
YSA contains specific components like bile salts, crystal violet, cefsulodin, and mannitol, which create a selective environment. Bile salts and cefsulodin inhibit the growth of many bacteria, while mannitol can be fermented by some Yersinia species, leading to the production of acid and a change in colony color.
4. What are the typical colony characteristics of Yersinia species on YSA?
Yersinia species on YSA often form small, translucent colonies with a red center (if they ferment mannitol). The appearance may vary depending on the species and the YSA formulation.
5. How is YSA prepared in the laboratory?
YSA is prepared by dissolving specific ingredients (peptone, yeast extract, mannitol, etc.) in water, adjusting the pH, and sterilizing the medium through autoclaving. It is then poured into Petri dishes and allowed to solidify.
6. What safety precautions should be taken when working with YSA?
Safety precautions include wearing appropriate personal protective equipment (PPE), using a biosafety level appropriate for the Yersinia species being handled, and following good laboratory practices to prevent contamination.
7. What are the limitations of YSA?
YSA is selective but not entirely specific, so it may not eliminate all competing bacteria. Interpretation can be complex, and further testing is often required for accurate identification.
8. Are there alternative methods for Yersinia species detection?
Yes, there are several methods for detecting Yersinia species, including molecular techniques (PCR, sequencing), serological assays, and traditional microbiological culture methods on other media.
9. What is the importance of Yersinia species detection in public health?
Detecting and identifying Yersinia species is crucial for diagnosing and managing diseases caused by these bacteria. It is also important for outbreak investigations, surveillance, and food safety monitoring.
10. What are some future trends in Yersinia species detection?
Future trends may include the development of rapid molecular detection methods, point-of-care testing, biosensors, and a One Health approach that considers human, animal, and environmental health in Yersinia surveillance and prevention.
Conclusion:
In conclusion, Yersinia Selective Agar (YSA) is a specialized microbiological medium designed for the selective isolation and identification of Yersinia species, which can cause various diseases in humans and animals. YSA provides a selective environment that encourages the growth of Yersinia while inhibiting the growth of other bacteria, making it a valuable tool in clinical diagnostics, environmental monitoring, and outbreak investigations.
Key points to remember about YSA include its composition, selective components (such as bile salts and mannitol), and the interpretation of colony characteristics. YSA is used to culture specimens collected from clinical and environmental sources, and the results are typically followed by further tests for species identification.
Safety considerations are essential when working with YSA due to the potential pathogenicity of Yersinia species. Proper personal protective equipment, biosafety measures, and adherence to laboratory safety protocols are crucial to prevent laboratory-acquired infections.
As the field of microbiology continues to evolve, future trends in Yersinia species detection may involve the development of rapid molecular techniques, point-of-care testing, biosensors, and a One Health approach to address the challenges posed by these bacteria comprehensively.
In summary, YSA plays a vital role in the detection and identification of Yersinia species, contributing to public health efforts and scientific research aimed at understanding and managing Yersinia-related diseases.