Anencephaly is a rare and severe congenital birth defect that occurs during early fetal development. It is a type of neural tube defect (NTD) in which the neural tube, which eventually forms the brain and spinal cord, fails to close properly. As a result, a major portion of the baby’s brain and skull is underdeveloped or missing. Anencephalic infants are born with only a rudimentary brainstem, which controls basic reflexes and functions such as heartbeat and breathing.
Definition of Anencephaly.
Anencephaly is a severe and rare congenital birth defect characterized by the absence or severe underdevelopment of the brain, skull, and scalp in a developing fetus. In babies born with anencephaly, the neural tube, which normally forms the brain and spinal cord, fails to close properly during early fetal development. As a result, the upper part of the neural tube does not develop into a fully formed brain and cranial vault (skull). Instead, only a rudimentary brainstem may be present, which controls basic functions such as heartbeat and breathing.
Causes and Risk Factors:
Here are some of the known causes and risk factors associated with anencephaly.
Genetic Factors:
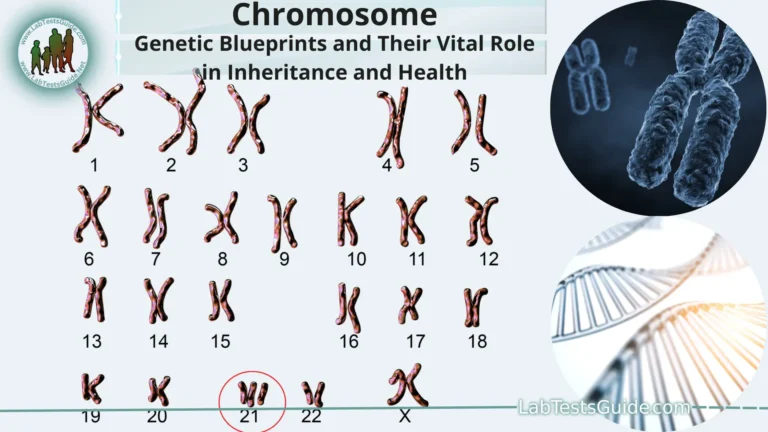
- Family History: Having a family history of neural tube defects (NTDs), including anencephaly, can increase the risk for future generations.
- Genetic Mutations: Certain genetic mutations or alterations may predispose individuals to an increased risk of anencephaly. These genetic factors can be inherited from one or both parents.
Folic Acid Deficiency:
- Insufficient intake of folic acid (vitamin B9) during early pregnancy is a well-established risk factor for neural tube defects, including anencephaly. Folic acid plays a crucial role in neural tube development, and adequate supplementation is recommended before and during pregnancy to reduce the risk.
Environmental Factors:
- Maternal Factors: Exposure to certain environmental factors during pregnancy may increase the risk of anencephaly. These factors can include maternal obesity, uncontrolled diabetes, and the use of certain medications.
- Chemical Exposures: Some studies have suggested that exposure to certain chemicals, such as certain pesticides and solvents, may be associated with an increased risk of neural tube defects, although the evidence is not always conclusive.
Other Factors:
- Geographical Variation: The prevalence of anencephaly can vary by geographical region, suggesting that environmental and possibly genetic factors specific to certain areas may contribute to the risk.
- Ethnicity: Some ethnic groups may have a higher risk of neural tube defects, including anencephaly.
Prenatal Diagnosis:
Here are some common prenatal diagnosis methods.
Ultrasound Screening:
- Transabdominal Ultrasound: Typically performed during the first trimester, this non-invasive imaging technique uses high-frequency sound waves to create images of the developing fetus. Anencephaly can often be visualized on ultrasound as a severe cranial abnormality, with a missing or poorly developed skull and brain.
- Transvaginal Ultrasound: In some cases, a transvaginal ultrasound may be used to provide clearer images during the early stages of pregnancy.
Maternal Serum Alpha-Fetoprotein (AFP) Testing:
- AFP is a protein produced by the fetal liver. Elevated levels of AFP in the maternal blood can be an indicator of neural tube defects, including anencephaly. This blood test is typically performed between the 15th and 20th weeks of pregnancy.
- An elevated AFP level may prompt further diagnostic tests or ultrasounds to confirm the presence of anencephaly.
Amniocentesis:
- Amniocentesis is an invasive diagnostic procedure performed in the second trimester (usually between 15 and 20 weeks of gestation). A thin needle is inserted into the amniotic sac to collect a sample of amniotic fluid, which contains fetal cells and proteins.
- The amniotic fluid can be tested for elevated AFP levels and other markers associated with neural tube defects. It can also be used for genetic testing to determine if there are any chromosomal abnormalities or genetic mutations contributing to the condition.
Chorionic Villus Sampling (CVS):
- CVS is another invasive diagnostic procedure that can be performed earlier in pregnancy, typically between 10 and 13 weeks. It involves the removal of a small piece of tissue from the placenta (chorionic villi) for genetic testing.
- CVS can detect chromosomal abnormalities and genetic mutations that may be associated with anencephaly.
Clinical Features:
Here are key points regarding prevention and folic acid supplementation.
Folic Acid Supplementation:
- Folic acid is essential for the proper development of the neural tube during early pregnancy, usually before a woman even realizes she is pregnant. Taking folic acid supplements before and during the early weeks of pregnancy is a crucial preventive measure.
- Most healthcare organizations recommend that women who are planning to become pregnant or who are capable of becoming pregnant take a daily folic acid supplement containing at least 400 micrograms (mcg) of folic acid. Some women at higher risk, such as those with a history of NTD-affected pregnancies or certain medical conditions, may require higher doses, and this should be discussed with a healthcare provider.
Dietary Sources of Folate:
- In addition to supplements, women can increase their folate intake through a diet rich in folate-containing foods. These include leafy green vegetables (such as spinach and kale), citrus fruits, beans, lentils, fortified cereals, and fortified grain products (like bread and pasta).
- While a balanced diet is important, it can be challenging to get the recommended amount of folate from food alone, which is why supplements are often recommended.
Preconception Care:
- Ideally, folic acid supplementation should begin at least one month before conception and continue throughout the first trimester of pregnancy. This is because the neural tube typically forms within the first 28 days after conception, often before a woman is aware she is pregnant.
- Women who are actively trying to conceive should ensure they are taking the recommended daily dose of folic acid as part of their preconception care.
High-Risk Groups:
- Some women may be at higher risk of having a pregnancy affected by anencephaly or other NTDs. This includes women with a personal or family history of NTDs, women with certain medical conditions, and women taking medications that interfere with folate metabolism. These individuals may require higher doses of folic acid and should consult with a healthcare provider.
Public Health Campaigns:
- Many countries have implemented public health campaigns to raise awareness about the importance of folic acid supplementation and to encourage women of childbearing age to take folic acid supplements. These campaigns aim to reduce the occurrence of NTDs.
Prognosis and Management:
Here are the clinical features commonly associated with anencephaly.
Absence of Cranial Vault:
- Anencephaly is often characterized by the absence of a significant portion of the skull, including the brain’s protective covering. The exposed brain tissue may be visible, covered by only a thin membrane or layer of skin.
- The absence of a cranial vault leaves the brain unprotected, making it vulnerable to damage.
Brain Abnormalities:
- The most significant feature of anencephaly is the underdevelopment or absence of the brain itself. In affected infants, the cerebral hemispheres (the large, outer part of the brain) are typically missing or severely reduced in size.
- The remaining brain tissue may consist of a rudimentary brainstem, which controls basic reflexes and functions like heartbeat and breathing.
Scalp Abnormalities:
- Infants with anencephaly often have abnormalities of the scalp, such as a flat or poorly formed area where the skull should be. The scalp may also appear translucent, and hair is usually absent in this region.
Facial and Craniofacial Features:
- Facial features of anencephalic infants can vary, but they may include abnormalities in the structure and positioning of the eyes, ears, and mouth. These features can be distorted or displaced due to the absence of the cranial vault.
- Infants with anencephaly may exhibit a characteristic appearance, but the severity of craniofacial abnormalities can vary.
Neurological Deficits:
- Because of the severe brain underdevelopment, infants with anencephaly typically do not exhibit normal neurological function. They lack higher brain functions and cognitive abilities.
- Basic reflexes, such as those related to breathing and heartbeat, may be present, but the infant’s neurological responses are very limited.
Motor Function Impairment:
- Anencephalic infants generally have limited motor function and are unable to control their movements intentionally. They may exhibit spontaneous reflexive movements but cannot engage in purposeful actions.
Survival and Life Expectancy:
- Unfortunately, due to the severe nature of anencephaly and the absence of essential brain structures, infants with this condition typically do not survive for an extended period after birth. Most are stillborn or die shortly after birth.
- Rarely, some infants with anencephaly may survive for a short time, but their life expectancy is extremely limited, and they have minimal cognitive function.
Prevention and Folic Acid Supplementation:
Here are key points regarding the prognosis and management of anencephaly.
Life Expectancy:
- Infants with anencephaly are often stillborn, and those who are born alive usually do not survive for more than a few hours or days after birth. The absence or severe underdevelopment of essential brain structures means that they cannot sustain life beyond a very short period.
Lack of Cognitive Function:
- Anencephalic infants lack higher brain structures responsible for consciousness, cognition, and sensory perception. They do not exhibit normal neurological function and do not have the capacity for awareness or meaningful interaction.
Palliative Care:
- When an infant is born with anencephaly, medical care is typically focused on providing comfort and support during the brief time the infant is alive. This is known as palliative care.
- Palliative care aims to ensure that the infant is as comfortable as possible and free from pain. It may include measures such as swaddling the baby, providing warmth, and offering comfort to the family during their time with the infant.
Emotional Support and Counseling:
- Parents who receive a prenatal diagnosis of anencephaly face emotionally challenging decisions. Healthcare providers offer counseling and support to help parents make informed choices about the continuation of the pregnancy and the care of their affected child.
- Grief support and counseling services are also important for parents and families who experience the loss of a child with anencephaly.
Ethical Considerations:
- The ethical considerations surrounding anencephaly are complex and can involve discussions about the quality of life, end-of-life care decisions, and cultural and personal beliefs.
- Decisions regarding the continuation of the pregnancy and the course of medical care are deeply personal and should be made in consultation with healthcare providers, counselors, and support networks.
Research and Advancements:
Here are some key areas of research and advancements related to anencephaly.
- Genetic Studies: Researchers are conducting genetic studies to identify specific genetic factors and mutations that may increase the risk of anencephaly. Understanding the genetic basis of the condition can lead to better risk assessment and potentially targeted interventions.
- Environmental Factors: Investigations into environmental factors that may contribute to anencephaly are ongoing. Researchers aim to identify specific exposures or conditions during pregnancy that may increase the risk of neural tube defects.
- Folic Acid Supplementation: Research continues to emphasize the importance of folic acid supplementation in preventing anencephaly and other NTDs. Studies may explore optimal dosages, timing, and methods of supplementation to maximize its protective effect.
- Preconception Care: Advancements in preconception care and counseling aim to provide women with the information and resources they need to reduce the risk of anencephaly before becoming pregnant.
- Prenatal Diagnosis: Improvements in prenatal screening and diagnostic methods, such as ultrasound and genetic testing, may enhance the accuracy and early detection of anencephaly, allowing for better counseling and decision-making for parents.
- Ethical and Counseling Support: Research focuses on the psychological and emotional aspects of anencephaly, including the development of support systems and resources to help parents and families cope with the diagnosis and its challenges.
- Public Health Initiatives: Public health campaigns and policies promoting folic acid awareness and supplementation continue to be a crucial part of preventing anencephaly and other NTDs on a broader scale.
- Stem Cell and Regenerative Medicine: While there are currently no curative treatments for anencephaly, research in regenerative medicine and stem cell therapy may hold potential for future interventions aimed at repairing or replacing damaged neural tissue. However, these approaches are in the experimental stage and face significant scientific and ethical challenges.
FAQs:
What is anencephaly?
Anencephaly is a severe and rare congenital birth defect in which a major portion of the baby’s brain and skull is underdeveloped or missing. It is a type of neural tube defect (NTD) that occurs during early fetal development.
What causes anencephaly?
The exact causes of anencephaly are not fully understood, but it is believed to result from a combination of genetic and environmental factors. Folic acid deficiency is a well-known risk factor.
How is anencephaly diagnosed during pregnancy?
Anencephaly can be diagnosed through prenatal screening methods, including ultrasound imaging and maternal serum alpha-fetoprotein (AFP) testing. Diagnostic procedures like amniocentesis and chorionic villus sampling (CVS) may also be used.
What is the prognosis for infants with anencephaly?
The prognosis for infants with anencephaly is extremely poor. Most are stillborn, and those who are born alive typically do not survive for more than a few hours or days after birth.
Is anencephaly treatable or curable?
There is currently no cure or effective treatment for anencephaly. Medical care primarily focuses on providing palliative care to keep the infant comfortable during their brief life.
How can anencephaly be prevented?
Anencephaly can be prevented to some extent by ensuring that women of childbearing age take folic acid supplements before and during early pregnancy. Adequate folic acid intake significantly reduces the risk of neural tube defects, including anencephaly.
What are the emotional and ethical considerations for parents with anencephalic pregnancies?
Parents faced with anencephaly often need emotional support and counseling to make difficult decisions regarding the continuation of the pregnancy and to prepare for the challenges they may face. Ethical considerations may vary among individuals and cultures.
Are there support groups or organizations for families affected by anencephaly?
Yes, there are support groups and organizations that provide information, counseling, and emotional support to parents and families affected by anencephaly. These groups can offer valuable resources and connect families with others who have experienced similar situations.
Is research being conducted to better understand anencephaly and develop treatments?
Yes, ongoing research aims to improve our understanding of anencephaly, identify risk factors, and explore potential preventive measures and treatments. While there are no current treatments, research continues to advance in this field.
Can anencephaly be detected before birth, and what options do parents have if it is diagnosed?
Yes, anencephaly can often be detected through prenatal screening methods. When diagnosed, parents have options to consider, including continuing the pregnancy with palliative care, terminating the pregnancy, or participating in research studies, depending on individual circumstances and personal beliefs.
conclusion:
In conclusion, anencephaly is a devastating congenital birth defect characterized by the severe underdevelopment or absence of the brain and skull during fetal development. With a prognosis that is almost universally fatal shortly after birth, anencephaly presents profound emotional and ethical challenges for affected families. While ongoing research seeks to better understand its causes and explore prevention strategies, the most effective current measure is the early and consistent supplementation of folic acid in women of childbearing age. Compassionate care, counseling, and support for parents facing this diagnosis are crucial, recognizing the difficult decisions they may need to make regarding the pregnancy and end-of-life care for their affected child.