Are you preparing for a medical laboratory certification exam or enhancing your microbiology skills? This free mock test on Analytic Procedures for Bacteriology is specifically designed for laboratory technologists, technicians, and students who want to test their knowledge in bacterial identification, biochemical testing, culture methods, and rapid diagnostic techniques.
This practice test includes multiple-choice questions (MCQs) with detailed answers, making it ideal for candidates appearing in ASCP MLS, AMT MLT, AIMS, CSMLS, IBMS, HAAD, DHA, and MOH exams .
✅ About this Mock Test This Analytic Procedures for Bacteriology Mock Test is created to simulate real exam scenarios. It covers key areas of bacteriological analysis, including:
Gram staining and bacterial classification Culture and selective media techniques Biochemical tests for bacterial differentiation Rapid identification methods Antimicrobial susceptibility testing The questions are designed to strengthen your understanding of laboratory diagnostic procedures and improve your problem-solving skills in clinical microbiology.
🧪 Why Take This Test? Helps you assess your knowledge of bacteriology lab procedures. Covers important exam topics frequently asked in certification tests. Enhances critical thinking and decision-making skills for laboratory work. Provides instant learning feedback with correct answers and explanations. 📋 Instructions: Use this test as a self-assessment tool for your microbiology exam preparation.four possible options , only one is correct .
Report a question
ASCP MLS Exam MCQs Chapter 16
Test your microbiology knowledge with our free Analytic Procedures for Bacteriology Mock Test . This practice quiz includes 118 multiple-choice questions (MCQs) with answers, covering Gram staining, culture techniques, biochemical tests, rapid identification methods, and antimicrobial susceptibility testing. Ideal for ASCP MLS, AMT MLT, AIMS, CSMLS, IBMS, HAAD, DHA, and MOH exam preparation.
🔹 Simulate the Real Exam : Beat test-day nerves with timed conditions.Track Your Progress : Review performance analytics to identify strengths and weaknesses.Master Time Management : Sharpen your pacing skills under pressure.Learn from Mistakes : Detailed answer explanations help you refine your understanding.
Ideal for final readiness checks , this mock test ensures you walk into the exam prepared, confident, and ready to excel! 🚀
1 / 118
Category:
ASCP Exam Questions
A Gram stain of urethral discharge shows gram-negative intracellular diplococci. The most likely organism is:
Neisseria gonorrhoeae is the classic cause of urethral discharge with:
Gram-negative intracellular diplococci : Kidney-shaped pairs within neutrophils on Gram stain.
Clinical context : Purulent discharge, dysuria; may progress to PID or disseminated infection.
Why Not the Others?
(a) Acinetobacter baumannii : Gram-negative coccobacilli (environmental, not sexually transmitted).
(c) Haemophilus ducreyi : Gram-negative rods/chains (causes chancroid, a genital ulcer disease).
(d) Escherichia coli : Gram-negative rods (UTIs, not urethritis with diplococci).
2 / 118
Category:
ASCP Exam Questions
Which test detects bacterial ability to decarboxylate amino acids such as lysine or ornithine?
The lysine decarboxylase test (and similar tests for ornithine or arginine ) detects bacterial enzymes that remove carboxyl groups (–COOH) from amino acids, producing amines (e.g., cadaverine from lysine) and CO₂ .
Positive result : The medium turns alkaline (purple) due to amine production, even after initial acidic fermentation (yellow).
Negative result : The medium remains yellow (no decarboxylation).
Key Uses: Why Not the Other Options? b) Citrate test : Detects citrate utilization (e.g., Klebsiella [+], E. coli [–]).
c) Gelatin hydrolysis : Tests for gelatinase (e.g., Serratia , Pseudomonas ).
d) Oxidase test : Identifies cytochrome c oxidase (e.g., Pseudomonas , Neisseria ).
3 / 118
Category:
ASCP Exam Questions
Which of the following media is specifically used to detect hemolytic patterns of bacteria?
Blood agar is the medium specifically used to detect hemolytic patterns of bacteria, as it contains 5% sheep or horse blood , allowing observation of:
Beta-hemolysis : Complete lysis of RBCs → clear zones around colonies (e.g., Streptococcus pyogenes ).
Alpha-hemolysis : Partial lysis → greenish discoloration (e.g., Streptococcus pneumoniae ).
Gamma-hemolysis : No hemolysis (e.g., Enterococcus faecalis ).
Why Not Other Options? (a) MacConkey agar : Selects for Gram-negatives and differentiates lactose fermenters (pink colonies) vs. non-fermenters.
(c) EMB agar : Selective for Gram-negatives; identifies E. coli (metallic green sheen).
(d) Citrate agar : Tests citrate utilization (e.g., Klebsiella vs. E. coli ).
4 / 118
Category:
ASCP Exam Questions
Selective culture media are primarily designed to:
Selective media contain specific components (e.g., antibiotics, salts, or dyes) that:
Suppress unwanted bacteria (e.g., Gram-positives, contaminants).
Promote the growth of target organisms (e.g., pathogens from mixed samples).
Key Examples: MacConkey agar :
Mannitol Salt Agar (MSA) :
Why Not the Others? a) Motility : Requires motility agar (stab inoculation), not selective media.
c) Hemolysis : Detected with blood agar (differential, not selective).
d) Antimicrobial resistance : Tested via Kirby-Bauer disk diffusion or MIC assays , not selective media.
6 / 118
Category:
ASCP Exam Questions
Which test detects bacterial ability to degrade gelatin into amino acids?
The gelatin hydrolysis test detects a bacterium’s ability to produce gelatinase , an enzyme that degrades gelatin (a protein) into amino acids .
Other options:
(a) DNase test → Detects breakdown of DNA (clearing around colonies on DNase agar).
(c) Urease test → Detects urea hydrolysis (turns pink if positive, e.g., Proteus ).
(d) Catalase test → Identifies catalase enzyme (bubbles with H₂O₂, e.g., Staphylococcus vs. Streptococcus ).
7 / 118
Category:
ASCP Exam Questions
An organism from a peritoneal abscess grows black colonies on BBE agar and is catalase-positive. The genus is:
Black colonies on Bacteroides Bile Esculin (BBE) agar and catalase-positive are hallmark features of Bacteroides fragilis , the most clinically significant anaerobe in this genus.
BBE agar : Selects for bile-resistant anaerobes; blackening occurs due to esculin hydrolysis .
Catalase-positive : Differentiates Bacteroides from other anaerobes (e.g., Prevotella , Porphyromonas are catalase-negative).
Why Not the Others?
(a) Acidaminococcus : Non-pigmented, catalase-negative, and does not grow on BBE agar.
(c) Porphyromonas : Forms black-pigmented colonies but is catalase-negative and bile-sensitive (no growth on BBE).
(d) Prevotella : May produce black pigment but is catalase-negative and often bile-sensitive.
Clinical Relevance :
Bacteroides fragilis is a major pathogen in intra-abdominal abscesses (e.g., post-surgery, perforated appendicitis).
Resistance : Often produces β-lactamase (treat with metronidazole, carbapenems, or β-lactam/β-lactamase inhibitors).
8 / 118
Category:
ASCP Exam Questions
Which test is used to identify bacteria capable of converting phenylalanine into phenylpyruvic acid?
The phenylalanine deaminase (PDA) test detects the enzyme phenylalanine deaminase , which converts phenylalanine → phenylpyruvic acid .
After incubation, 10% ferric chloride is added, forming a green-colored complex with phenylpyruvic acid (positive result).
Key Organisms Identified: ✔ Proteus , Morganella , and Providencia (rapid PDA-positive).Escherichia coli , Klebsiella , and Salmonella (PDA-negative).
Why Not the Other Tests? b) Citrate test → Checks if bacteria use citrate as a carbon source.
c) Voges-Proskauer (VP) test → Detects acetoin production (e.g., Enterobacter ).
d) Indole test → Identifies tryptophanase activity (e.g., E. coli ).
9 / 118
Category:
ASCP Exam Questions
Anaerobic, box-car shaped, beta-hemolytic gram-positive bacilli from a wound are most likely:
lostridium perfringens is an anaerobic, Gram-positive bacillus with:
“Box-car” morphology : Short, blunt-ended rods.
Beta-hemolysis : Double zone of hemolysis on blood agar (“target hemolysis”).
Rapid growth : Often visible within 6–12 hours.
Why Not the Others?
(a) Actinomyces israelii : Gram-positive, filamentous (not box-car), and non-hemolytic (sulfur granules in pus).
(c) Bacillus subtilis : Aerobic , spore-forming, and environmental (not a wound pathogen).
(d) Eggerthella lenta : Non-spore-forming , non-hemolytic anaerobe (gut flora, rare in wounds).
10 / 118
Category:
ASCP Exam Questions
Which test is performed to detect bacterial ability to hydrolyze esculin in the presence of bile salts?
Detects the ability of bacteria to hydrolyze esculin into esculetin and glucose in the presence of bile salts .
Esculetin reacts with ferric citrate (in the medium) to form a black precipitate , indicating a positive result.
Key Uses: Why Not the Other Options? a) PYR test → Detects pyrrolidonyl arylamidase (used for Enterococcus and Streptococcus pyogenes ).
c) Citrate utilization test → Determines if bacteria can use citrate as a carbon source (e.g., Klebsiella , Enterobacter ).
d) Indole test → Checks for tryptophanase activity (e.g., E. coli is indole-positive).
11 / 118
Category:
ASCP Exam Questions
The Kligler iron agar test is primarily used to detect:
The oxidase test detects the presence of cytochrome c oxidase, an enzyme in the electron transport chain of certain bacteria.
Neisseria spp. (e.g., N. gonorrhoeae , N. meningitidis ) and Pseudomonas spp. (e.g., P. aeruginosa ) are oxidase-positive .
Many other aerobic and facultative anaerobic bacteria (like Vibrio , Campylobacter , and Aeromonas ) also test positive.
Why Not the Other Options? a) Enterobacteriaceae (e.g., E. coli , Salmonella , Klebsiella ) are oxidase-negative .
c) Staphylococcus species and d) Streptococcus species are also oxidase-negative (they use alternative enzymes for respiration).
12 / 118
Category:
ASCP Exam Questions
Which test differentiates Staphylococcus aureus from other Staphylococcus species?
The coagulase test is the key test to differentiate Staphylococcus aureus (pathogenic) from other coagulase-negative staphylococci (e.g., S. epidermidis , S. saprophyticus ).
Why Not the Others? a) Catalase test :
c) Oxidase test :
d) Indole test :
13 / 118
Category:
ASCP Exam Questions
MacConkey agar for screening E. coli O157:H7 must contain:
Sorbitol-MacConkey agar (SMAC) is the standard medium to screen for E. coli O157:H7 because:
Why Not the Others?
(a) Indole : A biochemical test (post-culture), not a component of MacConkey agar.
(b) Citrate : Used in Simmons citrate agar (irrelevant here).
(d) Lactose : Standard MacConkey contains lactose, but E. coli O157:H7 ferments lactose (pink colonies), making it indistinguishable from normal flora without sorbitol differentiation .
14 / 118
Category:
ASCP Exam Questions
The CAMP test is especially useful for identifying:
The CAMP test (Christie–Atkins–Munch-Petersen test) is a specific biochemical assay used to identify Group B Streptococcus (S. agalactiae ) .
How It Works: S. agalactiae produces CAMP factor , a protein that synergizes with Staphylococcus aureus beta-hemolysin .
When streaked perpendicular to S. aureus on blood agar, it creates an arrowhead-shaped zone of enhanced hemolysis (positive result).
Clinical Importance: Group B strep is a leading cause of neonatal sepsis/meningitis and postpartum infections .
The CAMP test is rapid and reliable for screening pregnant women (vaginal/rectal swabs) to prevent transmission during delivery.
Why Not the Others? a) S. pyogenes (Group A strep) : Identified by bacitracin sensitivity or Pyr test .
c) S. aureus : Detected via coagulase test or Mannitol Salt Agar fermentation .
d) N. meningitidis : Diagnosed via oxidase test , glucose/maltose fermentation , or PCR.
15 / 118
Category:
ASCP Exam Questions
A clean-catch urine culture grows >100,000 CFU/mL of a gram-negative bacillus that is indole-positive and urease-positive. The organism is:
The described organism is a gram-negative bacillus that is:
Indole-positive → Rules out Proteus mirabilis (indole-negative).
Urease-positive → Consistent with Proteus , Morganella , and some Providencia species.
>100,000 CFU/mL in urine → Suggests a true urinary tract infection (UTI) pathogen.
Key differentiating factors: Proteus vulgaris : Indole positive , urease positive .
Proteus mirabilis : Indole negative , urease positive .
Morganella morganii : Indole positive , urease variable (often positive).
Providencia stuartii : Indole positive , urease negative .
16 / 118
Category:
ASCP Exam Questions
The presence of bubbles in the catalase test indicates:
The catalase test detects the enzyme catalase , which breaks down hydrogen peroxide (H₂O₂) into water (H₂O) and oxygen gas (O₂) .
Positive result : Immediate bubbling or effervescence (due to O₂ release).
Negative result : No bubbles (lack of catalase).
Key Uses: Why Not the Other Options? b) CO₂ production is detected in carbohydrate fermentation tests (e.g., Durham tube).
c) Indole formation is tested via Kovac’s reagent (tryptophanase activity).
d) Nitrate reductase is detected in the nitrate reduction test .
17 / 118
Category:
ASCP Exam Questions
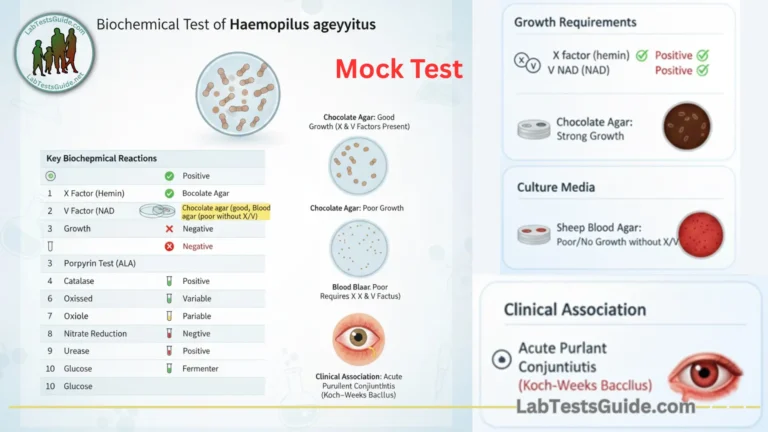
Which organism is typically identified using the X and V factor requirement test?
Key Points: Haemophilus influenzae requires both X and V factors .
Some species (e.g., Haemophilus parainfluenzae ) require only V factor .
The test helps differentiate Haemophilus from other bacteria that may grow on blood agar but do not need these factors.
Why Not the Others? Neisseria – Identified by oxidase test and sugar fermentation.
Corynebacterium – Identified by tellurite agar and biochemical tests.
Streptococcus – Identified by hemolysis patterns and Lancefield grouping.
18 / 118
Category:
ASCP Exam Questions
Copy – The CAMP test produces a characteristic arrowhead hemolysis when the test organism is streaked perpendicular to:
The CAMP test identifies Group B Streptococcus (Streptococcus agalactiae ) by detecting the CAMP factor , a protein that synergistically enhances the beta-hemolysis caused by Staphylococcus aureus ‘s sphingomyelinase (beta-hemolysin) .
When S. agalactiae is streaked perpendicular to S. aureus on sheep blood agar, the CAMP factor intensifies hemolysis , forming a distinct arrowhead-shaped zone at the intersection.
Key Points: ✔ CAMP factor does not cause hemolysis alone—it amplifies S. aureus ‘s beta-hemolysin activity.S. aureus must be streaked first, and the test organism (S. agalactiae ) streaked perpendicularly toward it.
Why Not the Other Options? a) Streptococcus pyogenes → Produces its own hemolysins (streptolysins) but does not interact with the CAMP factor.
c) Enterococcus faecalis → Non-hemolytic or gamma-hemolytic; irrelevant to the CAMP test.
d) Bacillus cereus → Produces hemolysins but does not synergize with the CAMP factor.
19 / 118
Category:
ASCP Exam Questions
Which test determines bacterial ability to use citrate as a sole carbon source?
The citrate utilization test determines if a bacterium can use citrate as its sole carbon source and ammonium salts as its nitrogen source, producing alkaline byproducts.
Positive result : Blue color change (due to pH rise from citrate metabolism, e.g., Klebsiella , Enterobacter ).
Negative result : Green/no change (e.g., E. coli ).
Why Not Other Options? (a) Methyl red test : Detects mixed-acid fermentation (e.g., E. coli vs. Enterobacter ).
(c) Voges-Proskauer test : Identifies acetoin production (e.g., Enterobacter ).
(d) Indole test : Detects tryptophan hydrolysis (e.g., E. coli vs. Klebsiella ).
20 / 118
Category:
ASCP Exam Questions
A vaginal swab shows clue cells. This suggests:
Definition : Clue cells are vaginal epithelial cells that appear stippled or granular under microscopy due to being coated with bacteria (primarily Gardnerella vaginalis ).
Diagnostic Significance :
They are the hallmark of bacterial vaginosis (BV) , the most common vaginal infection in women of reproductive age.
BV is a polymicrobial infection involving G. vaginalis , Mobiluncus spp., and anaerobes (Prevotella , Bacteroides ).
Why Not the Others? a) Candida albicans : Causes vulvovaginal candidiasis (yeast infection), diagnosed by budding yeast/hyphae on KOH prep (no clue cells).
c) Trichomonas vaginalis : Causes trichomoniasis , diagnosed by motile flagellated protozoa on wet mount (no clue cells).
d) Neisseria gonorrhoeae : Diagnosed via NAAT or culture (intracellular gram-negative diplococci); unrelated to clue cells.
21 / 118
Category:
ASCP Exam Questions
Nutritionally variant” streptococci belong to which genera?
Nutritionally variant streptococci (NVS) are fastidious bacteria that require pyridoxal (vitamin B6) or cysteine for growth. They were reclassified into two genera:
Abiotrophia
Granulicatella
These organisms:
Why Not Other Options? (a) Enterococci : Grow on standard media (e.g., Enterococcus faecalis ).
(b) Group D enterococci : Part of Enterococcus genus (not nutritionally fastidious).
(c) Beta-hemolytic streptococci : Grow readily on blood agar (e.g., S. pyogenes ).
22 / 118
Category:
ASCP Exam Questions
Which test is most useful for differentiating Streptococcus pyogenes from other beta-hemolytic streptococci?
Streptococcus pyogenes (Group A β-hemolytic Streptococcus ) is susceptible to bacitracin , meaning it shows a zone of inhibition around a bacitracin disk.
Other β-hemolytic streptococci (e.g., Streptococcus agalactiae – Group B) are typically resistant to bacitracin.
Why Not the Other Options? b) Coagulase test : Used to differentiate Staphylococcus aureus (coagulase-positive) from other staphylococci.
c) Oxidase test : Helps identify Pseudomonas or Neisseria , but streptococci are oxidase-negative.
d) Indole test : Used for gram-negative bacteria (e.g., E. coli ).
23 / 118
Category:
ASCP Exam Questions
A sputum culture grows mucoid, lactose-fermenting colonies. The organism is likely:
Mucoid colonies :
Klebsiella pneumoniae produces thick polysaccharide capsules , creating shiny, mucoid colonies on agar.
This capsule contributes to its virulence and is associated with pneumonia and nosocomial infections .
Lactose fermentation :
K. pneumoniae is a lactose fermenter , forming pink colonies on MacConkey agar (due to acid production).
This differentiates it from non-lactose fermenters like Pseudomonas (a) and Salmonella (d).
Why Not the Others? 24 / 118
Category:
ASCP Exam Questions
The CAMP factor enhances hemolysis caused by which bacterial enzyme?
The CAMP test detects the CAMP factor , produced by Group B Streptococcus (Streptococcus agalactiae) .
This factor enhances hemolysis caused by the β-hemolysin (a hemolysin) produced by Staphylococcus aureus .
When both organisms are streaked perpendicular to each other on blood agar, a characteristic arrowhead-shaped zone of enhanced hemolysis appears at the junction — a positive CAMP test .
Other options: a) Streptolysin O – Hemolysin produced by Streptococcus pyogenes (Group A), but not involved in CAMP test.
b) Beta-lactamase – Enzyme that breaks down β-lactam antibiotics, unrelated to hemolysis.
d) Urease – Breaks down urea; not involved in hemolysis.
25 / 118
Category:
ASCP Exam Questions
Cerebrospinal fluid test results most consistent with viral meningitis include:
Viral meningitis typically shows the following CSF findings :
Cell count : Lymphocytic pleocytosis (WBCs 50–500/μL, predominantly lymphocytes).
Glucose : Normal (≈2/3 of serum glucose).
Protein : Mildly elevated (50–100 mg/dL).
Lactate : Normal (unlike bacterial meningitis, where it’s elevated).
Why Not Other Options? (a) Decreased protein : Rare in meningitis (protein is usually normal/mildly elevated in viral cases).
(b) Increased glucose : Nonspecific; low glucose suggests bacterial/TB/fungal meningitis.
(c) Increased lactate : Suggests bacterial meningitis (due to anaerobic glycolysis).
26 / 118
Category:
ASCP Exam Questions
Legionella pneumophila grows best on which medium?
Legionella pneumophila is a fastidious Gram-negative bacillus that requires:
Buffered charcoal yeast extract (BCYE) agar , enriched with L-cysteine and iron (essential for growth).
pH 6.9 (optimized with ACES buffer).
Incubation : 3–5 days in 5% CO₂ at 35°C.
Why Not the Others?
(a) Thiosulfate citrate bile salts (TCBS) agar : Selective for Vibrio spp. (e.g., V. cholerae ).
(c) MacConkey agar : Does not support Legionella (no cysteine/iron).
(d) Blood agar : Lacks cysteine/iron; Legionella may grow poorly or not at all.
27 / 118
Category:
ASCP Exam Questions
Which test differentiates Streptococcus pneumoniae from viridans streptococci?
The bile solubility test is the key test to differentiate:
Why Not Other Options? (b) Coagulase test : Used for Staphylococcus aureus (irrelevant for streptococci).
(c) Catalase test : All streptococci are catalase-negative (rules out Staphylococcus only).
(d) Oxidase test : Streptococci are oxidase-negative (irrelevant).
Supportive Tests for S. pneumoniae :
28 / 118
Category:
ASCP Exam Questions
The satellite phenomenon, where small colonies grow around Staphylococcus aureus streaks, is characteristic of:
The satellite phenomenon occurs when Haemophilus influenzae (a fastidious bacterium requiring factor V [NAD] and factor X [hemin] for growth) forms small colonies around streaks of Staphylococcus aureus .
This phenomenon is a classic diagnostic clue for identifying H. influenzae in cultures.
Why Not the Other Options? b) Neisseria meningitidis : Requires cystine and iron , not NAD/hemin; no satellite growth.
c) Proteus mirabilis : Swarms on agar but does not depend on S. aureus for growth factors.
d) Escherichia coli : Non-fastidious; grows independently without S. aureus .
29 / 118
Category:
ASCP Exam Questions
Which test is used to differentiate Enterococcus species from non-enterococcal group D streptococci?
The PYR (L-pyrrolidonyl-β-naphthylamide) test is used to differentiate Enterococcus species (PYR-positive) from non-enterococcal Group D streptococci (PYR-negative).
Bile esculin hydrolysis (b) helps identify Group D streptococci (including both Enterococcus and non-enterococcal species).
Growth in 6.5% NaCl (c) is a characteristic of Enterococcus but not all Group D streptococci.
Oxidase test (d) is irrelevant for differentiating these Gram-positive cocci.
30 / 118
Category:
ASCP Exam Questions
A positive oxidase test indicates the presence of which enzyme?
The oxidase test detects the presence of cytochrome c oxidase , a key enzyme in the electron transport chain (ETC) of aerobic respiration.
Positive result (e.g., Pseudomonas , Neisseria ):
Negative result (e.g., Enterobacteriaceae like E. coli ):
Why Not the Others? b) Catalase : Detected via the catalase test (bubbles with H₂O₂).
c) Urease : Detected in the urease test (e.g., Helicobacter pylori turns urea broth pink).
d) Nitrate reductase : Detected via the nitrate reduction test (red color with zinc dust).
32 / 118
Category:
ASCP Exam Questions
Which of the following tests is most useful in differentiating Enterobacteriaceae species?
The Triple Sugar Iron (TSI) agar test is a key biochemical test used to differentiate members of the Enterobacteriaceae family (e.g., E. coli, Salmonella, Shigella, Proteus ). It assesses:
Sugar fermentation (glucose, lactose, sucrose) → Acid production (yellow).
Gas production → Cracks or bubbles in agar.
H₂S production → Black precipitate (e.g., Salmonella, Proteus ).
Why Not the Others? a) Oxidase test : Enterobacteriaceae are oxidase-negative , so this test doesn’t differentiate within the family.
c) Catalase test : Most Enterobacteriaceae are catalase-positive (useful to distinguish from Streptococcus , but not within the group).
d) Spore staining : Enterobacteriaceae do not form spores (only relevant for Bacillus or Clostridium ).
33 / 118
Category:
ASCP Exam Questions
Which rapid test is commonly used to identify beta-hemolytic Group A Streptococcus directly from throat swabs?
The rapid antigen detection test (RADT) is specifically designed for quick identification of Group A Streptococcus (GAS; Streptococcus pyogenes ) directly from throat swabs.
It detects Group A-specific carbohydrate antigens in minutes, allowing for prompt diagnosis and treatment of strep throat.
Key Features: ✔ Fast results (5–15 minutes).High specificity (low false positives).
Why Not the Other Tests? a) Latex agglutination → Used for confirming Group A Strep in culture, not rapid throat swabs.
b) PYR test → Helps differentiate S. pyogenes (PYR-positive) but requires culture isolation first.
d) Coagulase test → Used for Staphylococcus aureus , not streptococci.
34 / 118
Category:
ASCP Exam Questions
The optochin disk is used to differentiate:
Purpose : The optochin (ethylhydrocupreine) disk test differentiates:
S. pneumoniae
Viridans streptococci (resistant, no zone or <14 mm)
Mechanism :
Clinical Utility :
Why Not the Others? a) Staphylococcus vs. Streptococcus : Differentiated by catalase test (Staph = catalase+, Strep = catalase-).
c) E. coli vs. Klebsiella : Distinguished by indole test (E. coli = indole+, Klebsiella = indole-).
d) Pseudomonas vs. Acinetobacter : Differentiated by oxidase test (Pseudomonas = oxidase+, Acinetobacter = oxidase-).
35 / 118
Category:
ASCP Exam Questions
A gram-positive bacillus with “tumbling motility” at 25°C is:
Gram-positive bacillus :
Tumbling motility at 25°C :
Listeria exhibits characteristic tumbling motility when cultured at room temperature (20–25°C) due to its flagella.
Motility is lost at 37°C (unlike most bacteria, which are more motile at body temperature).
Other Features :
Catalase-positive (rules out Streptococcus and Enterococcus ).
Beta-hemolytic on blood agar.
Cold enrichment improves detection from food/clinical samples.
Why Not the Others? a) Bacillus anthracis : Non-motile, forms spores, and is catalase-positive (but no tumbling motility).
b) Corynebacterium diphtheriae : Non-motile , forms metachromatic granules , and has a “picket fence” arrangement.
d) Clostridium botulinum : Anaerobic , forms spores, and produces neurotoxins (no motility at 25°C).
36 / 118
Category:
ASCP Exam Questions
The urease test is useful for differentiating which organism from Escherichia coli?
The urease test detects the enzyme urease , which hydrolyzes urea into ammonia and CO₂ , raising the pH and turning the medium pink/red (due to the pH indicator phenol red).
Proteus species (e.g., P. mirabilis ) are rapid urease-positive , while Escherichia coli is urease-negative .
Why Not the Other Options? a) Klebsiella pneumoniae → Some strains are urease-positive, but this is not the primary differentiating test from E. coli .
c) Pseudomonas aeruginosa → Urease-negative (like E. coli ), so not useful for differentiation.
d) Neisseria meningitidis → Does not produce urease and is not relevant in this context.
37 / 118
Category:
ASCP Exam Questions
A positive “string test” is characteristic of:
Purpose : The string test is a rapid, simple test used to identify Vibrio cholerae Vibrio species.
Procedure :
A loop is mixed with bacterial colonies in saline.
If positive, the mixture forms a viscous “string” (>2 mm) when the loop is pulled away, due to the organism’s capsular polysaccharide or extracellular mucin .
Specificity : While other organisms (e.g., Aeromonas ) may occasionally give a weak string reaction, it is most strongly associated with V. cholerae .
Why Not the Others? b) Campylobacter jejuni – No string test; identified by oxidase+, motility, and microaerophilic growth.
c) Helicobacter pylori – Diagnosed via urease test, not string test.
d) Aeromonas hydrophila – Rarely weak string-positive, but not diagnostic (more reliably identified by oxidase+ and resistance to O/129).
38 / 118
Category:
ASCP Exam Questions
The oxidase test reagent contains which compound?
The oxidase test reagent contains tetramethyl-p-phenylenediamine dihydrochloride , which acts as an artificial electron acceptor for cytochrome c oxidase (a component of the bacterial electron transport chain).
Positive result : Dark blue/purple color change within seconds (e.g., Pseudomonas , Neisseria ).
Negative result : No color change (e.g., Enterobacteriaceae ).
Other options (incorrect):
(b) Phenol red → pH indicator (e.g., in carbohydrate fermentation tests).
(c) Crystal violet → Gram stain component or selective agent in MacConkey agar.
(d) Malachite green → Used in endospore staining.
39 / 118
Category:
ASCP Exam Questions
The satellite test is commonly used to identify which bacterium?
The satellite phenomenon (or satellite test ) is used to identify Haemophilus influenzae , which requires V factor (NAD or NADP) for growth.
When cultured near Staphylococcus aureus (which secretes V factor), H. influenzae forms small colonies “satelliting” around the S. aureus streaks.
This occurs because H. influenzae cannot grow without V factor unless it is provided by nearby bacteria.
Why Not the Other Options? b) Neisseria gonorrhoeae → Identified by oxidase test and selective media (e.g., Thayer-Martin agar).
c) Escherichia coli → Grows independently and does not require V factor.
d) Streptococcus pyogenes → Identified by beta-hemolysis and bacitracin sensitivity.
40 / 118
Category:
ASCP Exam Questions
Anaerobic gram-positive bacilli with subterminal spores isolated from a peritoneal abscess are most likely:
Clostridium septicum is an anaerobic, Gram-positive bacillus that forms subterminal spores and is associated with:
Peritoneal abscesses (often secondary to bowel pathology, e.g., colon cancer).
Gas gangrene (myonecrosis) in traumatic or spontaneous infections.
Why Not Other Options? (a) Bacillus cereus : Aerobic , spore-forming, foodborne pathogen (not anaerobic).
(c) Eggerthella lenta : Anaerobic Gram-positive non-spore-forming rod (part of gut flora).
(d) Bifidobacterium dentium : Anaerobic Gram-positive branching rod (commensal, no spores).
41 / 118
Category:
ASCP Exam Questions
Which test detects bacterial ability to convert tryptophan into indole using Kovac’s reagent?
The Indole test determines if a bacterium can break down the amino acid tryptophan into indole using the enzyme tryptophanase .
Kovac’s reagent (containing *p*-dimethylaminobenzaldehyde) is added to the culture.
Key Uses: Why Not the Other Options? a) Methyl Red (MR) test : Detects mixed-acid fermentation (e.g., E. coli vs. Enterobacter ).
c) Urease test : Identifies bacteria that hydrolyze urea (e.g., Proteus , Helicobacter pylori ).
d) Citrate test : Tests for citrate utilization (e.g., Klebsiella + vs. E. coli –).
42 / 118
Category:
ASCP Exam Questions
A common cause of acute exudative pharyngitis is:
Streptococcus pyogenes (Group A Streptococcus, GAS) is the most common bacterial cause of acute exudative pharyngitis (strep throat).
Clinical features : Sudden-onset sore throat, fever, tonsillar exudate, and tender cervical lymphadenopathy.
Diagnosis : Rapid antigen detection test (RADT) or throat culture.
Why Not the Others?
(a) Staphylococcus aureus : Causes skin infections (e.g., abscesses) or toxic shock syndrome, not classic pharyngitis.
(b) Streptococcus pneumoniae : A pathogen of pneumonia/meningitis/otitis media, not pharyngitis.
(c) Streptococcus agalactiae (Group B Streptococcus) : Neonatal sepsis/meningitis; no role in pharyngitis.
43 / 118
Category:
ASCP Exam Questions
Which enzyme is detected using the beta-lactamase test?
The beta-lactamase test detects the enzyme penicillinase (a type of beta-lactamase), which breaks down the beta-lactam ring in penicillin antibiotics , conferring resistance.
Positive result : Rapid degradation of penicillin (e.g., color change in nitrocefin test).
Clinically relevant for Staphylococcus aureus , Haemophilus influenzae , and Neisseria gonorrhoeae .
Why Not Other Options? (a) Urease : Hydrolyzes urea (e.g., Proteus , H. pylori ).
(c) Oxidase : Detects cytochrome c oxidase (Pseudomonas , Neisseria ).
(d) Coagulase : Clots plasma (S. aureus vs. S. epidermidis ).
44 / 118
Category:
ASCP Exam Questions
What color change indicates a positive citrate test on Simmons citrate agar?
Simmons citrate agar contains bromothymol blue , a pH indicator that is green at neutral pH and turns blue in alkaline conditions .
Bacteria that utilize citrate (e.g., Klebsiella , Enterobacter ) metabolize it into carbonates and bicarbonates , raising the pH.
A positive result shows blue coloration (alkaline pH), while a negative result remains green.
Why Not the Other Options? a) Red to yellow → Seen in urea hydrolysis (e.g., Proteus ).
c) Yellow to pink → Occurs in MacConkey agar (lactose fermentation).
d) Colorless to black → Indicates H₂S production (e.g., Salmonella in TSI agar).
45 / 118
Category:
ASCP Exam Questions
A triple sugar iron (TSI) agar slant showing a yellow butt and red slant indicates:
In Triple Sugar Iron (TSI) agar :
Other TSI Interpretations :
(b) Lactose/sucrose fermentation : Yellow butt + yellow slant (both sugars fermented).
(c) No fermentation : Red butt + red slant (inert organism, e.g., Pseudomonas ).
Gas/H₂S production : Cracks (gas) or black precipitate (H₂S) may accompany results.
46 / 118
Category:
ASCP Exam Questions
Which biochemical test detects bacterial ability to ferment lactose with gas production?
The phenol red lactose broth test detects:
Lactose fermentation : Acid production turns the medium yellow (phenol red indicator).
Gas production : Visible as bubbles in the Durham tube.
Why Not Other Options? (a) SIM test : Detects sulfide production (black precipitate), indole (red ring with Kovac’s), and motility (cloudy spread).
(c) Citrate test : Identifies citrate utilization (blue color change, e.g., Klebsiella ).
(d) Urease test : Detects urea hydrolysis (pink color, e.g., Proteus ).
47 / 118
Category:
ASCP Exam Questions
A positive indole test produces which visible change?
The indole test detects the ability of bacteria (e.g., E. coli ) to produce indole from the amino acid tryptophan using the enzyme tryptophanase .
Kovac’s reagent (containing p-dimethylaminobenzaldehyde ) is added to the culture.
A positive result forms a red/pink ring at the top of the medium due to the reaction between indole and Kovac’s reagent.
Why Not the Other Options? b) Blue-green color → Seen in oxidase test (e.g., Pseudomonas ).
c) Black precipitate → Occurs in H₂S production tests (e.g., SIM agar).
d) Gas bubble release → Indicates fermentation (e.g., in Durham tube tests).
48 / 118
Category:
ASCP Exam Questions
The most frequent cause of prosthetic heart valve infections occurring within 2-3 months after surgery is:
Prosthetic valve endocarditis (PVE) occurring within 2–3 months post-surgery is most commonly caused by coagulase-negative staphylococci (CoNS) , particularly Staphylococcus epidermidis . These organisms:
Why Not Other Options? (a) Streptococcus pneumoniae : Rarely causes PVE; more associated with native valve endocarditis.
(b) Streptococcus pyogenes : Causes acute rheumatic fever or pharyngitis, not early PVE.
(c) Staphylococcus aureus : More common in late PVE (>12 months) or IV drug use-related endocarditis .
49 / 118
Category:
ASCP Exam Questions
The hippurate hydrolysis test is used primarily to identify:
The hippurate hydrolysis test identifies Group B Streptococcus (GBS) by detecting the enzyme hippuricase , which breaks down sodium hippurate into glycine and benzoic acid .
Positive result : Formation of glycine is detected with ninhydrin reagent, turning deep purple (indicating S. agalactiae ).
Negative result : No color change (other streptococci).
Why Not Other Options? (a) S. pyogenes (Group A): Identified by bacitracin sensitivity or PYR test .
(c) S. pneumoniae : Identified by optochin sensitivity and bile solubility .
(d) E. faecalis : Identified by PYR test and growth in 6.5% NaCl .
50 / 118
Category:
ASCP Exam Questions
The nitrate reduction test is used to detect:
The nitrate reduction test is used to determine if bacteria can reduce nitrate (NO₃⁻) to nitrite (NO₂⁻) or further to nitrogen gas (N₂) or other nitrogenous compounds. This test helps differentiate bacteria based on their nitrate reductase enzyme activity.
The other options are unrelated:
a) Acid production from lactose is detected by tests like the MacConkey agar or phenol red broth .
c) Hydrogen sulfide (H₂S) formation is detected using SIM agar or TSI agar .
d) Beta-lactamase activity is tested using assays like the nitrocefin test or penicillin disk methods .
51 / 118
Category:
ASCP Exam Questions
Which test differentiates Staphylococcus saprophyticus from Staphylococcus epidermidis?
Staphylococcus saprophyticus is resistant to novobiocin , while Staphylococcus epidermidis is susceptible .
The test involves placing a novobiocin disk on a culture plate:
Why Not the Other Tests? a) Coagulase test : Both S. saprophyticus and S. epidermidis are coagulase-negative (this test only identifies S. aureus ).
c) Catalase test : Both are catalase-positive (does not differentiate them).
d) DNase test : Not routinely used for this purpose (though S. saprophyticus is usually DNase-negative, while S. epidermidis may be variable).
52 / 118
Category:
ASCP Exam Questions
Which test is used to differentiate between Micrococcus and Staphylococcus species?
The coagulase test (a) is the most commonly used test to differentiate Staphylococcus aureus (coagulase-positive) from other Staphylococcus species and Micrococcus (both coagulase-negative).
Why not the others? Oxidase test (b): Micrococcus is oxidase-positive, but Staphylococcus is usually negative (though some strains may vary).
Bacitracin test (c): Micrococcus is often susceptible, while Staphylococcus is resistant, but this is less reliable.
Catalase test (d): Both are catalase-positive, so it doesn’t differentiate.
53 / 118
Category:
ASCP Exam Questions
Which test detects the ability of bacteria to produce β-galactosidase enzyme?
The ONPG (o-nitrophenyl-β-D-galactopyranoside) test detects the enzyme β-galactosidase , which hydrolyzes ONPG into o-nitrophenol (yellow) and galactose.
A yellow color indicates a positive result , confirming β-galactosidase activity.
Key Uses: ✔ Differentiates late lactose fermenters (e.g., Citrobacter , Shigella sonnei ) from non-lactose fermenters (e.g., Salmonella ).E. coli (β-galactosidase-positive) vs. Shigella (usually negative).
Why Not the Other Tests? b) Indole test → Detects tryptophanase (e.g., E. coli ).
c) Urease test → Identifies urease enzyme (e.g., Proteus ).
d) Catalase test → Checks for catalase (e.g., Staphylococcus vs. Streptococcus ).
54 / 118
Category:
ASCP Exam Questions
Which enzyme is detected by the β-lactamase test to determine penicillin resistance?
The β-lactamase test detects the enzyme beta-lactamase , which hydrolyzes the β-lactam ring in penicillin and related antibiotics (e.g., ampicillin, amoxicillin), conferring resistance.
A positive result (e.g., color change in nitrocefin-based tests) indicates the bacterium can inactivate penicillin .
Key Uses: ✔ Rapidly identifies penicillin-resistant strains (e.g., Staphylococcus aureus , Haemophilus influenzae , Neisseria gonorrhoeae ).
Why Not the Other Options? a) Cytochrome oxidase → Detected by the oxidase test (e.g., Pseudomonas ).
c) Nitrate reductase → Involved in nitrate reduction tests (e.g., E. coli ).
d) DNA polymerase → Irrelevant to antibiotic resistance testing.
55 / 118
Category:
ASCP Exam Questions
The urease breath test diagnoses infection with:
Purpose : The urease breath test (UBT) is a non-invasive diagnostic tool specifically designed to detect active Helicobacter pylori infections, a bacterium linked to gastritis, peptic ulcers, and gastric cancer .
Mechanism :
H. pylori produces urease , an enzyme that breaks down urea into ammonia and carbon dioxide (CO₂).
During the test, the patient ingests urea labeled with a carbon isotope (¹³C or ¹⁴C). If H. pylori is present, urease converts the labeled urea into labeled CO₂, which is exhaled and measured .
Clinical Utility :
Used for initial diagnosis and post-treatment verification of eradication .
Preferred over serology (which cannot distinguish active vs. past infections) and stool antigen tests (less convenient for some patients) .
Why Not the Others? a) Salmonella typhi : Diagnosed via blood/stool culture or Widal test, not urease breath testing.
c) Shigella dysenteriae : Detected through stool culture or PCR; no urease-based breath test exists.
d) Clostridioides difficile : Diagnosed via stool toxin assays or PCR; unrelated to urease activity.
56 / 118
Category:
ASCP Exam Questions
A CSF Gram stain shows gram-negative diplococci. The most likely pathogen is:
Gram-negative diplococci – This morphology is classic for Neisseria meningitidis (and N. gonorrhoeae , but the latter rarely causes meningitis).
Rules out:
Streptococcus pneumoniae (a): Gram-positive lancet-shaped diplococci .
Haemophilus influenzae (b): Gram-negative coccobacilli (not diplococci).
Listeria monocytogenes (d): Gram-positive rods .
Clinical Context (CSF) :
N. meningitidis is a leading cause of bacterial meningitis , especially in young adults and outbreaks.
H. influenzae (b) is now rare due to vaccination (Hib vaccine).
Confirmatory Tests: 57 / 118
Category:
ASCP Exam Questions
The D-test detects inducible resistance to:
Purpose :
The D-test detects inducible macrolide-lincosamide-streptogramin B (iMLSB) resistance in Staphylococcus aureus and other Gram-positive bacteria.
Specifically, it identifies strains that appear susceptible to clindamycin but harbor erm genes that can induce resistance during treatment.
Mechanism :
Clinical Impact :
If the D-test is positive , clindamycin should not be used (risk of treatment failure).
If negative , clindamycin remains a treatment option.
Why Not the Others? a) Vancomycin : Resistance is detected via vanA/vanB genes or MIC testing (e.g., VRE).
c) Penicillin : Resistance in S. aureus is detected via beta-lactamase or mecA gene (for MRSA).
d) Ciprofloxacin : Resistance is chromosomal or plasmid-mediated (no D-test equivalent).
58 / 118
Category:
ASCP Exam Questions
A urine culture grows >100,000 CFU/mL of a gram-negative bacillus that is indole-positive and motile. The organism is likely:
Gram-negative bacillus – All options (a-d) fit, so further differentiation is needed.
Indole-positive – Strongly suggests E. coli (b), as most strains are indole-positive.
Klebsiella pneumoniae (a) is indole-negative .
Proteus mirabilis (c) is indole-negative (P. vulgaris is indole-positive, but less common in UTIs).
Serratia marcescens (d) is typically indole-negative .
Motile – E. coli is motile, further supporting the answer.
Why Not the Others? a) Klebsiella pneumoniae – Indole-negative, non-motile.
c) Proteus mirabilis – Indole-negative (though motile and common in UTIs).
d) Serratia marcescens – Usually indole-negative and less common in uncomplicated UTIs.
59 / 118
Category:
ASCP Exam Questions
The Gram stain differentiates bacteria based on:
Gram staining classifies bacteria based on fundamental differences in their cell wall structure , which directly affects their staining properties :
Gram-positive bacteria :
Thick peptidoglycan layer (60–90% of cell wall).
Retains crystal violet dye (purple color) after alcohol decolorization.
Examples : Staphylococcus , Streptococcus .
Gram-negative bacteria :
Thin peptidoglycan layer (10–20%) + outer lipid membrane .
Loses crystal violet during decolorization and takes up safranin counterstain (pink/red).
Examples : E. coli , Pseudomonas .
Why Not the Others? a) Enzyme activity : Requires biochemical tests (e.g., catalase/oxidase).
c) Oxygen requirement : Determined by culture conditions (aerobic/anaerobic), not staining.
d) Growth rate : Observed on culture media, unrelated to Gram classification.
60 / 118
Category:
ASCP Exam Questions
What is the main purpose of performing a Gram stain before further testing?
The main purpose of a Gram stain is to differentiate bacteria based on their cell wall composition :
Gram-positive bacteria have a thick peptidoglycan layer (retains crystal violet, appearing purple).
Gram-negative bacteria have a thin peptidoglycan layer and an outer lipid membrane (loses crystal violet, counterstains pink/red).
This classification is critical because:
Guides the choice of culture media (e.g., MacConkey for Gram-negatives).
Informs initial antibiotic selection (e.g., penicillin targets Gram-positive peptidoglycan).
Directs further biochemical testing .
Why Not the Others? a) Spore formation → Detected with specialized stains (e.g., malachite green for endospores).
c) Motility → Assessed via wet mount microscopy or motility agar.
d) Oxygen requirements → Determined by culturing in aerobic/anaerobic conditions, not Gram staining .
61 / 118
Category:
ASCP Exam Questions
The phenol red lactose broth test is designed to detect:
The phenol red lactose broth test is a carbohydrate fermentation test used to determine if bacteria can ferment lactose , producing:
Acid (lowers pH → yellow color change).
Gas (trapped in a Durham tube).
How It Works: Clinical Utility: Why Not the Others? a) Spore formation : Detected with malachite green stain (e.g., for Bacillus ).
c) Urease activity : Tested with urea broth (pink = positive).
d) Gelatin liquefaction : Requires gelatin agar stab (liquefaction at 4°C).
62 / 118
Category:
ASCP Exam Questions
Which rapid identification test is commonly used for Neisseria gonorrhoeae confirmation?
The carbohydrate utilization test (e.g., Cystine Trypticase Agar (CTA) sugars ) is a standard rapid method to confirm Neisseria gonorrhoeae by assessing its ability to ferment specific carbohydrates:
N. gonorrhoeae : Ferments glucose (acid production) but not maltose, lactose, or sucrose .
N. meningitidis : Ferments glucose and maltose .
Why Not Other Tests? (a) Oxidase test : Neisseria species are oxidase-positive, but this only confirms the genus, not the species.
(c) Latex agglutination : Used for Cryptococcus or Strep pneumoniae (not standard for N. gonorrhoeae ).
(d) Urease test : Used for Proteus or H. pylori (irrelevant here).
63 / 118
Category:
ASCP Exam Questions
A positive Voges-Proskauer (VP) test indicates:
The Voges-Proskauer (VP) test detects bacteria that ferment glucose via the butanediol pathway , producing acetoin (a precursor to 2,3-butanediol).
How It Works: Bacteria are cultured in glucose-phosphate broth .
Barritt’s reagents (α-naphthol + KOH) are added.
Positive result : A red/pink color (acetoin reacts with reagents).
Negative result : No color change (yellow/brown).
Why Not the Others? a) Mixed acid fermentation : Detected by the methyl red (MR) test (red = positive).
c) Indole production : Tested via Kovac’s reagent (red ring = positive).
d) Gas production : Observed in Durham tubes (e.g., lactose broth).
64 / 118
Category:
ASCP Exam Questions
A sputum culture from an alcoholic grows mucoid, dark pink colonies on MacConkey agar. The organism is:
Mucoid, dark pink (lactose-fermenting) colonies on MacConkey agar in an alcoholic patient strongly suggest Klebsiella pneumoniae .
Why Not the Others?
(a) Edwardsiella tarda : Typically non-lactose fermenting (colorless colonies on MacConkey).
(c) Escherichia coli : Ferments lactose but forms pink, non-mucoid colonies (less viscous).
(d) Proteus vulgaris : Non-lactose fermenting and swarms on agar (no pink color).
65 / 118
Category:
ASCP Exam Questions
The organism most commonly associated with neonatal purulent meningitis is:
Group B streptococci (GBS) are the most common cause of neonatal purulent meningitis , particularly in:
Why Not Other Options? (a) Neisseria meningitidis : More common in older children/adults (rare in neonates).
(b) Streptococcus pneumoniae : Causes meningitis in all ages but is less frequent in neonates.
(d) Haemophilus influenzae : Now rare due to Hib vaccination (historically affected infants >1 month).
66 / 118
Category:
ASCP Exam Questions
A blood culture bottle shows gram-positive cocci in clusters. Colonies are catalase-positive and coagulase-positive. The organism is:
Gram-positive cocci in clusters – Suggests Staphylococcus (streptococci and enterococci form chains or pairs).
Catalase-positive – Rules out Streptococcus (b) and Enterococcus (d), which are catalase-negative.
Coagulase-positive – Confirms Staphylococcus aureus (c), as it is the primary coagulase-positive Staphylococcus .
Why Not the Others? a) Staphylococcus epidermidis – Coagulase-negative (part of normal skin flora, often a contaminant).
b) Streptococcus agalactiae – Catalase-negative, gram-positive cocci in chains.
d) Enterococcus faecalis – Catalase-negative, gram-positive cocci in pairs/short chains.
67 / 118
Category:
ASCP Exam Questions
A wound culture grows gram-negative bacilli producing a blue-green pigment. The organism is:
Sorbitol-MacConkey agar (SMAC) is the standard medium to screen for E. coli O157:H7 because:
Why Not the Others?
(a) Indole : A biochemical test (post-culture), not a component of MacConkey agar.
(b) Citrate : Used in Simmons citrate agar (irrelevant here).
(d) Lactose : Standard MacConkey contains lactose, but E. coli O157:H7 ferments lactose (pink colonies), making it indistinguishable from normal flora without sorbitol differentiation .
68 / 118
Category:
ASCP Exam Questions
Which test confirms bacterial motility?
The SIM agar test (Sulfide-Indole-Motility) is a multitest medium that detects:
Motility : Cloudy growth radiating from the stab line (motile bacteria, e.g., Proteus ).
Indole production : Red ring with Kovac’s reagent (e.g., E. coli ).
H₂S production : Black precipitate (e.g., Salmonella ).
Why Not Other Options? (b) Citrate test : Identifies citrate utilization (e.g., Klebsiella ).
(c) Voges-Proskauer test : Detects acetoin (e.g., Enterobacter ).
(d) Oxidase test : Identifies cytochrome c oxidase (e.g., Pseudomonas ).
70 / 118
Category:
ASCP Exam Questions
A blood culture grows gram-negative rods that require X and V factors. The organism is:
Haemophilus influenzae is a fastidious gram-negative rod that requires both X (hemin) and V (NAD) factors for growth, typically cultured on chocolate agar (heated blood agar) or supplemented media like Haemophilus Test Medium (HTM) .
This distinguishes it from other gram-negative rods:
Brucella melitensis (b) : Requires CO₂ but not X/V factors; grows on standard blood agar .
Bordetella pertussis (c) : Needs charcoal-blood agar (Regan-Lowe or Bordet-Gengou media) but not X/V .
Legionella pneumophila (d) : Grows on buffered charcoal yeast extract (BCYE) agar , no X/V requirement .
73 / 118
Category:
ASCP Exam Questions
Which initial test is typically performed to classify bacteria in a clinical laboratory?
Gram staining is universally performed first in bacterial classification because it:
Divides bacteria into two fundamental groups :
Gram-positive (thick peptidoglycan, retains crystal violet → purple)
Gram-negative (thin peptidoglycan + outer membrane → pink/red)
Guides all subsequent testing :
Determines choice of culture media (e.g., blood agar vs. MacConkey).
Informs antibiotic selection (e.g., vancomycin targets Gram-positives).
Directs further biochemical tests (e.g., coagulase for Gram-positive cocci; TSI for Gram-negative rods).
Why Not the Others? a) Oxidase test : Used after Gram staining to differentiate Gram-negatives (e.g., Pseudomonas vs. Enterobacteriaceae ).
c) Catalase test : Follows Gram stain to separate Staphylococcus (catalase-positive) from Streptococcus (catalase-negative).
d) Coagulase test : Specific for Gram-positive cocci (e.g., S. aureus identification).
74 / 118
Category:
ASCP Exam Questions
What is the purpose of using mannitol salt agar?
Purpose of Mannitol Salt Agar (MSA): Selective medium : Contains 7.5–10% NaCl , which inhibits most bacteria except Staphylococcus species (salt-tolerant).
Differential medium : Contains mannitol and a pH indicator (phenol red) .
Staphylococcus aureus ferments mannitol → produces acid → turns the medium yellow .
Other Staphylococcus species (e.g., S. epidermidis ) do not ferment mannitol → medium remains pink/red .
Why Not the Other Options? a) Lactose fermenters → MacConkey agar or EMB agar are used instead.
c) Hemolysis detection → Blood agar (e.g., sheep or horse blood) is used.
d) Motility determination → Motility test medium or SIM agar is used.
75 / 118
Category:
ASCP Exam Questions
The indole test is performed to detect bacterial ability to:
The indole test identifies bacteria that produce the enzyme tryptophanase , which hydrolyzes the amino acid tryptophan into:
How It Works: Bacteria are cultured in tryptone broth (rich in tryptophan).
Kovac’s reagent (contains *p*-dimethylaminobenzaldehyde) is added.
Positive result : A red/pink layer forms (indole reacts with the reagent).
Negative result : No color change (yellow reagent remains).
Clinical Utility: Why Not the Others? a) Nitrate reduction : Detected via nitrate reductase test (red color with zinc).
b) Urea hydrolysis : Tested with urease test (pink color from ammonia).
d) Citrate utilization : Assessed with Simmons’ citrate agar (blue color change).
76 / 118
Category:
ASCP Exam Questions
Which carbohydrate fermentation test is essential for differentiating Neisseria species?
Why Not the Other Options? b) Lactose fermentation only → Too limited; lactose helps distinguish N. lactamica but not other Neisseria .
c) Citrate utilization → Used for Enterobacteriaceae , not Neisseria .
d) Voges-Proskauer test → Detects acetoin production (e.g., Enterobacter ), irrelevant here.
77 / 118
Category:
ASCP Exam Questions
Which test differentiates between Pseudomonas and Enterobacteriaceae?
The oxidase test is the most reliable method to differentiate Pseudomonas (oxidase-positive) from Enterobacteriaceae (oxidase-negative) .
Pseudomonas spp. (e.g., P. aeruginosa ):
Oxidase-positive → Turns dark blue/purple (due to cytochrome c oxidase).
Aerobic, opportunistic pathogens (e.g., wound/respiratory infections).
Enterobacteriaceae (e.g., E. coli, Salmonella, Klebsiella ):
Oxidase-negative → No color change.
Facultative anaerobes, common in gut flora and infections (UTIs, sepsis).
Why Not the Others? a) Catalase test : Both groups are catalase-positive (useless for differentiation).
c) TSI agar test : Used to differentiate within Enterobacteriaceae (e.g., Salmonella vs. E. coli ), but Pseudomonas does not ferment sugars in TSI.
d) Coagulase test : Only relevant for Staphylococcus (e.g., S. aureus is coagulase-positive).
78 / 118
Category:
ASCP Exam Questions
A positive PYR test identifies:
Purpose : The PYR (L-pyrrolidonyl-β-naphthylamide) test is a rapid biochemical test used to identify:
Mechanism :
The test detects the enzyme pyrrolidonyl arylamidase (PYRase)
S. pyogenes produces this enzyme, which hydrolyzes the PYR substrate
A color change to bright pink/red indicates a positive result
Clinical Utility :
Why Not the Others? b) Staphylococcus aureus : PYR-negative (identified by coagulase test)
c) Proteus vulgaris : PYR-negative (identified by urease and phenylalanine deaminase tests)
d) Klebsiella pneumoniae : PYR-negative (identified by lactose fermentation and capsule production)
79 / 118
Category:
ASCP Exam Questions
Which test detects extended-spectrum beta-lactamases (ESBLs)?
ESBL Definition :
Extended-spectrum beta-lactamases (ESBLs) hydrolyze penicillins, cephalosporins (e.g., ceftazidime, cefotaxime), and aztreonam , but are inhibited by clavulanic acid .
Synergy Test (c) :
The ceftazidime/clavulanic acid combination disk test is the gold standard for ESBL detection.
Positive result : Increased zone of inhibition around ceftazidime+clavulanate vs. ceftazidime alone (≥5 mm difference).
Alternative: Cefotaxime/clavulanic acid can also be used.
Why Not the Others? a) Oxidase test : Identifies Pseudomonas or Neisseria (not related to resistance).
b) Cefoxitin disk test : Detects methicillin-resistant Staphylococcus aureus (MRSA) or inducible AmpC beta-lactamases (not ESBLs).
d) Bacitracin susceptibility : Screens for Streptococcus pyogenes (Group A Strep), not resistance mechanisms.
80 / 118
Category:
ASCP Exam Questions
What is the main purpose of performing antimicrobial susceptibility testing?
The primary purpose of AST is to guide antibiotic selection by identifying which antimicrobial agents are effective against a specific bacterial isolate.
Common methods include disk diffusion (Kirby-Bauer) , E-test , and broth microdilution (MIC determination) .
Key Objectives: ✔ Avoid ineffective antibiotics , reducing treatment failure.Prevent antibiotic resistance by promoting targeted therapy.Confirm empirical treatment (e.g., adjusting therapy based on lab results).
Why Not the Other Options? a) Bacterial morphology → Determined by microscopy (e.g., Gram stain).
c) Spore formation → Observed via specialized stains (e.g., malachite green).
d) Gram reaction → Identified through Gram staining, not AST.
81 / 118
Category:
ASCP Exam Questions
A sputum Gram stain shows numerous neutrophils and small gram-negative coccobacilli. The organism grows only on chocolate agar. This suggests:
Gram-negative coccobacilli – Rules out:
Streptococcus pneumoniae (Gram-positive cocci, option a )
Mycobacterium tuberculosis (acid-fast, not seen on Gram stain, option d )
Pseudomonas aeruginosa (Gram-negative rods , not coccobacilli, option c )
Grows only on chocolate agar – Haemophilus influenzae requires X (hemin) and V (NAD) factors , which are provided by chocolate agar (heated blood agar). It does not grow on standard blood agar.
Clinical context (sputum with neutrophils) – Consistent with H. influenzae respiratory infections (e.g., pneumonia, exacerbations of COPD).
Why Not the Others? a) S. pneumoniae – Gram-positive, grows on blood agar (shows alpha-hemolysis).
c) P. aeruginosa – Gram-negative rod , grows on standard media (e.g., MacConkey agar).
d) M. tuberculosis – Requires Lowenstein-Jensen medium or specialized mycobacterial culture, not chocolate agar.
82 / 118
Category:
ASCP Exam Questions
Which rapid test is commonly used to identify Staphylococcus aureus in clinical samples?
The slide coagulase test is a rapid method to identify Staphylococcus aureus by detecting clumping factor (a cell wall-bound protein that binds fibrinogen and causes plasma agglutination).
Positive result : Immediate clumping of bacterial cells when mixed with rabbit plasma.
Negative result : No clumping (e.g., S. epidermidis or S. saprophyticus ).
Why Not Other Options? (b) Catalase test : All Staphylococcus species are catalase-positive (only rules out Streptococcus ).
(c) Indole test : Used for Gram-negatives (e.g., E. coli vs. Klebsiella ).
(d) TSI agar : Used for Enterobacteriaceae (e.g., Salmonella , Shigella ).
83 / 118
Category:
ASCP Exam Questions
A black precipitate forming on a TSI agar slant indicates:
In Triple Sugar Iron (TSI) agar , a black precipitate forms when bacteria produce hydrogen sulfide (H₂S) . This occurs due to:
Reduction of thiosulfate (in the medium) → H₂S gas.
Reaction with ferrous sulfate (indicator) → ferrous sulfide (FeS) , a black precipitate.
Key Bacteria That Produce H₂S: Salmonella spp. (e.g., S. Typhi → prominent blackening).
Proteus spp. (e.g., P. mirabilis ).
Some Citrobacter and Edwardsiella strains.
Clinical Relevance: Helps differentiate enteric pathogens (e.g., Salmonella vs. Shigella , which is H₂S-negative).
Supports diagnosis of gastrointestinal infections (e.g., typhoid fever).
Why Not the Others? a) Nitrate reduction : Detected via nitrate broth (red color with zinc).
c) Indole : Tested with Kovac’s reagent (red ring = positive).
d) Urease activity : Turns urea broth pink (e.g., Proteus , H. pylori ).
84 / 118
Category:
ASCP Exam Questions
Which test presumptively identifies Streptococcus pneumoniae?
Bile solubility test is a key presumptive test for Streptococcus pneumoniae .
Optochin sensitivity (P disk test) is another confirmatory test for S. pneumoniae , but bile solubility is also highly specific .
Why Not the Others? b) Catalase production – S. pneumoniae is catalase-negative , but this is a general test to differentiate staphylococci (catalase+) from streptococci (catalase-).
c) Coagulase test – Used to identify Staphylococcus aureus (coagulase+), not pneumococci.
d) Urease activity – Used for organisms like Proteus or Helicobacter pylori , not S. pneumoniae .
85 / 118
Category:
ASCP Exam Questions
Which organism produces a blue-green pigment and grape-like odor?
Blue-green pigment :
Produces pyocyanin (blue) and pyoverdine (green), which combine to create its distinctive blue-green color in cultures and infected tissues .
This pigment is visible on agar plates and in clinical specimens (e.g., wound exudates or sputum) .
Grape-like odor :
The organism emits a sweet, fruity odor due to the production of 2-aminoacetophenone , often described as resembling grapes or corn tortillas .
This odor is a diagnostic clue in clinical settings (e.g., infected burns or respiratory secretions) .
Why Not the Others? a) Serratia marcescens : Produces a red pigment (prodigiosin) and lacks the grape-like odor .
c) Enterobacter cloacae : Non-pigmented or pale yellow; no distinctive odor .
d) Acinetobacter baumannii : Non-pigmented and odorless; known for antibiotic resistance, not pigment production .
86 / 118
Category:
ASCP Exam Questions
The oxidase reagent must be read within a short time because:
The oxidase reagent (e.g., tetramethyl-p-phenylenediamine) is a redox indicator that turns purple/blue when oxidized by cytochrome c oxidase in bacteria.
However, the reagent is light-sensitive and unstable —it auto-oxidizes upon prolonged exposure to air, leading to a color change even without bacterial enzymes , which can cause false-positive results .
Therefore, results must be read within 10–30 seconds for accuracy.
Why Not the Other Options? a) While some reagents can be toxic, this isn’t the primary reason for rapid reading.
b) Evaporation isn’t a significant issue with oxidase reagents.
d) The oxidase test detects cytochrome c oxidase , not catalase (catalase activity is tested separately with hydrogen peroxide).
87 / 118
Category:
ASCP Exam Questions
Which of the following is the first step in identifying an unknown bacterial isolate in the clinical laboratory?
The first step in identifying an unknown bacterial isolate is Gram staining , which categorizes bacteria into:
Gram-positive (purple)
Gram-negative (pink/red)
This basic classification guides further testing (e.g., culture media selection, biochemical tests). While other steps (b, c, d) are important, they come after initial Gram staining.
Why not the others?
b) Culture on selective media : Requires prior knowledge (e.g., Gram type) to choose the right media.
c) Biochemical testing : Performed after preliminary identification (e.g., Gram reaction).
d) Antibiotic susceptibility testing : Done after identifying the bacterium.
88 / 118
Category:
ASCP Exam Questions
A positive DNase test indicates that the organism:
A positive DNase test indicates the organism produces deoxyribonuclease (DNase) , an enzyme that hydrolyzes DNA into smaller fragments.
Why Not Other Options? (b) Nitrate utilization : Detected by nitrate reduction test .
(c) H₂S production : Seen in SIM or TSI agar (e.g., Salmonella , Proteus ).
(d) Urea breakdown : Detected by urease test (e.g., Proteus , H. pylori ).
89 / 118
Category:
ASCP Exam Questions
The catalase test differentiates between:
The catalase test detects the enzyme catalase , which breaks down hydrogen peroxide (H₂O₂) into water and oxygen. This test is primarily used to differentiate:
Why Not Other Options? (a) Gram-positive cocci vs. Gram-negative rods : Catalase status varies within these groups (e.g., Enterococcus is Gram-positive/catalase-negative).
(c) Lactose fermenters : Differentiated by MacConkey agar or phenol red broths.
(d) Motility : Detected via motility agar or microscopic examination.
90 / 118
Category:
ASCP Exam Questions
A positive bile esculin test shows which result?
A positive bile esculin test results in blackening of the medium due to:
This indicates that the organism can grow in bile and hydrolyze esculin, typical of Group D streptococci (including Enterococcus ) and some other bacteria.
Other options:
(a) Pink color → PYR test (for Enterococcus ).
(c) Gas in Durham tube → Fermentation tests (e.g., lactose fermentation).
(d) Blue-green → Pseudomonas pigments (irrelevant here).
91 / 118
Category:
ASCP Exam Questions
Which biochemical test is key to differentiating many Enterobacteriaceae species?
The TSI test is a fundamental biochemical assay for differentiating Enterobacteriaceae (a large family of Gram-negative rods including E. coli , Salmonella , Shigella , and Proteus ). It evaluates three key metabolic traits simultaneously:
Sugar fermentation (glucose, lactose, sucrose) → Acid production (yellow).
Gas production → Cracks or lifting of the agar.
Hydrogen sulfide (H₂S) production → Black precipitate (e.g., Salmonella , Proteus ).
Why Not the Others? a) Oxidase test : Enterobacteriaceae are uniformly oxidase-negative ; this test helps distinguish them from other Gram-negative bacteria (e.g., Pseudomonas ).
c) Catalase test : Most Enterobacteriaceae are catalase-positive; this test is more useful for separating Staphylococcus (catalase-positive) from Streptococcus (catalase-negative).
d) Bile solubility test : Used to differentiate Streptococcus pneumoniae (soluble in bile) from other alpha-hemolytic streptococci.
Key Clinical Utility: The TSI test is low-cost, rapid, and highly informative for:
Identifying enteric pathogens (e.g., Salmonella in stool cultures).
Distinguishing lactose fermenters (e.g., E. coli , Klebsiella ) from non-fermenters (e.g., Shigella , Salmonella ).
93 / 118
Category:
ASCP Exam Questions
The optochin sensitivity test is primarily used to identify:
The optochin sensitivity test uses an ethylhydrocupreine (P disk) to differentiate:
Why Not Other Options? (a) Group A Streptococcus (S. pyogenes ) : Identified by bacitracin sensitivity or PYR test .
(b) Group B Streptococcus (S. agalactiae ) : Identified by CAMP test or hippurate hydrolysis .
(d) Enterococcus species : Identified by PYR test and growth in 6.5% NaCl .
94 / 118
Category:
ASCP Exam Questions
For Neisseria gonorrhoeae, the optimal growth atmosphere is:
Capnophilic Requirement :
Obligate Aerobe :
Not Microaerophilic (d) :
Additional Growth Requirements: Why Not the Others? a) Strict anaerobic – N. gonorrhoeae is an obligate aerobe.
b) Ambient air – Lacks the required CO₂ concentration.
d) Microaerophilic – Used for Campylobacter or Helicobacter , not Neisseria .
95 / 118
Category:
ASCP Exam Questions
A wound culture grows swarming gram-negative bacilli. This suggests:
Swarming motility – Proteus mirabilis is famous for its swarming growth pattern on agar plates, creating concentric waves of bacterial spread.
Gram-negative bacilli – All options (a-d) are Gram-negative rods, but only Proteus exhibits swarming.
Why Not the Others? a) Escherichia coli – Motile but does not swarm on agar.
c) Salmonella enterica – Motile but does not swarm like Proteus .
d) Klebsiella oxytoca – Non-motile (no flagella), so no swarming.
96 / 118
Category:
ASCP Exam Questions
The satellite phenomenon around Staphylococcus aureus colonies indicates the presence of:
Satellite growth refers to small colonies of Haemophilus influenzae growing around Staphylococcus aureus on blood agar.
This occurs because S. aureus releases NAD (V factor) and hemin (X factor) through hemolysis, which H. influenzae requires for growth.
H. influenzae cannot grow alone on standard blood agar but forms satellite colonies near S. aureus , which provides these essential nutrients.
Why Not the Others? a) Streptococcus pyogenes – Does not require X/V factors; grows independently on blood agar.
c) Neisseria meningitidis – Requires enriched media (e.g., chocolate agar) but does not show satellite phenomenon with S. aureus .
d) Pseudomonas aeruginosa – Grows readily on standard media without needing X/V factors.
97 / 118
Category:
ASCP Exam Questions
Which organism causes food poisoning by preformed enterotoxin?
Bacillus cereus causes food poisoning via preformed enterotoxins :
Emetic toxin (cereulide) : Heat-stable, preformed in contaminated food (e.g., fried rice), causing vomiting within 1–6 hours .
Diarrheal toxin : Heat-labile, produced in the intestine after ingestion of bacteria (watery diarrhea in 6–15 hours).
Why Not the Others?
(a) Salmonella enteritidis : Invades intestinal mucosa (toxins produced after ingestion, not preformed).
(b) Shigella sonnei : Produces Shiga toxin during infection (not preformed in food).
(d) Aeromonas hydrophila : Causes diarrhea via enterotoxins but not preformed in food.
98 / 118
Category:
ASCP Exam Questions
A positive string test is used to help identify:
The string test is a rapid screening method primarily used to identify Vibrio cholerae (a member of the Vibrio genus).
When a colony of V. cholerae is mixed with 0.5% sodium deoxycholate , it lyses and releases viscous DNA , forming a mucoid “string” when the loop is lifted.
This occurs due to the extracellular polysaccharides and DNA released from the lysed bacteria.
Why Not the Other Options? b) Escherichia coli → Does not produce a viscous string in this test.
c) Neisseria meningitidis → Identified by oxidase test and carbohydrate utilization, not the string test.
d) Bacillus anthracis → Identified by Gram stain, capsule staining, and lack of hemolysis.
99 / 118
Category:
ASCP Exam Questions
A positive methyl red test indicates:
The methyl red (MR) test detects mixed-acid fermentation , where bacteria produce stable acidic end products (e.g., lactic, acetic, and formic acids) from glucose.
Positive result : Red color (pH ≤4.4) after adding methyl red indicator (e.g., E. coli , Salmonella ).
Negative result : Yellow/orange (pH ≥6.0, indicating neutral products like acetoin, e.g., Enterobacter ).
Why Not Other Options? (a) Neutral end products : Indicates a negative MR test (part of Voges-Proskauer [VP] test).
(c) Acetoin production : Detected by the VP test (e.g., Klebsiella ).
(d) Citrate utilization : Tested separately (e.g., Klebsiella is citrate+ but MR-).
100 / 118
Category:
ASCP Exam Questions
The PYR test is most useful for identifying:
The PYR test detects the enzyme L-pyrrolidonyl arylamidase (PYRase) , which is produced by:
Enterococcus species (e.g., E. faecalis , E. faecium ).
Group A Streptococcus (Streptococcus pyogenes ).
Why Not Other Options? (b) S. pneumoniae : Identified by optochin sensitivity and bile solubility .
(c) S. aureus : Identified by coagulase test or DNase test .
(d) K. pneumoniae : Identified by urease test and capsule production .
101 / 118
Category:
ASCP Exam Questions
The best nonculture method for diagnosing Neisseria gonorrhoeae in females is:
NAAT is the gold standard for diagnosing Neisseria gonorrhoeae in females because:
High sensitivity (>95%) : Detects bacterial DNA/RNA even at low loads (asymptomatic/pauci-bacillary infections).
Non-invasive samples : Vaginal swabs, urine, or self-collected specimens are valid.
Co-testing for Chlamydia : Most NAATs simultaneously detect C. trachomatis .
Why Not the Others?
(a) Gram stain : Poor sensitivity in females (endocervical discharge lacks reliable intracellular diplococci).
(b) MALDI-TOF MS : Requires culture isolates (not a direct diagnostic tool).
(d) Serology : No role in acute diagnosis (antibodies may reflect past infection).
102 / 118
Category:
ASCP Exam Questions
Which organism requires cysteine for growth and causes tularemia?
Requires cysteine for growth – Francisella tularensis is a fastidious organism that needs cysteine-supplemented media (e.g., cysteine-enriched blood agar or Thayer-Martin agar with added cysteine ).
Causes tularemia – Also called “rabbit fever,” this zoonotic disease is transmitted via ticks, rabbits, or aerosol exposure.
Why Not the Others? a) Brucella abortus – Causes brucellosis; grows on standard enriched media (no cysteine requirement).
c) Yersinia pestis – Causes plague; grows on blood agar without cysteine.
d) Bartonella henselae – Causes cat-scratch disease; requires hemin but not cysteine.
103 / 118
Category:
ASCP Exam Questions
What result would indicate a positive urease test?
The urease test detects the enzyme urease , which hydrolyzes urea into ammonia (NH₃) and CO₂ . A positive result is indicated by:
Key Examples: Strongly positive : Helicobacter pylori (rapid pink in urea broth).
Weakly positive : Proteus spp. (slower reaction).
Negative : E. coli (no color change, remains yellow/orange).
Why Not the Others? a) Gas production : Seen in fermentation tests (e.g., lactose broth with Durham tube).
b) Blue-green color : Occurs in oxidase tests (tetramethyl-p-phenylenediamine reaction).
d) Black precipitate : Indicates H₂S production (e.g., in TSI or SIM agar).
104 / 118
Category:
ASCP Exam Questions
A positive oxidase test is typically observed in which bacterial group?
The oxidase test detects the presence of cytochrome c oxidase, an enzyme in the electron transport chain of certain bacteria.
Neisseria spp. (e.g., N. gonorrhoeae , N. meningitidis ) and Pseudomonas spp. (e.g., P. aeruginosa ) are oxidase-positive .
Many other aerobic and facultative anaerobic bacteria (like Vibrio , Campylobacter , and Aeromonas ) also test positive.
Why Not the Other Options? a) Enterobacteriaceae (e.g., E. coli , Salmonella , Klebsiella ) are oxidase-negative .
c) Staphylococcus species and d) Streptococcus species are also oxidase-negative (they use alternative enzymes for respiration).
105 / 118
Category:
ASCP Exam Questions
A urine isolate is non-lactose fermenting, motile, and phenylalanine deaminase-positive. The most likely genus is:
Non-lactose fermenting : This rules out many Enterobacteriaceae that ferment lactose (e.g., E. coli ).
Motile : Shigella (option d) is non-motile, so it can be excluded.
Phenylalanine deaminase (PAD) positive : This is a key test that narrows it down to Proteus , Morganella , and Providencia .
Edwardsiella (a) is PAD-negative.
Hafnia (c) is also PAD-negative.
Morganella is PAD-positive, motile, and non-lactose fermenting, fitting all the given characteristics.
106 / 118
Category:
ASCP Exam Questions
Which rapid test detects the presence of catalase enzyme using hydrogen peroxide?
The catalase test detects the enzyme catalase , which breaks down hydrogen peroxide (H₂O₂) into water (H₂O) and oxygen (O₂) .
When H₂O₂ is added to a bacterial colony:
Key Uses: ✔ Differentiates Staphylococcus (catalase-positive) from Streptococcus (catalase-negative). aerobic/anaerobic bacteria (most aerobes are catalase-positive).
Why Not the Other Tests? a) Oxidase test → Detects cytochrome oxidase (e.g., Pseudomonas , Neisseria ).
c) DNase test → Identifies DNA hydrolysis (e.g., Staphylococcus aureus ).
d) Nitrate reduction test → Checks for nitrate reductase activity.
107 / 118
Category:
ASCP Exam Questions
Which of the following tests differentiates Escherichia coli from Enterobacter cloacae?
The indole test is the key test to differentiate:
Escherichia coli : Indole-positive (produces indole from tryptophan, turning red with Kovac’s reagent).
Enterobacter cloacae : Indole-negative (no color change).
Why Not Other Tests? (b) Catalase test : Both are catalase-positive (not useful).
(c) Oxidase test : Both are oxidase-negative (typical of Enterobacteriaceae).
(d) Coagulase test : Used for Staphylococcus (irrelevant here).
109 / 118
Category:
ASCP Exam Questions
Which test is used to differentiate Proteus species from other Enterobacteriaceae?
The urease test is key to differentiating Proteus species (urease-positive) from most other Enterobacteriaceae (urease-negative):
Positive result : Rapid hydrolysis of urea → pink/red color (e.g., Proteus mirabilis , Proteus vulgaris ).
Negative result : No color change (e.g., E. coli , Klebsiella ).
Why Not Other Options? (a) Oxidase test : All Enterobacteriaceae are oxidase-negative (including Proteus ).
(c) Coagulase test : Used for Staphylococcus aureus (irrelevant here).
(d) Bile solubility test : Identifies Streptococcus pneumoniae (not Gram-negatives).
110 / 118
Category:
ASCP Exam Questions
The best medium for culture of Bordetella pertussis is:
Regan-Lowe agar is the optimal medium for culturing Bordetella pertussis (the causative agent of whooping cough ).
Contains charcoal, horse blood, and cephalexin (supports growth while inhibiting contaminants).
Starch in the medium absorbs toxic metabolites.
Why Not the Others?
(a) Phenylethyl alcohol agar : Selective for Gram-positives (e.g., Staphylococcus ), not Bordetella .
(b) Potassium tellurite blood agar : Used for Corynebacterium diphtheriae (turns colonies gray-black).
(d) Tinsdale agar : Also for C. diphtheriae (colonies turn brown-black with halo due to cystinase).
Alternative Media :
111 / 118
Category:
ASCP Exam Questions
Relapsing fever in humans is caused by:
Relapsing fever is caused by Borrelia recurrentis (louse-borne) or other Borrelia species (e.g., B. hermsii , tick-borne). These spirochetes evade the immune system by antigenic variation of surface proteins, leading to cyclic fever episodes.
Why Not Other Options? (b) Brucella abortus : Causes brucellosis (undulant fever), not relapsing fever.
(c) Leptospira interrogans : Causes leptospirosis (jaundice, renal failure).
(d) Spirillum minus : Causes rat-bite fever (sodoku), characterized by ulcerative lesions and arthritis.
112 / 118
Category:
ASCP Exam Questions
The string test producing a viscous “string” from a bacterial colony when mixed in sodium deoxycholate is characteristic of:
The string test is a rapid screening method to identify Vibrio cholerae .
When a colony of V. cholerae is mixed with a drop of 0.5% sodium deoxycholate solution , it lyses and releases viscous DNA , forming a mucoid “string” when the loop is lifted.
This occurs due to the release of extracellular polysaccharides and DNA from the lysed bacteria.
Why Not the Other Options? a) Escherichia coli → Does not produce a viscous string in this test.
c) Salmonella enterica → Negative in the string test.
d) Enterococcus faecalis → Unrelated to this test; it is a Gram-positive coccus.
113 / 118
Category:
ASCP Exam Questions
Which medium is used to detect lactose fermentation and differentiate Gram-negative enteric bacteria?
MacConkey agar is a selective and differential medium used to:
Detect lactose fermentation by Gram-negative enteric bacteria (e.g., E. coli , Klebsiella ).
Lactose fermenters : Pink/red colonies (due to acid production and neutral red dye uptake).
Non-lactose fermenters : Colorless/transparent colonies (e.g., Salmonella , Shigella ).
Inhibit Gram-positive bacteria (via bile salts and crystal violet).
Other options (incorrect):
(b) Blood agar → General-purpose medium for hemolysis (not selective for Gram-negatives).
(c) Mannitol salt agar → Selective for Staphylococcus (high salt; detects mannitol fermentation).
(d) Chocolate agar → Enriched medium for fastidious bacteria (e.g., Haemophilus , Neisseria ).
114 / 118
Category:
ASCP Exam Questions
Which of the following is a rapid test used to presumptively identify Moraxella catarrhalis?
The tributyrin hydrolysis test detects the enzyme butyrate esterase , which hydrolyzes tributyrin .
Moraxella catarrhalis is positive for this test and is one of the few Gram-negative diplococci that can rapidly hydrolyze tributyrin.
A positive result is a color change on the test disk (usually blue/green).
Other options: b) Oxidase test – Positive in M. catarrhalis , but not specific (many organisms are oxidase positive).
c) Indole test – M. catarrhalis is indole negative; not useful for ID.
d) Bile solubility test – Used for identifying Streptococcus pneumoniae, not Moraxella.
115 / 118
Category:
ASCP Exam Questions
A stool culture from a patient with bloody diarrhea grows lactose-negative colonies. Which selective medium would detect E. coli O157:H7?
Lactose-negative colonies in bloody diarrhea – Suggests Shiga toxin-producing E. coli (STEC) , particularly O157:H7 .
MacConkey sorbitol agar (SMAC) :
E. coli O157:H7 cannot ferment sorbitol (unlike 95% of other E. coli strains), producing colorless colonies on SMAC.
Standard MacConkey agar (lactose-based) would miss it, as most E. coli are lactose+.
Why Not the Others? a) Hektoen enteric (HE) agar – Selects for Salmonella /Shigella (lactose-negative), but O157:H7 may appear similar (not specific).
c) XLD agar – Used for Salmonella (red colonies with black centers) and Shigella (red colonies).
d) Salmonella-Shigella (SS) agar – Inhibits E. coli ; selects for Salmonella (colorless with black centers) and Shigella (colorless).
116 / 118
Category:
ASCP Exam Questions
For Campylobacter jejuni isolation, fecal specimens should be incubated:
Atmosphere :
Requires microaerophilic conditions (~5% O₂, 10% CO₂, 85% N₂).
Not aerobic (a), anaerobic (b), or ambient air (d).
Temperature :
Optimal growth at 42°C (selective for C. jejuni over other fecal flora).
35°C (a) is less selective, and 25°C (d) is too cold.
Special Media :
Why Not the Others? a) Aerobically at 35°C – Campylobacter does not grow in aerobic conditions.
b) Anaerobically at 42°C – Requires microaerophilic, not anaerobic, conditions.
d) Ambient air at 25°C – No growth; ambient O₂ levels are inhibitory, and temperature is too low.
117 / 118
Category:
ASCP Exam Questions
Which test differentiates Klebsiella pneumoniae from Enterobacter aerogenes?
To differentiate Klebsiella pneumoniae (non-motile) from Enterobacter aerogenes (motile), the motility test is key:
Why Not Other Tests? (b) Catalase test : Both are catalase-positive (not useful for differentiation).
(c) Oxidase test : Both are oxidase-negative (typical of Enterobacteriaceae).
(d) Indole test : While K. pneumoniae is usually indole-negative and E. aerogenes is always indole-negative, this test alone isn’t definitive.
118 / 118
Category:
ASCP Exam Questions
The primary function of selective media in bacteriology is:
Selective media contain specific inhibitors (e.g., antibiotics, salts, dyes) that:
Suppress unwanted bacteria (e.g., Gram-positives, non-target organisms).
Promote growth of desired bacteria (e.g., Gram-negatives, pathogens).
Examples: Why Not the Others? a) Colony color : A feature of differential media (e.g., blood agar for hemolysis).
b) Allow all growth : Contradicts the purpose of selectivity (general media like TSA do this).
d) Detect motility : Requires motility agar (stab inoculation), not selective media.
Your score is
The average score is 72%
Follow us on Sicial Media:
Restart quiz
📚 Who Should Use This Mock Test? This test is suitable for:
Medical Laboratory Scientists (MLS) preparing for ASCP or equivalent exams.Medical Laboratory Technicians (MLT) seeking international certifications.Microbiology students and interns improving their practical knowledge.Healthcare professionals refreshing bacteriology lab skills.📝 Take the Full Mock Test Now Challenge yourself with over 118 multiple-choice questions covering all essential analytic procedures in bacteriology. Each question is carefully crafted to match real exam standards, giving you an effective self-assessment tool.
✅ Key Benefits of This Test Free online access anytime. Realistic exam-style MCQs. Immediate answer key for self-checking. Supports preparation for multiple international lab exams. Top 8 Medical Laboratory Scientist (MLS) Exams: Top 8 Medical Laboratory Scientist (MLS) Exams that are recognized globally and can help professionals validate their credentials and enhance their career opportunities:
1. ASCP – American Society for Clinical Pathology (USA) Exam Name: MLS(ASCP)Eligibility: Bachelor’s degree with clinical laboratory experience.Global Recognition: HighPurpose: Certifies Medical Laboratory Scientists in the United States and internationally.2. AMT – American Medical Technologists (USA) Exam Name: MLT(AMT) or MT(AMT)Eligibility: Academic and/or work experience in medical laboratory technology.Global Recognition: ModeratePurpose: Credentialing for medical technologists and technicians.3. AIMS – Australian Institute of Medical and Clinical Scientists Exam Name: AIMS Certification ExamEligibility: Assessment of qualifications and work experience.Recognition: Required for practice in Australia.Purpose: Certification and registration in Australia.4. CSMLS – Canadian Society for Medical Laboratory Science Exam Name: CSMLS General or Subject-specific ExamsEligibility: Graduation from a CSMLS-accredited program or equivalent.Recognition: CanadaPurpose: Entry-to-practice certification in Canada.5. IBMS – Institute of Biomedical Science (UK) Exam Name: Registration and Specialist Portfolio AssessmentEligibility: Accredited degree and lab experience.Recognition: UK and some Commonwealth countries.Purpose: Biomedical Scientist registration with the HCPC (UK).6. HAAD / DOH – Department of Health, Abu Dhabi (UAE) Exam Name: DOH/HAAD License ExamEligibility: Degree in medical laboratory science and experience.Recognition: UAE (Abu Dhabi)Purpose: Licensure for medical laboratory practice in Abu Dhabi.7. DHA – Dubai Health Authority (UAE) Exam Name: DHA License Exam for Medical Laboratory TechnologistsEligibility: Relevant degree and experience.Recognition: Dubai, UAEPurpose: Professional license for clinical laboratory practice in Dubai.8. MOH – Ministry of Health (Gulf Countries like UAE, Saudi Arabia, Kuwait) Exam Name: MOH License ExamEligibility: BSc/Diploma in Medical Laboratory + experience.Recognition: Varies by country.Purpose: Required for practicing in public and private sector labs.Tags:
Possible References Used