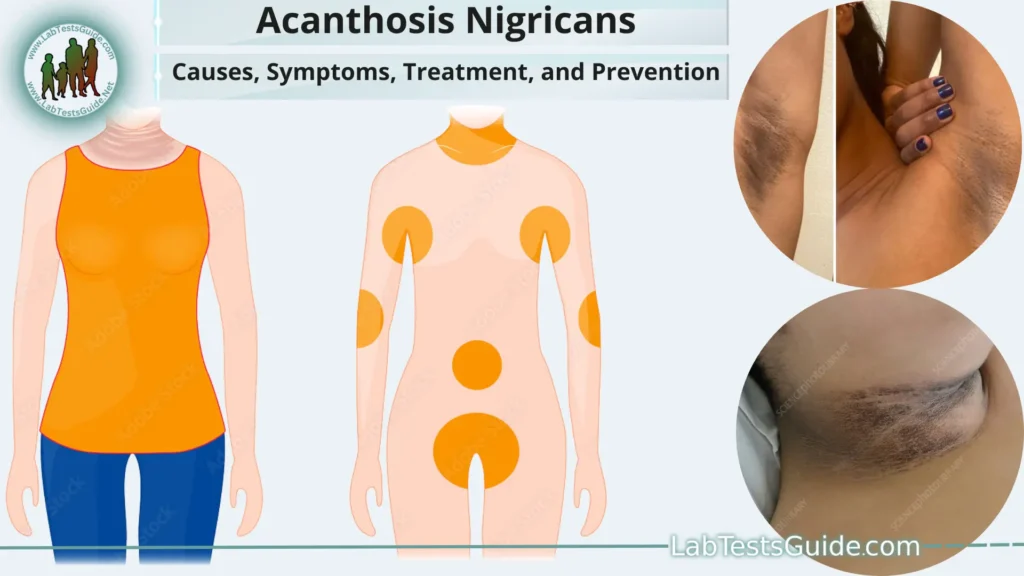
Acanthosis nigricans is a skin condition characterized by dark, thickened patches of skin that may feel velvety or rough to the touch. It primarily affects the folds and creases of the skin, such as the armpits, neck, groin, and sometimes other areas of the body.
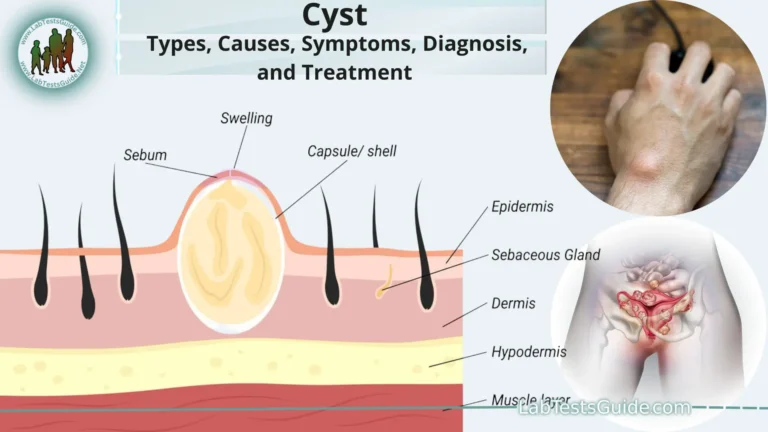
What is Acanthosis Nigricans?
Acanthosis nigricans is a skin condition characterized by dark, thickened patches of skin that may appear velvety or rough. These patches typically develop in areas where the skin folds or creases, such as the neck, armpits, groin, and sometimes the knuckles, elbows, knees, and face. The affected skin may have a tan, brown, or black coloration, and its texture might resemble velvet or have a wart-like appearance.
The primary feature of acanthosis nigricans is the hyperpigmentation and thickening of the skin. The affected areas may not cause any physical discomfort, but they can be cosmetically distressing for some individuals. In most cases, acanthosis nigricans is not harmful itself, but it is often considered a cutaneous marker or a visible sign of an underlying health condition.
Causes and Risk Factors:
- Insulin Resistance: The most common cause of acanthosis nigricans is insulin resistance. When the body’s cells do not respond adequately to insulin, the pancreas produces more insulin to compensate. High levels of insulin in the bloodstream can lead to skin changes, including the thickening and darkening of certain areas.
- Obesity: A significant risk factor for developing acanthosis nigricans is obesity. Excess body fat is associated with insulin resistance, and the condition is more prevalent in individuals with a higher body mass index (BMI).
- Type 2 Diabetes: Acanthosis nigricans is frequently seen in people with type 2 diabetes, as it is often linked to insulin resistance and metabolic abnormalities related to diabetes.
- Polycystic Ovary Syndrome (PCOS): PCOS is a hormonal disorder in women that can be associated with insulin resistance. Women with PCOS may develop acanthosis nigricans due to the hormonal and metabolic imbalances.
- Medications: Some medications have been linked to the development of acanthosis nigricans. Examples include high-dose niacin, oral contraceptives, corticosteroids, and some other drugs.
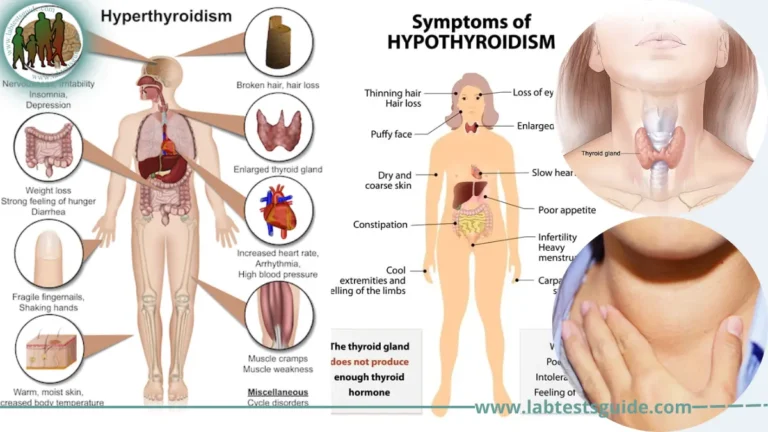
- Endocrine Disorders: Certain hormonal imbalances or endocrine disorders, such as Cushing’s syndrome and hypothyroidism, can be associated with acanthosis nigricans.
- Genetic Factors: While rare, there are some instances of familial acanthosis nigricans, suggesting a genetic predisposition to the condition.
Risk Factors for Acanthosis Nigricans:
- Obesity: Being overweight or obese is a significant risk factor for developing acanthosis nigricans, especially in children and adolescents.
- Family History: If there is a family history of acanthosis nigricans or related conditions, there might be a higher risk of developing the condition.
- Ethnicity: Acanthosis nigricans can occur in people of any ethnicity, but it is more common in individuals of African, Hispanic, or Native American descent.
- Age and Gender: Acanthosis nigricans can affect people of all ages, but it is more frequently seen in children, adolescents, and young adults. It can occur in both males and females.
- Underlying Health Conditions: Certain medical conditions, such as type 2 diabetes, PCOS, and endocrine disorders, increase the risk of developing acanthosis nigricans.
- Medication Use: Some medications, as mentioned earlier, can be associated with acanthosis nigricans, so their use may elevate the risk in certain individuals.
Understanding Insulin Resistance:
Key aspects of understanding insulin resistance include.
Insulin and Glucose Regulation:
- After a meal, blood sugar levels rise, prompting the pancreas to release insulin.
- Insulin signals cells throughout the body, such as muscle, fat, and liver cells, to take up glucose from the blood.
- The absorbed glucose is used for energy production or stored as glycogen in the liver and muscles.
Causes of Insulin Resistance:
- Obesity: Excess body fat, particularly visceral fat around organs, is strongly linked to insulin resistance. Adipose tissue releases various hormones and inflammatory molecules that can impair insulin signaling.
- Sedentary Lifestyle: Physical inactivity and a lack of exercise can contribute to insulin resistance.
- Genetics: Some individuals may have a genetic predisposition to developing insulin resistance.
- Hormonal Imbalances: Conditions like polycystic ovary syndrome (PCOS) can be associated with insulin resistance.
Implications of Insulin Resistance:
- Type 2 Diabetes: Insulin resistance is a significant risk factor for type 2 diabetes. Over time, the pancreas may struggle to produce enough insulin to compensate for the resistance, leading to high blood sugar levels.
- Metabolic Syndrome: Insulin resistance is a central feature of metabolic syndrome, a cluster of conditions that include high blood pressure, high blood sugar, abnormal cholesterol levels, and abdominal obesity.
- Cardiovascular Health: Insulin resistance is associated with an increased risk of cardiovascular diseases, such as heart disease and stroke.
Diagnosis and Assessment:
- Fasting Blood Glucose Test: Measures blood sugar levels after an overnight fast to assess glucose control.
- Oral Glucose Tolerance Test (OGTT): Evaluates how the body responds to a glucose challenge by measuring blood sugar levels over time.
- Hemoglobin A1c (HbA1c) Test: Reflects average blood sugar levels over the past few months.
Management of Insulin Resistance:
- Lifestyle Changes: A combination of regular exercise, a balanced diet, and weight management can improve insulin sensitivity.
- Medications: Some medications, such as metformin, may be prescribed to help manage insulin resistance and blood sugar levels.
- Treatment of Underlying Conditions: Addressing any underlying medical conditions contributing to insulin resistance, such as PCOS, can be beneficial.
Symptoms and Clinical Presentation:
Here are some key aspects of its symptoms and clinical presentation.
Skin Changes:
- Dark, Thickened Patches: Acanthosis nigricans typically appears as dark brown to black, velvety, and thickened patches of skin. The affected areas may feel rough or may have a wart-like appearance.
- Common Locations: The most common areas affected by acanthosis nigricans include the back of the neck, armpits, groin, and skin folds around the abdomen. It can also occur on the elbows, knees, and face in some cases.
- Gradual Progression: Acanthosis nigricans usually develops slowly over time. In the early stages, the skin changes may be subtle, but they can become more noticeable and extensive with time if the underlying cause is not addressed.
- Non-Painful and Non-Itchy: The affected skin is typically not painful or itchy. In most cases, individuals with acanthosis nigricans do not experience physical discomfort related to the skin changes.
Associated Conditions:
- Insulin Resistance and Diabetes: Acanthosis nigricans is often associated with insulin resistance, which is a key feature of type 2 diabetes. Therefore, individuals with the skin condition may have an increased risk of developing diabetes.
- Obesity: Acanthosis nigricans is commonly seen in individuals who are overweight or obese, especially when accompanied by insulin resistance.
- Polycystic Ovary Syndrome (PCOS): Women with PCOS, a hormonal disorder, may also have acanthosis nigricans due to insulin resistance.
- Psychological Impact: While acanthosis nigricans itself is not harmful, the cosmetic appearance of the skin changes can lead to self-consciousness and emotional distress in some individuals.
Diagnosing Acanthosis Nigricans:
Here are the steps involved in diagnosing acanthosis nigricans.
Physical Examination:
- The healthcare professional will examine the affected skin areas, looking for dark, thickened patches with a velvety texture.
- They will check common locations such as the neck, armpits, groin, and skin folds for characteristic skin changes.
- The healthcare professional may also examine other parts of the body, such as the elbows, knees, and face, to determine the extent of the condition.
Medical History Review:
- The healthcare provider will ask about your medical history, including any previous diagnoses of diabetes, insulin resistance, or other endocrine disorders.
- They may inquire about any family history of acanthosis nigricans or related conditions.
Assessment of Underlying Causes:
- Since acanthosis nigricans is often associated with underlying health conditions like insulin resistance, diabetes, and PCOS, the healthcare professional will assess for signs of these conditions.
- They may inquire about symptoms like increased thirst, frequent urination, unexplained weight gain, or irregular menstrual cycles.
Blood Tests:
- Blood tests can help in evaluating blood sugar levels, insulin levels, and other metabolic markers.
- Fasting blood glucose test: Measures blood sugar levels after an overnight fast.
- Oral Glucose Tolerance Test (OGTT): Assesses how the body processes glucose after ingesting a specific amount of sugar.
- Hemoglobin A1c (HbA1c) test: Reflects average blood sugar levels over the past few months.
Screening for Underlying Conditions:
- Depending on the findings from the physical examination and blood tests, the healthcare professional may screen for other conditions related to insulin resistance or hormonal imbalances, such as PCOS.
Biopsy (in some cases):
- In rare cases, a skin biopsy may be performed to confirm the diagnosis. A small sample of the affected skin is taken and examined under a microscope to evaluate the skin changes.
Underlying Medical Conditions:
Here are some of the common underlying medical conditions associated with acanthosis nigricans.
Insulin Resistance and Type 2 Diabetes:
- Insulin resistance, characterized by the body’s reduced response to insulin, is a significant cause of acanthosis nigricans.
- Individuals with insulin resistance may have elevated blood sugar levels, and if left untreated, it can progress to type 2 diabetes.
- Proper management of blood sugar levels through lifestyle changes and, if necessary, medications is crucial for improving acanthosis nigricans in these cases.
Obesity:
- Acanthosis nigricans is commonly seen in individuals who are overweight or obese, particularly when associated with insulin resistance.
- Weight loss and lifestyle modifications, such as adopting a balanced diet and engaging in regular physical activity, can help improve the condition in obese individuals.
Polycystic Ovary Syndrome (PCOS):
- PCOS is a hormonal disorder that affects women and is associated with insulin resistance and hyperandrogenism (elevated male hormone levels).
- Acanthosis nigricans can be seen in women with PCOS, and managing the hormonal imbalances and insulin resistance is essential for skin improvement.
Endocrine Disorders:
- Certain endocrine disorders, such as Cushing’s syndrome (excess cortisol production) and hypothyroidism (underactive thyroid), can be associated with acanthosis nigricans.
- Treating the underlying endocrine condition is important to address the skin changes effectively.
Medication-Induced Acanthosis Nigricans:
- Some medications, such as oral contraceptives, corticosteroids, high-dose niacin, and certain other drugs, have been linked to the development of acanthosis nigricans.
- In such cases, the healthcare professional may consider alternative medications or adjust the dosage to improve the skin condition.
Gastrointestinal Tumors (Rarely):
- In rare instances, acanthosis nigricans can be associated with certain gastrointestinal tumors, particularly adenocarcinomas, located in the stomach, colon, or other parts of the gastrointestinal tract.
- It is essential to rule out the presence of tumors when evaluating a patient with acanthosis nigricans, especially if there is a sudden onset of skin changes.
Familial Acanthosis Nigricans (Rarely):
- In rare cases, acanthosis nigricans may be hereditary and run in families, suggesting a genetic component.
Acanthosis Nigricans in Children and Adolescents:
Here are some key points about acanthosis nigricans in children and adolescents.
- Association with Obesity: Acanthosis nigricans is commonly observed in children and adolescents who are overweight or obese. Excess body weight, especially with central adiposity (abdominal fat), is strongly linked to insulin resistance, which is a significant cause of acanthosis nigricans.
- Insulin Resistance and Type 2 Diabetes Risk: Children and adolescents with acanthosis nigricans are at an increased risk of developing insulin resistance and type 2 diabetes later in life. The condition can be an early indicator of metabolic disturbances and serves as a warning sign for potential health issues.
- Precursor to Metabolic Syndrome: Acanthosis nigricans in children and adolescents may be associated with other components of metabolic syndrome, such as high blood pressure, dyslipidemia (abnormal cholesterol levels), and impaired glucose tolerance. These factors collectively increase the risk of cardiovascular disease.
- Polycystic Ovary Syndrome (PCOS) in Adolescent Females: In teenage girls, acanthosis nigricans can be associated with PCOS, a hormonal disorder characterized by irregular menstrual cycles, ovarian cysts, and insulin resistance. Early detection and management are essential to address PCOS-related symptoms and potential long-term health consequences.
- Psychological Impact: Acanthosis nigricans can affect a child or adolescent’s self-esteem and body image, leading to emotional distress. It may result in lowered self-confidence and social withdrawal. Addressing the underlying condition and providing support can help alleviate these concerns.
- Lifestyle Modifications: The primary approach to managing acanthosis nigricans in children and adolescents involves lifestyle modifications. Encouraging regular physical activity, promoting a balanced and healthy diet, and achieving and maintaining a healthy weight are crucial for improving insulin sensitivity and resolving the skin changes.
- Medical Evaluation: If acanthosis nigricans is suspected in a child or adolescent, it is essential to seek medical evaluation from a healthcare professional, such as a pediatrician or dermatologist. The healthcare provider will perform a physical examination, assess the child’s medical history, and may conduct blood tests to evaluate blood sugar levels and other metabolic markers.
- Early Intervention: Detecting acanthosis nigricans early in life allows for timely intervention to prevent the progression of metabolic disturbances. Lifestyle modifications and appropriate management of any underlying conditions can lead to improved outcomes.
Treatment Options:
Here are the main treatment options for acanthosis nigricans.
Lifestyle Modifications:
- Weight Management: For individuals who are overweight or obese, achieving and maintaining a healthy weight is essential. Weight loss can improve insulin sensitivity and may lead to a reduction in the severity of acanthosis nigricans.
- Balanced Diet: Adopting a balanced and nutritious diet, rich in fruits, vegetables, whole grains, and lean proteins, can support overall health and improve metabolic function.
- Physical Activity: Regular exercise can help improve insulin sensitivity and aid in weight management. Engaging in moderate-intensity physical activities, such as walking, swimming, or cycling, is beneficial.
Managing Underlying Health Conditions:
- Insulin Resistance and Diabetes: If acanthosis nigricans is associated with insulin resistance or type 2 diabetes, blood sugar management is crucial. This may involve lifestyle changes, such as dietary modifications and exercise, and, in some cases, the use of medications prescribed by a healthcare professional.
- Polycystic Ovary Syndrome (PCOS): In cases where acanthosis nigricans is linked to PCOS, the management of the hormonal disorder is essential. Treatments may include oral contraceptives, anti-androgen medications, and lifestyle modifications.
Topical Treatments:
- In some cases, dermatologists may prescribe topical treatments to improve the appearance of acanthosis nigricans.
- Topical retinoids or vitamin D analogs can be applied to the affected areas to help reduce the thickness and hyperpigmentation of the skin.
Medications:
- In cases where lifestyle modifications are not sufficient to manage insulin resistance or related conditions, healthcare professionals may prescribe medications such as metformin to improve insulin sensitivity and regulate blood sugar levels.
Surgical and Procedural Interventions (in rare cases):
- In specific situations, dermatologists may consider surgical or procedural interventions to address acanthosis nigricans, especially in cases where it causes significant discomfort or cosmetic concerns.
- Procedures such as laser therapy or chemical peels may be used to improve the appearance of affected skin.
Prevention and Lifestyle Tips:
Here are some prevention and lifestyle tips to consider.
Maintain a Healthy Weight:
- Aim to achieve and maintain a healthy weight through a balanced diet and regular physical activity.
- If you are overweight or obese, gradual weight loss can improve insulin sensitivity and reduce the severity of acanthosis nigricans.
Adopt a Balanced Diet:
- Focus on a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats.
- Limit the consumption of sugary and processed foods, as well as high-calorie snacks and beverages.
Limit Sedentary Behavior:
- Minimize prolonged periods of sitting or inactivity. Take breaks to stand, stretch, or walk around, especially if you have a sedentary job or lifestyle.
Manage Underlying Health Conditions:
- If you have been diagnosed with insulin resistance, type 2 diabetes, PCOS, or any other underlying condition associated with acanthosis nigricans, follow your healthcare provider’s recommended treatment plan.
- Take prescribed medications as directed and make necessary lifestyle adjustments to manage the condition effectively.
Seek Professional Evaluation:
- If you notice any skin changes, especially dark, thickened patches in skin folds, consult a healthcare professional, preferably a dermatologist.
- Early detection and intervention can lead to better outcomes and prevent complications.
Stay Informed and Educated:
- Stay informed about the risk factors and potential complications of acanthosis nigricans.
- Educate yourself about proper nutrition, exercise, and healthy lifestyle habits to promote overall well-being.
Coping with Acanthosis Nigricans:
Here are some strategies for coping with acanthosis nigricans.
Education and Understanding:
Educate yourself about acanthosis nigricans, its causes, and associated conditions. Understanding the condition can help reduce anxiety and fear.
Learn about lifestyle changes and medical management options available to improve the skin changes and underlying health issues.
Seek Professional Support:
- Consult with a dermatologist or healthcare professional to receive a proper diagnosis and personalized treatment plan.
- If acanthosis nigricans is associated with underlying health conditions, work closely with healthcare providers to manage those conditions effectively
Emotional Support:
- Share your concerns and feelings with friends, family, or a support group. Talking about your experiences can provide emotional relief and reduce isolation.
- Seek support from mental health professionals if the skin changes significantly impact your self-esteem or emotional well-being.
Body Positivity:
- Focus on body positivity and self-acceptance. Remember that everyone’s body is unique, and skin changes do not define your worth as a person.
- Celebrate and appreciate your body for its strength and resilience.
Wear Comfortable Clothing:
- Choose comfortable clothing that does not cause irritation or friction on the affected areas. Avoid tight-fitting clothes that may exacerbate the condition
Sun Protection:
- Protect your skin from excessive sun exposure, as UV rays can worsen hyperpigmentation. Wear sunscreen with broad-spectrum protection and use protective clothing when outdoors.
Avoid Harsh Skin Products:
- Refrain from using harsh chemicals or exfoliants on the affected skin, as they may cause further irritation.
Camouflage Makeup:
- Some individuals may find comfort in using cosmetic products to camouflage the appearance of acanthosis nigricans. Dermatologist-approved makeup can help conceal the skin changes.
Focus on Overall Health:
- Prioritize your overall health through a balanced diet, regular exercise, and stress management techniques.
- Taking care of your physical and emotional well-being can positively impact how you cope with the condition.
FAQs:
Is acanthosis nigricans a contagious skin condition?
No, acanthosis nigricans is not contagious. It is a skin condition that develops due to various underlying factors, such as insulin resistance, obesity, or hormonal imbalances. It cannot be transmitted from one person to another.
Can acanthosis nigricans be cured completely?
Acanthosis nigricans can improve or resolve completely with appropriate management of the underlying cause. For example, if it is associated with insulin resistance or diabetes, controlling blood sugar levels through lifestyle changes and medications can lead to improvement in the skin changes.
Is acanthosis nigricans always linked to diabetes?
Acanthosis nigricans is commonly associated with insulin resistance, which is a hallmark of type 2 diabetes. However, it can also be linked to other conditions like polycystic ovary syndrome (PCOS), obesity, certain medications, and endocrine disorders.
Can acanthosis nigricans affect any age group?
Acanthosis nigricans can affect individuals of all ages, but it is more commonly seen in children, adolescents, and young adults. It can also occur in older adults and may be associated with certain health conditions.
Can acanthosis nigricans go away on its own without treatment?
In some cases, acanthosis nigricans may improve or resolve on its own if the underlying cause is addressed. For example, if the condition is related to weight loss, managing obesity can lead to improvement. However, in many cases, proper treatment and management are necessary for significant improvement.
How is acanthosis nigricans different from skin cancer?
Acanthosis nigricans is a benign skin condition caused by various factors like insulin resistance, whereas skin cancer is the abnormal growth of skin cells that can be malignant. While acanthosis nigricans is not harmful itself, skin cancer requires immediate medical attention and appropriate treatment.
Can acanthosis nigricans affect any part of the body?
Acanthosis nigricans typically appears in skin folds and creases, such as the back of the neck, armpits, and groin. It can also affect other areas like the elbows, knees, face, and abdomen in some cases.
Can acanthosis nigricans be prevented?
Acanthosis nigricans can often be prevented or managed effectively through lifestyle changes, such as maintaining a healthy weight, adopting a balanced diet, and engaging in regular physical activity. Early detection and management of underlying health conditions are also crucial for prevention and improvement.
Can acanthosis nigricans come back after treatment?
If the underlying cause of acanthosis nigricans is not properly managed, the skin changes may recur. Consistent management of the underlying condition, lifestyle changes, and regular follow-ups with healthcare professionals can help prevent recurrence.
Can cosmetic procedures completely remove the skin changes caused by acanthosis nigricans?
Cosmetic procedures, such as laser therapy or chemical peels, may improve the appearance of the skin affected by acanthosis nigricans. However, complete removal may not always be possible, especially if the underlying cause is not adequately addressed. The focus of treatment is primarily on managing the underlying condition rather than cosmetic removal.
Conclusion:
In conclusion, acanthosis nigricans is a skin condition characterized by dark, thickened patches of skin, commonly found in skin folds and creases. It is often associated with underlying factors such as insulin resistance, obesity, and hormonal imbalances. A thorough evaluation by a healthcare professional, preferably a dermatologist, is crucial for accurate diagnosis and to identify any related health conditions. Treatment options include lifestyle modifications, medical management of underlying conditions, and sometimes topical treatments. While acanthosis nigricans itself is harmless, addressing the underlying causes is essential for improving or resolving the skin changes. Additionally, seeking emotional support, practicing body positivity, and maintaining a healthy lifestyle can aid in coping with the condition and promoting overall well-being.