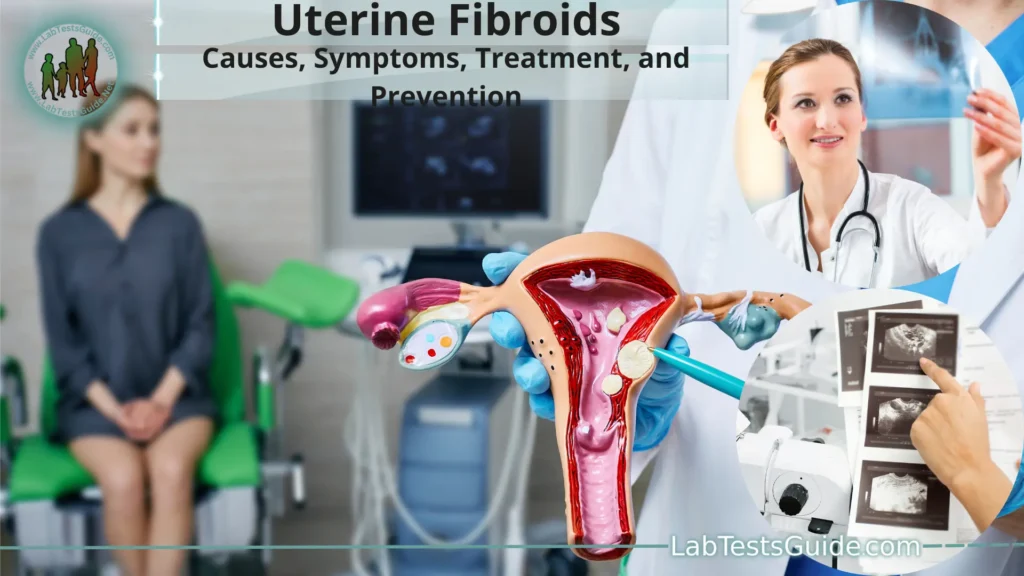
Uterine fibroids, also known as leiomyomas or myomas, are non-cancerous growths that develop within or on the walls of the uterus. They are the most common type of benign tumor found in women of childbearing age. Uterine fibroids can vary in size, ranging from tiny seedlings that are not visible to the naked eye to large masses that can distort the shape of the uterus.
What are Uterine Fibroids?
Uterine fibroids, also known as leiomyomas or myomas, are non-cancerous growths that develop within or on the walls of the uterus. They are the most common type of benign tumor found in women of childbearing age. Uterine fibroids are composed of smooth muscle cells and fibrous connective tissue, and their size can vary from small seedlings that are not visible to the naked eye to large masses that can distort the shape and size of the uterus.
The exact cause of uterine fibroids is not fully understood, but they are believed to be influenced by hormonal factors, particularly estrogen and progesterone. These hormones play a crucial role in the development and growth of the fibroids. Fibroids tend to grow in response to hormonal changes during a woman’s reproductive years when estrogen and progesterone levels are at their highest. During menopause, when hormone levels decrease, fibroids often shrink and become less symptomatic.
Causes and Pathogenesis:
Some of the key factors believed to play a role in the development of uterine fibroids include.
- Hormonal Influence: Estrogen and progesterone, two hormones that regulate the menstrual cycle and pregnancy, are thought to be significant contributors to the growth of fibroids. During the reproductive years, when hormone levels are at their highest, fibroids tend to grow and become more symptomatic. Conversely, during menopause, when hormone levels decline, fibroids often shrink and may become less problematic.
- Genetic Factors: There is evidence to suggest that genetic predisposition may play a role in the development of uterine fibroids. Women with a family history of fibroids have a higher risk of developing them themselves. Specific genes and genetic variations have been identified as potential contributors to fibroid development, but more research is needed to fully understand the genetic aspects of their pathogenesis.
- Growth Factors: Certain growth factors, such as insulin-like growth factor (IGF) and transforming growth factor-beta (TGF-β), may be involved in stimulating the growth of fibroids. These growth factors can affect the proliferation of smooth muscle cells in the uterus, leading to the formation of fibroids.
- Extracellular Matrix Abnormalities: The extracellular matrix, which provides structural support to tissues, may undergo changes in the uterine tissue, contributing to fibroid formation. These changes can affect cell signaling and lead to the abnormal growth of smooth muscle cells in the uterus.
- Angiogenesis: Fibroids require a blood supply to grow, and the process of angiogenesis, which involves the formation of new blood vessels, is essential for their development. Factors promoting angiogenesis may contribute to fibroid growth and expansion.
- Inflammation: Chronic inflammation in the uterine tissue may promote the development and growth of fibroids. Inflammatory mediators can influence cell growth and stimulate fibroid formation.
Symptoms of Uterine Fibroids:
Common symptoms of uterine fibroids include.
- Heavy or Prolonged Menstrual Bleeding: Fibroids can cause excessive menstrual bleeding, leading to prolonged periods or passing of large blood clots. Women may also experience increased cramping during menstruation.
- Pelvic Pain or Pressure: Large fibroids or those located in specific areas of the uterus can exert pressure on surrounding organs, causing pelvic pain, discomfort, or a feeling of fullness in the lower abdomen.
- Frequent Urination: Fibroids that press on the bladder can cause frequent urination or the urge to urinate more often than usual.
- Difficulty Emptying the Bladder: In some cases, fibroids can obstruct the normal flow of urine, making it challenging to completely empty the bladder.
- Constipation: Fibroids located near the rectum or intestines can lead to constipation or difficulty passing stools.
- Pain during Sexual Intercourse: Depending on their location, fibroids can cause pain or discomfort during sexual intercourse.
- Lower Back Pain: Fibroids may cause low back pain, especially when they exert pressure on the nerves in the lower back region.
- Enlarged Abdomen: Large fibroids can cause the abdomen to become enlarged, giving the appearance of pregnancy or a swollen belly.
- Anemia: Excessive menstrual bleeding caused by fibroids can lead to anemia, which is characterized by a low red blood cell count and can cause fatigue, weakness, and dizziness.
- Fertility Issues: Depending on their location and size, fibroids can sometimes interfere with fertility and increase the risk of pregnancy complications.
Types of Uterine Fibroids:
The types of uterine fibroids include.
- Intramural Fibroids: Intramural fibroids are the most common type and develop within the muscular wall of the uterus (myometrium). They can grow larger, distorting the shape of the uterus and potentially leading to symptoms such as heavy menstrual bleeding, pelvic pain, and pressure.
- Subserosal Fibroids: Subserosal fibroids grow on the outer surface of the uterus, extending outward and sometimes becoming pedunculated (attached to the uterus by a stalk). These fibroids may not significantly affect the uterine cavity but can cause symptoms like pelvic pain, pressure on adjacent organs, and an enlarged abdomen.
- Submucosal Fibroids: Submucosal fibroids are located just beneath the inner lining of the uterus (endometrium). They protrude into the uterine cavity and can cause significant symptoms, including heavy menstrual bleeding, prolonged periods, and fertility issues.
- Pedunculated Fibroids: Pedunculated fibroids are fibroids that develop a stalk or base, which attaches them to the uterine wall or outer surface. They can be intramural, submucosal, or subserosal in nature. Depending on their location, they may cause symptoms related to their size and position.
- Cervical Fibroids: Cervical fibroids develop in or around the cervix, which is the lower part of the uterus that connects to the vagina. They are relatively rare but can cause symptoms such as pain during intercourse and difficulty passing urine.
Diagnosing Uterine Fibroids:
Here are the common steps involved in diagnosing uterine fibroids.
- Medical History: Your healthcare provider will start by taking a detailed medical history, including asking about your symptoms, menstrual cycles, and any relevant family history. Be sure to provide information about any symptoms you may be experiencing, such as heavy or prolonged menstrual bleeding, pelvic pain, or other related issues.
- Physical Examination: During a pelvic examination, your healthcare provider will feel your abdomen and pelvis for any unusual lumps or masses. They will also check the size and position of your uterus. Depending on the location and size of the fibroids, they may be palpable during the examination.
Imaging Studies:
Imaging tests are crucial for confirming the presence of uterine fibroids and determining their size, number, and location. The following imaging modalities are commonly used.
- Ultrasound: Transabdominal or transvaginal ultrasound is often the first imaging test used to visualize the uterus and detect fibroids. This non-invasive procedure uses sound waves to create images of the pelvic organs.
- Magnetic Resonance Imaging (MRI): MRI provides detailed images of the uterus and fibroids, allowing for a better assessment of their size, location, and characteristics. It is particularly useful when planning for certain treatments, such as myomectomy or uterine fibroid embolization (UFE).
- Computed Tomography (CT) Scan: CT scans may be used to get a more comprehensive view of the pelvis, particularly if other imaging tests are inconclusive.
- Hysteroscopy (optional): If submucosal fibroids (fibroids inside the uterine cavity) are suspected, a hysteroscopy may be performed. In this procedure, a thin, lighted tube with a camera is inserted into the uterus through the vagina to visualize the uterine cavity and identify any abnormalities.
- Biopsy (optional): In some cases, a small tissue sample (biopsy) may be taken to rule out other conditions that can mimic the symptoms of uterine fibroids, such as cancer. However, fibroids themselves are typically non-cancerous.
Complications and Associated Conditions:
Some of the potential complications and associated conditions related to uterine fibroids include.
- Heavy Menstrual Bleeding (Menorrhagia): Large fibroids or submucosal fibroids that protrude into the uterine cavity can cause excessive menstrual bleeding. This can lead to anemia, a condition characterized by a low red blood cell count, resulting in fatigue, weakness, and dizziness.
- Pelvic Pain and Pressure: Fibroids can cause pelvic pain or discomfort, especially when they grow large or press on nearby organs. Women may experience a feeling of heaviness or pressure in the lower abdomen.
- Urinary Symptoms: Depending on their location, fibroids can compress the bladder, leading to increased frequency of urination, urgency, or difficulty emptying the bladder fully.
- Bowel Symptoms: Large fibroids may put pressure on the rectum or intestines, causing constipation, difficulty passing stools, or even bowel obstruction in rare cases.
- Infertility and Pregnancy Complications: Submucosal fibroids can interfere with implantation and pregnancy, potentially leading to fertility issues or recurrent miscarriages. Large fibroids can also increase the risk of certain pregnancy complications, such as preterm labor, abnormal fetal position, or difficulty during delivery.
- Red Degeneration: In some cases, fibroids may undergo a process called red degeneration, where the blood supply to the fibroid is disrupted, leading to pain and tenderness in the fibroid. This usually occurs during pregnancy and can cause acute pain requiring medical attention.
- Hyaline Degeneration: Hyaline degeneration is a type of fibroid degeneration in which the fibroid’s tissue becomes more fibrous and less vascular. While this degeneration is usually not symptomatic, it may be detected during imaging studies or surgical procedures.
- Increased Abdominal Girth: Large fibroids can cause the abdomen to become enlarged, resembling pregnancy or abdominal distention.
- Iron-Deficiency Anemia: Chronic and heavy menstrual bleeding caused by fibroids can lead to iron-deficiency anemia due to the loss of red blood cells. Anemia can cause fatigue, weakness, and shortness of breath.
Treatment Options:
Some common treatment options for uterine fibroids include.
- Watchful Waiting and Monitoring: If the fibroids are small, asymptomatic, or not causing significant problems, your healthcare provider may recommend a watchful waiting approach. Regular check-ups and monitoring may be suggested to ensure that the fibroids are not growing or causing any complications.
Medications:
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs): NSAIDs, such as ibuprofen or naproxen, can help relieve pelvic pain and menstrual cramps associated with fibroids.
- Hormonal Birth Control: Birth control pills, hormonal patches, or intrauterine devices (IUDs) with progestin can help regulate heavy menstrual bleeding and reduce pain in some cases.
- Gonadotropin-Releasing Hormone (GnRH) Agonists: These medications can temporarily induce a menopausal state, reducing estrogen levels and causing fibroids to shrink. They are typically used for short periods before surgical interventions.
- Uterine Fibroid Embolization (UFE): UFE is a minimally invasive procedure in which the blood supply to the fibroids is blocked, causing them to shrink and alleviating symptoms. It is an effective option for women who want to preserve their uterus and avoid surgery.
- Myomectomy: Myomectomy is a surgical procedure in which the fibroids are surgically removed, leaving the uterus intact. It is often recommended for women who wish to retain their fertility or have significant symptoms caused by fibroids.
- Hysterectomy: Hysterectomy involves the removal of the uterus and is considered a definitive treatment for uterine fibroids. It is typically recommended for women who no longer desire to have children or have severe symptoms that do not respond to other treatments.
- MRI-Guided High-Intensity Focused Ultrasound (MRgFUS): This non-invasive procedure uses focused ultrasound waves to heat and destroy the fibroid tissue. It can be effective for treating small to medium-sized fibroids.
- Endometrial Ablation: Endometrial ablation is a procedure that involves removing or destroying the endometrial lining of the uterus, which can reduce heavy menstrual bleeding caused by submucosal fibroids.
- Hysteroscopic Resection: This procedure involves removing submucosal fibroids through a hysteroscope inserted into the uterus through the vagina. It is a minimally invasive option for treating certain types of fibroids.
Managing Fibroid Symptoms:
Here are some strategies for managing fibroid symptoms.
- Pain Management: Over-the-counter pain relievers, such as nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen, can help alleviate pelvic pain and menstrual cramps associated with fibroids.
- Hormonal Birth Control: Hormonal contraceptives, such as birth control pills, patches, or intrauterine devices (IUDs) with progestin, can help regulate heavy menstrual bleeding and reduce pain in some cases.
- Iron Supplementation: If heavy menstrual bleeding has led to iron-deficiency anemia, iron supplements may be prescribed to restore iron levels and improve energy levels.
- Heat Therapy: Applying a heating pad to the lower abdomen can help relieve pain and discomfort associated with fibroids.
- Exercise: Regular physical activity can help improve overall health and may alleviate some fibroid symptoms. Exercise can also help manage stress, which can contribute to symptom exacerbation.
- Dietary Changes: Some women find that reducing their consumption of red meat and caffeine can help manage fibroid symptoms. A well-balanced diet rich in fruits, vegetables, and whole grains is generally recommended.
- Stress Management: Stress can exacerbate fibroid symptoms, so finding effective ways to manage stress, such as meditation, yoga, or deep breathing exercises, can be beneficial.
- Uterine Fibroid Embolization (UFE): UFE is a minimally invasive procedure that blocks the blood supply to the fibroids, causing them to shrink and alleviate symptoms.
- Myomectomy: Surgical removal of fibroids (myomectomy) may be considered for women who want to preserve their fertility or have significant symptoms caused by fibroids.
- Endometrial Ablation: This procedure involves removing or destroying the endometrial lining of the uterus and can be effective in reducing heavy menstrual bleeding caused by submucosal fibroids.
- Hormonal Therapy: In some cases, hormonal therapies such as gonadotropin-releasing hormone (GnRH) agonists or progestin-releasing intrauterine devices (IUDs) may be used to shrink fibroids and alleviate symptoms temporarily.
- Pain Management During Pregnancy: For pregnant women with fibroids experiencing pain, rest, heat therapy, and safe pain medications as advised by a healthcare provider may be recommended.
Lifestyle Changes and Prevention:
Here are some lifestyle changes and preventive measures to consider.
- Maintain a Healthy Diet: Eat a well-balanced diet rich in fruits, vegetables, whole grains, and lean proteins. Avoid excessive consumption of red meat, processed foods, and sugary beverages. A healthy diet can help maintain a healthy weight and reduce inflammation, potentially benefiting fibroid management.
- Exercise Regularly: Engage in regular physical activity, such as walking, swimming, or yoga. Exercise can help improve blood circulation, reduce stress, and promote overall health.
- Manage Stress: Chronic stress can exacerbate fibroid symptoms. Practice stress-reduction techniques such as meditation, deep breathing exercises, or mindfulness practices.
- Maintain a Healthy Weight: Obesity is associated with an increased risk of fibroids and may worsen symptoms. Aim to achieve and maintain a healthy weight through a balanced diet and regular exercise.
- Limit Alcohol Consumption: Excessive alcohol consumption can impact hormone levels and may contribute to the growth of fibroids. Limit alcohol intake to moderate levels or avoid it altogether.
- Quit Smoking: Smoking is associated with an increased risk of fibroid development and may worsen fibroid-related symptoms. If you smoke, consider quitting to improve your overall health.
- Birth Control Options: Hormonal contraceptives, such as birth control pills or hormonal IUDs, can regulate menstrual cycles and reduce heavy bleeding caused by fibroids.
- Regular Health Check-ups: Regular visits to your healthcare provider for preventive check-ups and screenings can help detect any health issues early, including fibroids.
- Family Planning: If you have concerns about fibroids and their impact on fertility, discuss your family planning options with your healthcare provider. They can help you understand how fibroids may affect your reproductive goals.
- Stay Informed: Educate yourself about uterine fibroids and their symptoms. Being aware of the signs and symptoms can help you seek medical attention promptly if needed.
FAQs:
What are uterine fibroids?
Uterine fibroids are non-cancerous growths that develop within or on the walls of the uterus. They are composed of smooth muscle cells and fibrous connective tissue.
Who is at risk of developing uterine fibroids?
Women of childbearing age, especially between 30 and 50 years old, are at a higher risk of developing uterine fibroids. Other risk factors include a family history of fibroids, obesity, and early onset of menstruation.
What are the symptoms of uterine fibroids?
Symptoms can vary but may include heavy or prolonged menstrual bleeding, pelvic pain, frequent urination, difficulty emptying the bladder, constipation, and an enlarged abdomen.
How are uterine fibroids diagnosed?
Uterine fibroids can be diagnosed through a pelvic examination, imaging studies (ultrasound, MRI, or CT scan), and sometimes hysteroscopy or biopsy.
Can uterine fibroids lead to infertility?
Depending on their size and location, uterine fibroids can interfere with fertility and increase the risk of pregnancy complications. However, not all fibroids will affect fertility.
What are the treatment options for uterine fibroids?
Treatment options include watchful waiting, medications, uterine fibroid embolization (UFE), myomectomy, hysterectomy, MRI-guided focused ultrasound, and hysteroscopic resection.
Are there any lifestyle changes that can help manage fibroid symptoms?
Yes, lifestyle changes such as maintaining a healthy diet, exercising regularly, managing stress, and avoiding excessive alcohol and smoking can help manage fibroid symptoms.
Can uterine fibroids become cancerous?
Uterine fibroids are typically benign, meaning they are not cancerous. However, in rare cases, a type of cancer known as leiomyosarcoma can develop in the uterine tissue, but it is not directly related to the presence of fibroids.
Can fibroids go away on their own?
Some fibroids may shrink or go away on their own, particularly after menopause when hormone levels decrease. However, others may persist and may require medical intervention.
Can fibroids come back after treatment?
In some cases, fibroids may recur after treatment, especially if not all fibroids were removed during surgery or if new fibroids develop over time.
Conclusion:
Uterine fibroids are common non-cancerous growths that can develop in or on the uterus, affecting women of childbearing age. Although their exact cause remains unclear, hormonal influence, genetic factors, and other elements may contribute to their pathogenesis. Symptoms can vary widely, ranging from heavy menstrual bleeding and pelvic pain to an enlarged abdomen and urinary problems. While prevention of fibroid development is not possible, managing symptoms through lifestyle changes, medical treatments, and surgical interventions can help improve women’s quality of life and address fertility concerns. Early diagnosis, regular health check-ups, and informed decision-making can aid in the effective management of uterine fibroids tailored to individual needs and preferences.
Home | Blog | About Us | Contact Us | Disclaimer