Diverticulosis is a condition that primarily affects the large intestine (colon) and involves the formation of small pouches or pockets called diverticula in the wall of the colon. These diverticula can develop when weak spots in the muscular wall of the colon give way under pressure, causing the inner lining of the colon to protrude outward. Diverticulosis itself is generally not associated with any symptoms, but it can lead to more serious conditions if complications arise.

Definition of Diverticulosis:
Diverticulosis is a medical condition characterized by the presence of small pouches or pockets, known as diverticula, that form in the walls of the large intestine, specifically the colon. These diverticula develop when weak areas in the muscular layers of the colon allow the inner lining to protrude outward, forming small, balloon-like pouches. Diverticulosis itself often does not cause noticeable symptoms, and many individuals with this condition may be unaware of its presence.
The development of diverticula is often associated with increased pressure within the colon due to factors such as a low-fiber diet, which can lead to harder stools that require more force to move through the colon. The condition becomes more common as people age, particularly in individuals over the age of 40.
Causes and Risk Factors:
- Low-Fiber Diet: One of the primary factors contributing to diverticulosis is a diet low in dietary fiber. A diet lacking in fiber can lead to the formation of harder stools that require more force to move through the colon. This increased pressure can cause weak spots in the colon wall to bulge out and form diverticula.
- Age: Diverticulosis becomes more common as people age. It is most frequently diagnosed in individuals over the age of 40, and the prevalence tends to increase with advancing age.
- Genetics: There appears to be a genetic component to the development of diverticulosis. Individuals with a family history of the condition may be at a higher risk.
- Lifestyle Factors: Certain lifestyle factors can increase the risk of developing diverticulosis, including a sedentary lifestyle, obesity, and smoking.
- Lack of Exercise: Insufficient physical activity and a sedentary lifestyle can contribute to constipation and increased pressure in the colon, potentially promoting the formation of diverticula.
- Obesity: Being overweight or obese is associated with a higher risk of diverticulosis. Excess weight may contribute to increased pressure within the colon.
- Smoking: Smoking has been linked to an increased risk of diverticulosis, possibly due to its effects on blood vessels and inflammation.
- Medications: Long-term use of certain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and steroids, may be associated with an elevated risk of diverticulosis.
- Connective Tissue Disorders: Rare connective tissue disorders that affect the strength and integrity of the colon wall can predispose individuals to diverticulosis.
- Gender: Diverticulosis is slightly more common in men than in women.
Symptoms and Diagnosis:
These symptoms are often non-specific and can overlap with other gastrointestinal issues.
Symptoms of Diverticulitis:
Symptoms of diverticulitis can include.
- Abdominal Pain: Typically localized in the lower left side of the abdomen, but it can also be felt on the right side or throughout the abdomen. The pain may be constant or intermittent and can range from mild to severe.
- Fever and Chills: Inflammation or infection in the diverticula can lead to fever and chills, especially if an infection is present.
- Changes in Bowel Habits: Diverticulitis can cause changes in bowel movements, including diarrhea or constipation.
- Nausea and Vomiting: Some individuals with diverticulitis may experience nausea and vomiting.
Diagnosis:
Diagnosing diverticulosis and diverticulitis involves a combination of clinical evaluation, medical history, and diagnostic tests. Common diagnostic methods include:
- Physical Examination: A healthcare provider may perform a physical examination to assess abdominal tenderness, check for signs of infection, and evaluate overall health.
Imaging Tests:
- Colonoscopy: A procedure in which a thin, flexible tube with a camera is inserted through the rectum to examine the colon.
- Computed Tomography (CT) Scan: This imaging test can provide detailed images of the colon and help identify diverticula, inflammation, and other abnormalities.
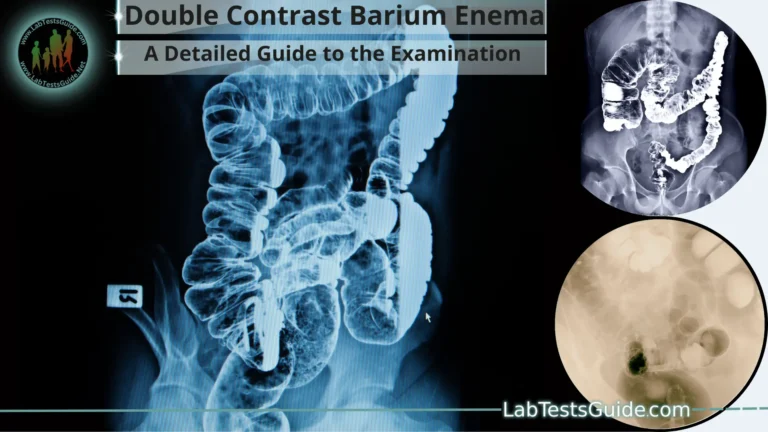
- Barium Enema: In this procedure, a contrast material containing barium is introduced into the colon through the rectum. X-rays are then taken to visualize the colon and its abnormalities.
- Blood Tests: Blood tests may be conducted to check for signs of infection (elevated white blood cell count) and inflammation (elevated C-reactive protein levels).
Stool Tests: Stool samples might be analyzed to rule out other gastrointestinal conditions.
Prevention and Lifestyle:
Here are some important prevention strategies and lifestyle changes.
- High-Fiber Diet: Consuming a diet rich in fiber can help prevent diverticulosis and promote overall digestive health. Fiber softens stools, making them easier to pass and reducing pressure within the colon. Good sources of fiber include whole grains, fruits, vegetables, legumes, and nuts.
- Stay Hydrated: Drinking plenty of water helps maintain soft and regular bowel movements, preventing constipation and reducing the risk of diverticula formation.
- Regular Exercise: Engaging in regular physical activity can promote proper bowel function and prevent constipation. Aim for at least 30 minutes of moderate exercise most days of the week.
- Maintain a Healthy Weight: Being overweight or obese increases the risk of diverticulosis. Adopting a balanced diet and staying physically active can help maintain a healthy weight.
- Avoid Smoking: If you smoke, quitting is beneficial for your overall health, including reducing the risk of diverticulosis and its complications.
- Limit Red Meat and Processed Foods: A diet high in red meat and processed foods has been associated with a higher risk of diverticulitis. Aim to consume these foods in moderation and focus on whole, unprocessed options.
- Moderate Alcohol Consumption: Limit alcohol intake to moderate levels. Excessive alcohol consumption can irritate the gastrointestinal tract and potentially worsen symptoms.
- Practice Good Bowel Habits: Avoid delaying bowel movements when you feel the urge to go, as this can lead to constipation and increased pressure in the colon.
- Consider Fiber Supplements: If it’s challenging to get enough fiber from your diet, you can consider taking fiber supplements. However, it’s generally better to get fiber from whole foods.
- Limit Foods Low in Fiber: Foods low in fiber, such as refined grains and certain dairy products, should be consumed in moderation.
- Manage Stress: Chronic stress can affect digestive health. Engage in relaxation techniques, such as meditation, yoga, or deep breathing exercises, to help manage stress.
- Regular Check-Ups: Schedule regular visits to your healthcare provider for check-ups. Discuss your risk factors, lifestyle habits, and any gastrointestinal symptoms you may be experiencing.
Treatment Options:
Here are some treatment options.
- Dietary Modifications: For uncomplicated diverticulosis, making dietary changes is often the first step. Increasing dietary fiber intake can help soften stools and prevent constipation, reducing the risk of diverticula formation and minimizing symptoms. Foods rich in fiber, such as whole grains, fruits, vegetables, legumes, and nuts, should be included in the diet.
- Fiber Supplements: If it’s challenging to get enough fiber from the diet, fiber supplements (e.g., psyllium) can be taken as directed by a healthcare provider. These supplements can help improve bowel regularity and prevent constipation.
- Medications for Diverticulitis: If diverticulitis occurs and is mild to moderate in severity, your doctor may prescribe antibiotics to treat the infection and reduce inflammation. Pain relievers may also be recommended to manage discomfort.
- Rest and Fluids: During episodes of diverticulitis, rest and increased fluid intake are important. Rest allows the colon to heal, and proper hydration helps maintain overall health and supports recovery.
- Hospitalization and Intravenous (IV) Antibiotics: In severe cases of diverticulitis, hospitalization may be necessary. Intravenous antibiotics and fluids can be administered to manage the infection and inflammation more effectively.
Surgical Interventions:
Surgical options include.
- Primary Bowel Resection: This involves removing the affected portion of the colon and reattaching the healthy ends.
- Bowel Resection with Colostomy: In more complex cases, a temporary or permanent colostomy (an opening through the abdominal wall to divert stool) might be necessary.
Complications:
Here are some potential complications associated with diverticulosis:
Diverticulitis:
Diverticulitis can lead to complications such as.
- Abscess Formation: Inflammation can result in the development of pus-filled pockets (abscesses) near the affected diverticula.
- Perforation: If an inflamed diverticulum bursts or tears, it can lead to a perforation (hole) in the colon wall. This can allow stool and bacteria to leak into the abdominal cavity, leading to a serious infection known as peritonitis.
- Fistula Formation: An abnormal connection (fistula) can form between the colon and other nearby organs, such as the bladder or the skin. This can lead to complications and require medical intervention.
- Bowel Obstruction: Though less common, diverticulosis can lead to a partial or complete blockage of the colon, causing bowel obstruction. This can result from inflammation, scarring, or narrowing of the colon due to repeated episodes of diverticulitis.
- Bleeding: Bleeding can occur from blood vessels near the diverticula. This can lead to rectal bleeding, which may be bright red or maroon in color. While diverticulosis-related bleeding is usually not severe, it can still cause significant discomfort and require medical evaluation.
- Chronic Symptoms: Some individuals with diverticulosis may experience chronic symptoms such as bloating, cramping, and changes in bowel habits. While these symptoms might not be as severe as acute diverticulitis, they can still affect quality of life.
Management of Diverticulitis:
Here are the general approaches to managing diverticulitis:
Mild Diverticulitis:
The following management strategies are often recommended.
- Rest and Clear Liquid Diet: Resting and consuming a clear liquid diet (water, broth, clear juices, tea, etc.) for a short period can help the inflamed colon recover.
- Gradual Transition to Low-Fiber Diet: After the acute phase, transitioning to a low-fiber diet is often advised. This allows the colon to heal while minimizing the risk of further irritation. Low-fiber foods may include well-cooked vegetables, refined grains, and lean proteins.
- Antibiotics: Your doctor may prescribe antibiotics to help treat the infection and reduce inflammation.
Severe Diverticulitis or Complications:
For severe cases of diverticulitis or when complications like abscesses, perforations, or fistulas are present, more intensive management is necessary:
- Hospitalization: Severe cases often require hospitalization. This allows for closer monitoring, intravenous antibiotics, and appropriate management of complications.
- NPO and Intravenous (IV) Fluids: Patients may be asked to refrain from eating and drinking (NPO) to allow the colon to rest. Intravenous fluids are administered to maintain hydration and provide necessary nutrients.
- Possible Surgical Intervention: Surgery might be considered if there’s a risk of complications, if the patient doesn’t respond to medical treatment, or if recurrent episodes of diverticulitis occur. Surgical options may involve removing the affected portion of the colon or creating a temporary or permanent colostomy.
Recovery and Aftercare:
- Gradual Diet Transition: As the inflammation subsides, you’ll gradually reintroduce higher-fiber foods to your diet to support bowel regularity and overall digestive health.
- Hydration: Continue to drink plenty of fluids to maintain hydration and support healthy digestion.
- Lifestyle Modifications: Focus on adopting a healthier lifestyle, including a high-fiber diet, regular exercise, and stress management, to help prevent future episodes.
Long-Term Outlook:
- Diverticulosis: Diverticulosis itself is usually a benign condition, and many people with diverticula never experience complications or symptoms. With appropriate dietary and lifestyle changes, such as adopting a high-fiber diet and staying hydrated, you can often manage diverticulosis effectively and prevent its progression.
- Diverticulitis: The outlook for diverticulitis depends on its severity and the promptness of treatment. Mild cases of diverticulitis that are managed early and effectively generally have a good prognosis. However, if left untreated or if complications arise, such as perforation or abscess formation, the condition can become more serious and require more intensive interventions, including surgery.
- Prevention and Management: Adopting a healthy lifestyle, including maintaining a high-fiber diet, staying active, managing stress, and avoiding smoking, can significantly reduce the risk of diverticulosis and diverticulitis. Proper management of diverticulitis episodes through rest, dietary adjustments, antibiotics, and potential surgical intervention when necessary can also contribute to positive outcomes.
- Long-Term Monitoring: If you have a history of diverticulosis or diverticulitis, it’s important to continue regular check-ups with your healthcare provider. They can monitor your condition, assess the effectiveness of your management plan, and provide guidance on maintaining your digestive health.
- Complications and Recurrence: While most individuals can effectively manage diverticulosis and diverticulitis, there is a risk of recurrence. Adhering to a high-fiber diet and adopting a healthy lifestyle can help minimize the risk of recurrence. Complications such as abscesses, perforations, or fistulas are more common in severe cases of diverticulitis, but with appropriate treatment, they can often be managed successfully.
FAQs:
What is the difference between diverticulosis and diverticulitis?
Diverticulosis refers to the presence of small pouches (diverticula) in the colon wall without inflammation or infection.
Diverticulitis is a condition where one or more diverticula become inflamed or infected, leading to symptoms such as abdominal pain, fever, and changes in bowel habits.
Can diverticulosis be reversed?
Diverticulosis itself cannot be reversed, but its progression and associated complications can often be prevented or managed through dietary and lifestyle changes.
Can stress trigger diverticulitis?
While stress is not a direct cause of diverticulitis, chronic stress can affect digestive health and potentially contribute to exacerbating symptoms or triggering flare-ups.
Is surgery always necessary for diverticulitis?
Surgery is usually reserved for severe cases of diverticulitis, complications, or cases where other treatments have not been effective. Most cases of uncomplicated diverticulitis can be managed with rest, antibiotics, and dietary adjustments.
Can I still eat nuts and seeds if I have diverticulosis?
In the past, it was commonly believed that nuts and seeds should be avoided by individuals with diverticulosis. However, current research suggests that moderate consumption of nuts and seeds is generally safe and might even have health benefits. Always consult your healthcare provider for personalized dietary recommendations.
What’s the role of antibiotics in treating diverticulitis?
Antibiotics are often prescribed to treat the infection and inflammation associated with diverticulitis. They help control the infection and prevent complications. The choice of antibiotics and duration of treatment depend on the severity of the condition.
Can I prevent diverticulosis through diet alone?
A healthy, high-fiber diet can significantly reduce the risk of diverticulosis by promoting regular bowel movements and preventing constipation. However, other factors like genetics and age can also play a role.
Can diverticulosis lead to colon cancer?
There is no direct link between diverticulosis and colon cancer. However, both conditions can occur in the same individual. Regular screenings for colon cancer are important, especially as you age.
What’s the recommended daily fiber intake for preventing diverticulosis?
The recommended daily fiber intake varies based on age, gender, and individual health needs. Generally, aiming for 25 to 38 grams of fiber per day is recommended to support digestive health.
Can I resume my normal activities after an episode of diverticulitis?
After an episode of diverticulitis, your doctor will provide guidance on when it’s safe to resume normal activities. In mild cases, you may be able to gradually return to your regular routine once symptoms subside. In severe cases, additional recovery time might be necessary.
Conclusion:
In conclusion, diverticulosis is a common condition characterized by the formation of small pouches, or diverticula, in the colon wall, often caused by a low-fiber diet and aging. While usually asymptomatic, it can lead to diverticulitis—an inflammation of these pouches that presents with abdominal pain, fever, and changes in bowel habits. Prevention and management involve adopting a high-fiber diet, maintaining a healthy lifestyle, and seeking medical attention promptly for complications. With proper care and attention, individuals can effectively manage these conditions and lead healthy lives while minimizing the risk of complications.
Possible References Used