Bone marrow is a soft, spongy tissue found inside the bones of vertebrates. It plays a crucial role in the production of blood cells and the immune system. There are two types of bone marrow: red marrow and yellow marrow.

What is Bone Marrow?
Bone marrow is a soft, spongy tissue found inside the bones of vertebrates, including humans. It is a vital component of the body’s hematopoietic system, responsible for the production of blood cells and supporting the immune system. The marrow is surrounded by hard bone, and its primary function is the formation and maturation of various types of blood cells, which are essential for carrying out crucial functions within the body.
Types of Bone Marrow:
There are two main types of bone marrow based on their cellular composition and functions.
Red Marrow:
- Red marrow, also known as myeloid tissue, is the active, hematopoietic type of bone marrow responsible for the production of blood cells.
- It is found primarily in the spongy or trabecular bone regions, such as the vertebrae, ribs, sternum, pelvis, and the ends of long bones (e.g., femur and humerus).
- Red marrow contains hematopoietic stem cells (HSCs) or pluripotent stem cells. These stem cells can differentiate into various blood cell lineages, including red blood cells (erythrocytes), white blood cells (leukocytes), and platelets (thrombocytes).
- Hematopoiesis, the process of blood cell formation, occurs within the red marrow, making it a crucial site for maintaining the body’s blood cell levels and immune function.
- In newborns and young children, nearly all bone marrow is red marrow, but as a person ages, some red marrow is gradually replaced by yellow marrow, especially in the long bones.
Yellow Marrow:
- Yellow marrow, also known as fatty marrow, is a type of bone marrow that contains a higher proportion of fat cells and a lower concentration of blood-forming cells.
- It is found in the central cavities of certain bones, such as the long bones (e.g., femur and humerus) and flat bones (e.g., sternum and ribs).
- Yellow marrow serves as an energy reserve and is less involved in active blood cell production compared to red marrow.
- Despite its reduced hematopoietic activity, yellow marrow still possesses the potential to revert to red marrow and resume hematopoiesis in response to certain conditions, such as severe blood loss or specific diseases.
Hematopoiesis: Blood Cell Formation:
Here is an overview of the key aspects of hematopoiesis.
Hematopoietic Stem Cells (HSCs):
- Hematopoiesis begins with hematopoietic stem cells, which are undifferentiated cells found within the bone marrow. These stem cells have the unique ability to self-renew (produce more stem cells) and differentiate into different types of blood cells.
- HSCs are multipotent, meaning they can give rise to multiple cell lineages, including myeloid cells (red blood cells, white blood cells, and platelets) and lymphoid cells (B-cells, T-cells, and natural killer cells).
Differentiation of Blood Cells:
- Hematopoietic stem cells undergo a process of differentiation, where they become committed to specific blood cell lineages. This process is tightly regulated by various signaling pathways and transcription factors.
- Myeloid Lineage: Some HSCs differentiate into myeloid progenitor cells, which further differentiate into erythroid progenitor cells (red blood cells), myeloblasts (granulocytes like neutrophils, eosinophils, and basophils), monoblasts (monocytes), and megakaryoblasts (platelets).
- Lymphoid Lineage: Other HSCs differentiate into lymphoid progenitor cells, which give rise to lymphoblasts. Lymphoblasts further mature into B-cells, T-cells, and natural killer (NK) cells.
Regulation of Hematopoiesis:
- Hematopoiesis is tightly regulated by various growth factors, cytokines, and hormones. These factors control the proliferation, differentiation, and survival of blood cell precursors.
- Key regulators of hematopoiesis include erythropoietin (EPO) for red blood cell production, granulocyte colony-stimulating factor (G-CSF) for granulocyte production, and thrombopoietin (TPO) for platelet production, among others.
- The balance between cell production, differentiation, and cell death is crucial to maintain the appropriate number and types of blood cells in circulation.
Maturation and Release of Blood Cells:
- As blood cells mature, they develop specific characteristics and functions necessary for their roles in the body.
- Mature blood cells are released into the bloodstream, where they circulate to various tissues and organs to carry out their respective functions.
- Red blood cells transport oxygen from the lungs to body tissues, white blood cells defend against infections and provide immune responses, and platelets are involved in blood clotting.
Components of Bone Marrow:
Here are the key components of bone marrow.
Cellular Components:
- Hematopoietic Stem Cells (HSCs): These are multipotent stem cells that have the unique ability to differentiate into various blood cell lineages, including red blood cells, white blood cells, and platelets. HSCs are responsible for the continuous renewal of blood cells throughout life.
- Progenitor Cells: These are the immediate descendants of hematopoietic stem cells and are more committed to a specific blood cell lineage. Progenitor cells undergo limited differentiation and give rise to more specialized precursor cells.
- Precursor Cells: Precursor cells are the immediate precursors to mature blood cells. They undergo further differentiation and maturation before becoming fully functional blood cells.
- Mature Blood Cells: These are fully differentiated and functional blood cells that are released into the bloodstream to carry out their respective roles. Mature blood cells include red blood cells (erythrocytes), white blood cells (leukocytes), and platelets (thrombocytes).
Stromal Cells:
Mesenchymal Stem Cells (MSCs): Stromal cells within the bone marrow include mesenchymal stem cells, which are multipotent cells capable of differentiating into various connective tissue cells. MSCs play a crucial role in supporting the microenvironment of the bone marrow and providing structural support for hematopoietic cells.- Endothelial Cells: These cells form the inner lining of blood vessels and are essential for maintaining blood vessel integrity and regulating blood flow within the bone marrow.
- Extracellular Matrix (ECM): The extracellular matrix is a network of proteins and fibers that provide structural support and help create the microenvironment within the bone marrow. The ECM plays a crucial role in regulating hematopoiesis and influencing the behavior and function of hematopoietic cells.
- Cytokines and Growth Factors: Cytokines and growth factors are signaling molecules that regulate the proliferation, differentiation, and survival of blood cell precursors. These factors are secreted by various cell types within the bone marrow microenvironment and play a central role in hematopoiesis.
- Blood Vessels and Nerves: The bone marrow contains a rich network of blood vessels that supply nutrients and oxygen to the hematopoietic cells and remove waste products. Nerves also innervate the bone marrow, contributing to the regulation of hematopoiesis and the modulation of immune responses.
Bone Marrow Microenvironment:
Here are the key aspects of the bone marrow microenvironment.
Cellular Components:
- Mesenchymal Stem Cells (MSCs): MSCs are multipotent stromal cells found in the bone marrow, and they play a central role in forming the bone marrow microenvironment. MSCs can differentiate into various cell types, including osteoblasts (bone-forming cells), adipocytes (fat cells), and chondrocytes (cartilage cells). They also secrete important factors that regulate hematopoiesis and support the maintenance of HSCs.
- Endothelial Cells: Endothelial cells form the inner lining of blood vessels within the bone marrow. They help regulate blood flow and nutrient delivery to hematopoietic cells, and they also release factors that influence HSC function.
- Osteoblasts and Osteoclasts: Osteoblasts are involved in bone formation, and osteoclasts are responsible for bone resorption. The balance between bone formation and resorption affects the structure of the bone marrow microenvironment and influences hematopoiesis.
- Macrophages: Macrophages are immune cells that reside in the bone marrow and play a role in the removal of cellular debris and apoptotic cells. They also contribute to immune regulation and support hematopoiesis through cytokine secretion.
Non-Cellular Components:
- Extracellular Matrix (ECM): The ECM is a complex network of proteins and fibers that provides structural support for cells within the bone marrow. It also contains binding sites for cell adhesion and signaling molecules that help regulate hematopoiesis.
- Cytokines and Growth Factors: Various cytokines and growth factors are produced by stromal cells, endothelial cells, and other components of the microenvironment. These signaling molecules play a critical role in regulating the behavior of HSCs and blood cell progenitors.
Nerves and Neural Cells:
- Nerves and neural cells innervate the bone marrow and influence hematopoiesis through the release of neurotransmitters and neuropeptides. The nervous system can also modulate immune responses within the bone marrow.
Bone Marrow Aspiration and Biopsy:
Bone Marrow Aspiration:
- Bone marrow aspiration is a relatively less invasive procedure that involves the extraction of a small amount of liquid bone marrow from the bone marrow cavity. It is commonly performed on the posterior iliac crest (hip bone) in adults, and on other bones, such as the sternum or tibia, in specific cases.
- The procedure is typically carried out using a thin, hollow needle that is inserted through the skin and into the bone marrow cavity. The needle is then advanced into the spongy bone to aspirate (suction) a liquid sample of bone marrow.
- Local anesthesia is usually administered to minimize discomfort during the procedure.
- The obtained bone marrow sample is examined under a microscope to assess the cellular composition, including the presence of blood cells, progenitor cells, and abnormal cells.
Bone Marrow Biopsy:
- Bone marrow biopsy is a more invasive procedure that involves the removal of a small core of bone and marrow tissue from the bone marrow cavity.
- Similar to bone marrow aspiration, the biopsy is often performed on the posterior iliac crest in adults, and other bones may be used in specific situations.
- A larger, slightly wider needle is used to obtain the bone marrow biopsy sample.
- Local anesthesia is administered to numb the area before the procedure.
- The needle is carefully advanced into the bone, and a small core of bone and marrow is removed.
- The biopsy sample provides information about the cellular composition of the bone marrow and also offers insights into the bone structure and architecture.
Uses of Bone Marrow Aspiration and Biopsy:
- Diagnosis of Blood Disorders: Bone marrow samples are crucial in diagnosing various blood-related conditions, such as leukemia, lymphoma, anemia, and myelodysplastic syndromes (MDS).
- Staging and Monitoring: The procedures help assess the extent of disease progression and the effectiveness of treatments in hematological disorders.
- Donor Compatibility: In bone marrow transplantation, the compatibility of a potential donor’s bone marrow with the recipient is determined through these procedures.
- Investigating Unexplained Symptoms: Bone marrow tests may be used when other diagnostic methods are inconclusive in investigating certain symptoms or abnormalities.
Bone Marrow Disorders:
Some common bone marrow disorders include:
- Anemia: Anemia is a condition characterized by a decrease in the number of red blood cells or a low level of hemoglobin in the blood. It can result from various causes, including nutritional deficiencies (e.g., iron deficiency anemia), chronic diseases, blood loss, or inherited conditions affecting hemoglobin production.
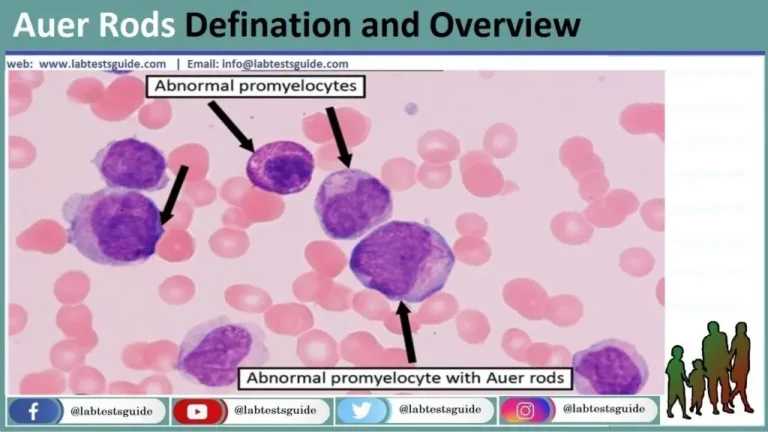
- Leukemia: Leukemia is a type of cancer that affects the bone marrow and blood. It is characterized by the uncontrolled proliferation of abnormal white blood cells (leukocytes). Leukemia can be acute or chronic and can involve different types of white blood cells, such as lymphocytes or myeloid cells.
- Lymphoma: Lymphoma is another type of blood cancer that primarily affects lymphocytes, a type of white blood cell. It usually starts in the lymph nodes but can involve the bone marrow as the disease progresses.
- Multiple Myeloma: Multiple myeloma is a cancer that originates from plasma cells, a type of white blood cell responsible for producing antibodies. It can lead to the overproduction of abnormal plasma cells and the accumulation of harmful proteins in the bone marrow and blood.
- Aplastic Anemia: Aplastic anemia is a rare and serious disorder in which the bone marrow fails to produce enough blood cells, including red blood cells, white blood cells, and platelets. It may be acquired (often due to immune system dysfunction) or inherited.
- Myelodysplastic Syndromes (MDS): MDS refers to a group of disorders in which the bone marrow does not produce mature and fully functional blood cells. Instead, there is an accumulation of immature cells called blasts, leading to a variety of blood abnormalities.
- Thrombocytopenia: Thrombocytopenia is a condition characterized by a low platelet count in the blood. It can result in an increased risk of bleeding and difficulty in clotting.
- Polycythemia Vera: Polycythemia vera is a rare blood disorder characterized by the overproduction of red blood cells, leading to an increase in blood viscosity. It can also cause an elevation in white blood cell and platelet counts.
- Hemophilia: Hemophilia is a genetic disorder that affects blood clotting. People with hemophilia have deficiencies in specific clotting factors, leading to prolonged bleeding episodes even after minor injuries.
Bone Marrow Transplantation:
Types of Bone Marrow Transplantation.
- Autologous Transplantation: In autologous transplantation, the patient’s own stem cells are collected and stored before undergoing high-dose chemotherapy or radiation therapy to treat certain types of cancer, such as lymphoma or multiple myeloma. After the treatment, the stored stem cells are infused back into the patient to help restore blood cell production.
- Allogeneic Transplantation: In allogeneic transplantation, stem cells are obtained from a compatible donor, typically a sibling, another family member, or an unrelated donor with a closely matched human leukocyte antigen (HLA) tissue type. Allogeneic transplantation offers the potential for a complete immune system replacement and is used to treat various hematological disorders, including leukemia, aplastic anemia, and certain immunodeficiencies.
- Syngeneic Transplantation: Syngeneic transplantation involves the use of stem cells from an identical twin as the donor. Since the donor and recipient have an identical genetic makeup, there is no risk of graft-versus-host disease (GVHD), a potentially severe complication of allogeneic transplantation.
The Bone Marrow Transplantation Process:
- Conditioning Regimen: Before the transplant, the patient typically undergoes a conditioning regimen, which includes high-dose chemotherapy, radiation therapy, or a combination of both. The conditioning serves to destroy cancer cells (in the case of cancer treatment) and suppress the recipient’s immune system to prevent rejection of the donor cells.
- Stem Cell Collection: For allogeneic and autologous transplants, stem cells are collected from the donor (allogeneic) or the patient (autologous). Stem cells may be collected from the bone marrow, peripheral blood, or umbilical cord blood.
- Transplantation: The collected stem cells are infused into the recipient’s bloodstream through a process similar to a blood transfusion. Once infused, the stem cells migrate to the bone marrow and begin to produce healthy blood cells.
- Engraftment: The period following transplantation is called the engraftment phase. During this time, the transplanted stem cells start to grow and produce new blood cells in the recipient’s bone marrow.
- Post-Transplant Care: After the transplantation, the patient is closely monitored for engraftment, complications, and signs of graft-versus-host disease (in allogeneic transplantation). Immunosuppressive medications may be given to prevent GVHD.
Bone Marrow in Immune System Function:
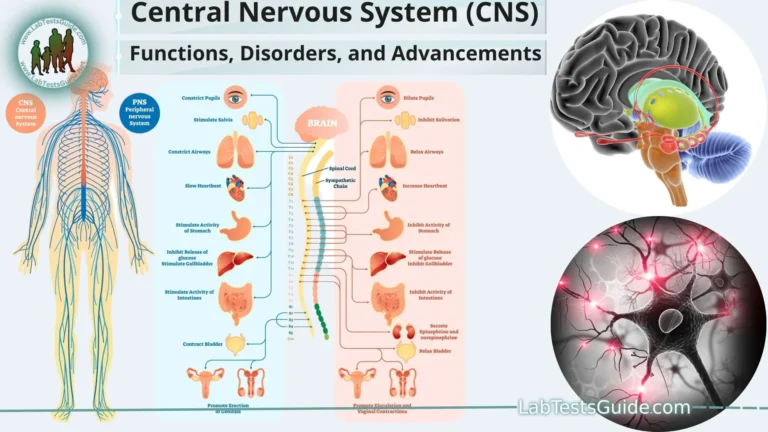
- Production of Immune Cells: Hematopoietic stem cells (HSCs) in the bone marrow give rise to all blood cells, including immune cells. These stem cells differentiate into different lineages of immune cells, which are essential for the body’s defense against infections and foreign substances.
- B-Cells: B-cells, a type of white blood cell, are produced and mature in the bone marrow. They play a crucial role in the humoral immune response by producing antibodies that specifically target and neutralize pathogens, such as bacteria and viruses.
- T-Cells: T-cells, another type of white blood cell, are also produced in the bone marrow but mature in the thymus gland (hence the name T-cells). T-cells are involved in the cell-mediated immune response, where they directly recognize and destroy infected cells and cancer cells.
- Natural Killer (NK) Cells: NK cells are a type of cytotoxic lymphocyte that plays a role in the innate immune response. They are produced in the bone marrow and are responsible for detecting and killing infected or abnormal cells, including virus-infected cells and tumor cells.
- Immune Cell Maturation and Education: Within the bone marrow and thymus, developing immune cells undergo a process of maturation and education. During this process, they are exposed to various antigens (substances that trigger an immune response), and those immune cells that recognize self-antigens are eliminated or suppressed to prevent autoimmune responses.
- Immune Cell Activation and Proliferation: The bone marrow provides a supportive microenvironment that aids in the activation and proliferation of immune cells. Stromal cells, endothelial cells, and cytokines within the bone marrow facilitate the proper functioning and expansion of immune cells.
- Immune Memory: Memory B-cells and memory T-cells, which are responsible for immune memory, are also generated in the bone marrow and thymus. These memory cells “remember” previous encounters with pathogens, allowing for a faster and more effective immune response upon subsequent exposure to the same pathogen.
Current Research and Advances:
Some insights into potential research areas and recent advances up to that point.
- Stem Cell Transplantation Techniques: Researchers were exploring innovative approaches to improve the success rates and reduce complications of bone marrow and hematopoietic stem cell transplantation. This included novel conditioning regimens, refined graft selection, and the use of alternative stem cell sources, such as umbilical cord blood and haploidentical (half-matched) donors.
- Gene Editing and Gene Therapy: Advances in gene editing technologies, like CRISPR-Cas9, opened up possibilities for treating genetic blood disorders. Researchers were exploring gene therapy approaches to correct genetic mutations in bone marrow cells to treat conditions like sickle cell anemia and thalassemia.
- Immunotherapy and CAR-T Cell Therapy: Immunotherapies, such as chimeric antigen receptor (CAR) T-cell therapy, showed promise in the treatment of certain types of leukemia and lymphoma. These therapies involved modifying a patient’s immune cells to recognize and attack cancer cells.
- Understanding Bone Marrow Microenvironment: Research focused on gaining a deeper understanding of the bone marrow microenvironment and its impact on hematopoiesis and immune function. This included investigating stromal cells, cytokines, and growth factors that regulate blood cell production and immune responses.
- Targeted Therapies for Blood Cancers: Ongoing studies were exploring targeted therapies that specifically inhibit abnormal signaling pathways in cancer cells, leading to more effective and less toxic treatments for blood cancers.
- Immunomodulatory Drugs: Researchers were investigating new drugs that could modulate the immune system to enhance the response against cancer cells or suppress autoimmunity in certain diseases.
- Biomarkers and Diagnostic Tools: Efforts were being made to identify biomarkers and develop advanced diagnostic tools for early detection and monitoring of bone marrow disorders.
- Personalized Medicine: The concept of personalized medicine was gaining traction in the field of bone marrow research, tailoring treatment approaches based on a patient’s individual genetic profile and disease characteristics.
FAQs:
What is bone marrow, and what is its function?
Bone marrow is a soft, spongy tissue found inside bones. Its primary function is to produce and mature various types of blood cells, including red blood cells, white blood cells, and platelets. These blood cells are crucial for oxygen transport, immune responses, and blood clotting.
What are the types of bone marrow?
There are two main types of bone marrow: red marrow and yellow marrow. Red marrow is the active, hematopoietic type responsible for blood cell production. Yellow marrow contains a higher proportion of fat cells and has a lower hematopoietic capacity.
What is hematopoiesis?
Hematopoiesis is the process of blood cell formation that occurs in the bone marrow. It involves the differentiation of hematopoietic stem cells into different blood cell lineages, ensuring a continuous supply of functional blood cells.
What is the bone marrow microenvironment?
The bone marrow microenvironment, also known as the bone marrow niche, refers to the specialized cellular and non-cellular components that support and regulate hematopoietic stem cells and blood cell production.
What are bone marrow aspiration and biopsy?
Bone marrow aspiration and biopsy are medical procedures used to obtain samples of bone marrow for diagnostic and therapeutic purposes. Aspiration involves extracting liquid bone marrow, while biopsy involves removing a small core of bone and marrow tissue.
What are some common bone marrow disorders?
Common bone marrow disorders include anemia, leukemia, lymphoma, multiple myeloma, aplastic anemia, myelodysplastic syndromes (MDS), and thrombocytopenia.
What is bone marrow transplantation?
Bone marrow transplantation, or hematopoietic stem cell transplantation, is a medical procedure where healthy stem cells are infused into a recipient’s bloodstream to replace damaged or diseased bone marrow. It is used to treat various cancers, genetic blood disorders, and immune deficiencies.
How does bone marrow contribute to immune system function?
Bone marrow is responsible for producing and maturing immune cells, such as B-cells, T-cells, and natural killer (NK) cells. It also plays a role in immune cell activation, proliferation, and the development of immune memory.
What are some recent advances in bone marrow research?
As of the last update in September 2021, recent advances included exploring new stem cell transplantation techniques, gene editing and gene therapy for genetic blood disorders, immunotherapy and CAR-T cell therapy for blood cancers, and a deeper understanding of the bone marrow microenvironment.
Is bone marrow transplantation risky?
Bone marrow transplantation is a complex and intensive procedure with potential risks and complications, including graft failure, infections, and graft-versus-host disease (GVHD). However, it can offer life-saving treatment for various conditions when performed by skilled medical teams in specialized facilities.
Conclusion:
In conclusion, bone marrow serves as a critical component of the hematopoietic system, playing a central role in blood cell production, immune system function, and overall health. It is responsible for generating and maturing various types of blood cells, including red blood cells, white blood cells, and platelets, which are essential for oxygen transport, immune responses, and clotting. The bone marrow microenvironment supports and regulates the development of immune cells and provides a nurturing setting for the hematopoietic process. Furthermore, bone marrow aspiration and biopsy are valuable diagnostic tools for understanding and diagnosing various bone marrow disorders. Advancements in bone marrow transplantation, gene editing, immunotherapies, and personalized medicine continue to improve treatment outcomes and expand our understanding of this intricate and vital tissue.
Possible References Used