More than a year after the emergence of SARS-CoV-2, the virus that causes COVID-19, researchers are beginning to better understand some of the short- and long-term effects that the disease can have on the body. … One such effect commonly found among COVID-19 patients with varying degrees of severity is an increase in blood D-dimer levels.
D-dimer is a protein made when blood clots form and then break down. An elevated level of D-dimer in the blood may be a sign of increased blood clotting in the body.
The D-dimer protein fragment is usually undetectable in the blood or is found at low levels that increase slightly with age. However, if the body does not actively form clots and does not break down already formed blood clots, the level of D-dimer in the blood should be below the threshold values for a certain age.
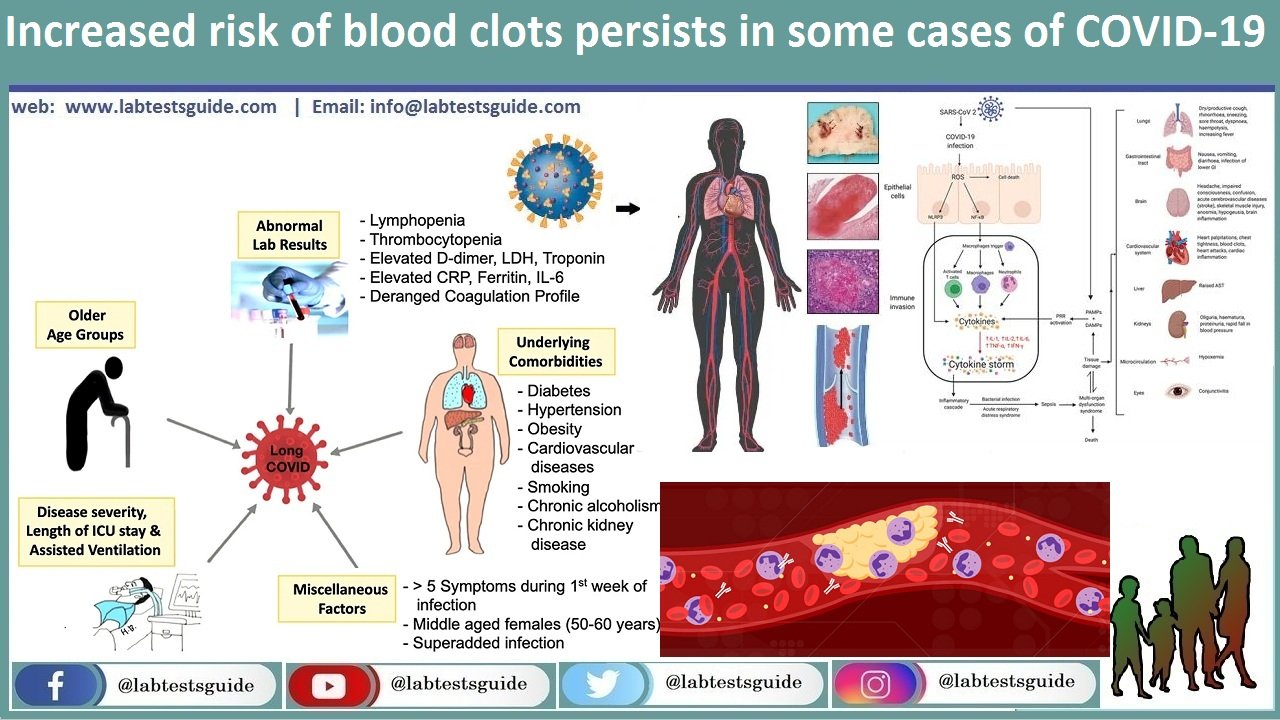
Conversely, elevated D-dimer levels may indicate increased blood clotting, which is part of the body’s natural response to inflammation and damage to blood vessels or tissues. Increased blood clotting can lead to complications such as deep vein thrombosis (DVT), pulmonary embolism (PE), heart attack, and stroke. The elevated D-dimer levels seen in some patients with severe COVID-19 may indicate an increased risk of blood clots and complications. Undetected and untreated blood clots can contribute to poor outcomes and have been fatal in some cases of severe COVID-19.
Recently, a team of scientists studied the effects of persistent COVID-19, commonly referred to as Long COVID-19, and its relationship to inflammation and blood clotting. Some patients experience persistent symptoms such as fatigue, shortness of breath, and lack of stamina, even after the acute illness has subsided. Researchers followed 150 COVID-19 patients who were treated at St James’s Hospital in Dublin from May to September 2020 for an average of 80 days after they were first diagnosed. Their report, published in the Journal of Thrombosis and Hemostasis, found that D-dimer levels remained elevated in about 25% of study participants for up to four months after being diagnosed with COVID-19. Elevated D-dimer levels were most often found in hospitalized patients with severe illness and in patients aged 50 and over.
Data collection is ongoing regarding elevated D-dimer levels in patients with varying severity of COVID-19. The current recommendation suggests that D-dimer levels be monitored even after hospital discharge with COVID-19, as it is not known how long the increased risk of blood clotting persists and when it will go away. There is also speculation that the likelihood of an increased risk of blood clots – like the severity of COVID-19 – may increase depending on the underlying health conditions associated with the patient. Examples of such underlying conditions include, but are not limited to, cancer, bodily injury such as fracture or surgery, autoimmune disorders, and heart failure.
Although elevated D-dimer levels are commonly found among COVID-19 patients, there is no evidence to explain how or why this increase occurs. It is also unclear why these levels become increasingly high in severely diagnosed COVID-19 patients and why the increase persists in some patients. The study authors are calling for more research to better understand the effects of long-term COVID-19. Determining why D-dimer levels remain elevated can help understand why some patients suffer from long-term COVID-19 and can be informative for how to effectively manage and treat these patients.
Related Articles:
Sources
(April 8, 2021) Southall, Jennifer. Elevated D-dimer levels common months after COVID-19 diagnosis. Healio, Hematology/Oncology. Accessed May 1, 2021. https://www.healio.com/news/hematology-oncology/20210408/elevated-ddimer-levels-common-months-after-covid19-diagnosis
Townsend L, et al. Prolonged elevation of D‐dimer levels in convalescent COVID‐19 patients is independent of the acute phase response. J Thromb Haemost. 2021; doi:10.1111/jth.15267.
(January 29, 2021) COVID-19 and Coagulopathy: Frequently Asked Questions. American Society of Hematology. Accessed May 1, 2021. https://www.hematology.org/covid-19/covid-19-and-coagulopathy






