Ascites is a medical condition characterized by the abnormal accumulation of fluid in the abdominal cavity. This fluid buildup leads to abdominal swelling and distension. Ascites can be a sign of an underlying medical problem and is most commonly associated with liver disease, particularly cirrhosis.

Definition of Ascites.
Ascites is a medical condition characterized by the abnormal accumulation of fluid in the abdominal cavity, specifically within the peritoneal cavity. This buildup of fluid results in abdominal swelling and distension, which can be visually noticeable and often causes discomfort. Ascites is not a disease itself but is typically a symptom or sign of an underlying medical condition, with the most common cause being liver cirrhosis. It can also be associated with various other health issues, including heart failure, kidney disease, certain cancers, and infections. Ascites may be diagnosed through physical examinations, medical history review, imaging tests, and analysis of the fluid that has accumulated in the abdomen. Treatment of ascites involves addressing the underlying cause and managing the fluid accumulation to alleviate symptoms and prevent complications.
Causes of Ascites:
Here is a list of common causes of ascites.
- Liver Cirrhosis: This is the leading cause of ascites. Cirrhosis is a late stage of scarring (fibrosis) of the liver caused by long-term liver damage, often due to excessive alcohol consumption, chronic viral hepatitis, or other liver diseases. The damaged liver is less able to process fluids, leading to fluid accumulation in the abdomen.
- Heart Failure: Congestive heart failure can cause fluid to back up into the abdominal cavity, leading to ascites. The heart’s inability to pump blood effectively can result in increased pressure in the veins and capillaries, causing fluid leakage into the abdomen.
- Kidney Disease: Severe kidney disease can lead to a decrease in the elimination of excess fluid and sodium from the body. This fluid retention can cause ascites.
- Cancer: Certain cancers, particularly advanced abdominal cancers like ovarian, pancreatic, or stomach cancer, can cause ascites as they grow and affect the peritoneal lining.
- Infections: Infections within the peritoneal cavity can lead to ascites. One example is spontaneous bacterial peritonitis (SBP), which is an infection of the ascitic fluid.
- Portal Hypertension: Elevated pressure in the portal vein, which carries blood from the digestive organs to the liver, can lead to ascites. Portal hypertension can be caused by cirrhosis or other conditions that obstruct blood flow through the liver.
- Pancreatitis: Inflammation of the pancreas can lead to ascites, although it’s relatively less common.
- Malnutrition: Severe malnutrition, often seen in conditions like protein-losing enteropathy, can result in low levels of proteins (albumin) in the blood. Low albumin levels can lead to fluid leakage from blood vessels into the abdominal cavity.
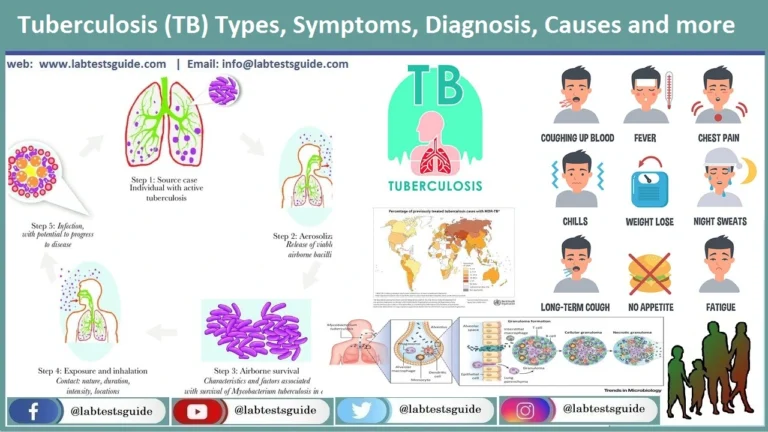
- Tuberculosis: In some cases, tuberculosis (TB) can cause peritoneal tuberculosis, leading to ascites.
- Other Causes: Ascites can also result from less common causes, such as certain autoimmune diseases, abdominal trauma, and congestive splenomegaly.
Symptoms of Ascites:
Common symptoms of ascites include.
- Abdominal Swelling: The most prominent and noticeable symptom of ascites is the progressive enlargement of the abdomen. The abdomen becomes distended and appears swollen or bloated. The degree of swelling can vary from mild to severe.
- Weight Gain: Due to the accumulation of fluid, individuals with ascites often experience unexplained weight gain, even when they haven’t increased their food intake.
- Difficulty Breathing: As the abdomen becomes distended, it can put pressure on the diaphragm and limit its movement. This can lead to shortness of breath or difficulty breathing, especially when lying flat.
- Abdominal Discomfort and Pain: Some individuals may experience discomfort or mild pain in the abdominal area. This discomfort can result from the stretching of the abdominal wall due to the increased fluid volume.
- Nausea and Vomiting: Ascites can sometimes cause nausea and vomiting, which may be related to the pressure exerted on the stomach by the accumulating fluid.
- Loss of Appetite: Many people with ascites may lose their appetite, which can contribute to unintentional weight loss.
- Swelling in the Legs and Ankles: In some cases, the excess fluid in the abdomen can lead to peripheral edema, causing swelling in the legs and ankles.
- Fatigue: Ascites and its underlying causes, such as liver disease or heart failure, can lead to general fatigue and weakness.
- Frequent Urination: Some individuals may experience increased urination, especially during the night, as the body attempts to get rid of excess fluid through the kidneys.
- Hernias: The pressure from ascitic fluid can increase the risk of developing hernias, particularly umbilical hernias (around the belly button).
Diagnosis of Ascites:
Medical History and Physical Examination:
- The healthcare provider will start by taking a detailed medical history, including any known underlying conditions, recent symptoms, and relevant medications.
- A physical examination will be conducted to assess the extent of abdominal distension, check for tenderness, and identify any signs of underlying diseases.
Imaging Tests:
- Ultrasound: Ultrasonography is often the initial imaging test used to detect ascites. It can help visualize the accumulation of fluid in the abdominal cavity and assess its distribution.
- CT Scan (Computed Tomography): CT scans provide detailed cross-sectional images of the abdomen and can help identify the cause of ascites, such as liver disease or abdominal tumors.
- MRI (Magnetic Resonance Imaging): In some cases, MRI may be used to evaluate the extent and nature of ascites and any associated conditions.
Ascitic Fluid Analysis:
- If ascites is confirmed through imaging and physical examination, a sample of the ascitic fluid may be obtained for analysis.
- A procedure called paracentesis is commonly used to collect ascitic fluid. During paracentesis, a thin needle is inserted into the abdominal cavity, and a sample of the fluid is withdrawn for laboratory testing.
Ascitic fluid analysis can provide valuable information about the underlying cause of ascites. The analysis may include:
- Cell count and differential: To check for infection or cancer cells.
- Protein levels: To assess the serum-ascites albumin gradient (SAAG), which helps differentiate between causes of ascites.
- Culture and sensitivity testing: To identify any infections and determine the appropriate antibiotics if necessary.
- Cytology: To detect cancer cells, especially in cases where malignancy is suspected.
Laboratory Tests:
- Blood tests may be performed to assess liver function, kidney function, and other relevant parameters. These tests can help identify underlying conditions contributing to ascites.
- Additional Diagnostic Procedures: Depending on the suspected cause of ascites, additional tests or procedures may be necessary. For example, a liver biopsy may be recommended if liver disease is suspected.
Treatment and Management:
Here are the main approaches to treating and managing ascites:
Treating the Underlying Cause:
- Ascites is often a symptom of an underlying medical condition. The most common cause is liver cirrhosis, but it can also result from heart failure, kidney disease, cancer, or other conditions.
- Treatment will focus on managing or curing the underlying condition. For example:
- In liver cirrhosis, treatment may involve lifestyle changes (e.g., alcohol cessation), medications to manage liver function, and, in some cases, liver transplantation.
- Heart failure may be managed with medications, lifestyle changes, and sometimes procedures like cardiac interventions.
- Cancer-related ascites may require cancer treatments such as chemotherapy, radiation therapy, or surgery.
Dietary Sodium Restriction:
- Reducing dietary sodium (salt) intake is essential in managing ascites because salt can cause the body to retain fluids. Patients are often advised to follow a low-sodium diet to minimize fluid retention.
Diuretic Medications:
- Diuretic drugs, such as spironolactone and furosemide, may be prescribed to help the body eliminate excess fluid. These medications increase urine production and reduce fluid buildup in the body.
- Diuretics should be used carefully and under medical supervision to avoid electrolyte imbalances and kidney problems.
- Paracentesis (Fluid Removal): Paracentesis is a procedure in which a needle is inserted into the abdominal cavity to remove excess ascitic fluid. This can provide immediate relief from discomfort and improve breathing.
Paracentesis may be performed regularly in cases of recurrent or refractory ascites. - Albumin Replacement: After paracentesis, especially large-volume paracentesis, albumin may be administered intravenously to help maintain blood volume and prevent complications.
- Transjugular Intrahepatic Portosystemic Shunt (TIPS): TIPS is a procedure that creates a shunt (passageway) within the liver to reduce portal hypertension and improve ascites. It is typically considered for patients with advanced liver disease.
- Antibiotics (for Infection): If ascites is complicated by infection (spontaneous bacterial peritonitis or SBP), antibiotics are administered to treat the infection.
- Lifestyle Modifications: Patients with ascites should be encouraged to make lifestyle changes, such as limiting alcohol intake and maintaining a healthy diet, to prevent exacerbation of the underlying condition.
- Monitoring and Follow-Up: Regular medical follow-up is essential to monitor the effectiveness of treatment, manage complications, and adjust medications as needed.
Surgical Interventions: In some cases, surgical procedures may be considered, such as a liver transplant for end-stage liver disease or surgery to remove tumors causing ascites.
Prevention of Ascites:
Here are some strategies and preventive measures for reducing the risk of developing ascites.
- Manage Liver Disease: If you have liver disease, such as hepatitis or cirrhosis, it’s crucial to follow your healthcare provider’s recommendations for managing the condition. This may include medications, lifestyle changes, and regular check-ups to monitor liver function.
- Limit Alcohol Consumption: If alcohol is a contributing factor to liver disease or other underlying conditions, reducing or eliminating alcohol consumption is essential to prevent further liver damage and the development of ascites.
- Maintain a Healthy Diet: A balanced and nutritious diet can help support liver health and overall well-being. It’s important to follow a low-sodium diet to minimize fluid retention if you have ascites or are at risk of developing it.
- Manage Heart Health: If you have heart disease or heart failure, follow your healthcare provider’s recommendations for managing the condition. This may involve medications, dietary changes, exercise, and regular monitoring.
- Control Blood Pressure: High blood pressure can contribute to the development of ascites. Taking steps to control blood pressure through medication, lifestyle modifications, and regular check-ups is important.
- Maintain Kidney Health: Regular check-ups and monitoring of kidney function can help prevent kidney disease, which is a potential cause of ascites. Managing conditions like diabetes and hypertension can also reduce the risk of kidney disease.
- Practice Safe Sex: Hepatitis B and C are common causes of liver disease, which can lead to ascites. Practicing safe sex and avoiding sharing needles or other drug paraphernalia can reduce the risk of contracting these viruses.
- Vaccinations: Vaccinations for hepatitis A and B are available and can help prevent infection with these viruses, which can cause liver damage.
- Seek Early Medical Attention: If you experience symptoms or risk factors associated with liver disease, heart disease, or kidney disease, seek prompt medical attention. Early diagnosis and treatment can prevent or slow the progression of these conditions.
- Medication Management: If you are prescribed medications that have the potential to cause liver damage or kidney problems, take them as directed and discuss any concerns or side effects with your healthcare provider.
- Regular Check-Ups: Even if you feel well, it’s important to have regular check-ups with your healthcare provider, especially if you have underlying conditions that increase the risk of ascites. Early detection and management of any developing issues can be crucial.
- Lifestyle Changes: Adopting a healthy lifestyle that includes regular exercise, maintaining a healthy weight, and avoiding smoking can have a positive impact on overall health and may reduce the risk of certain underlying conditions that lead to ascites.
Complications of Ascites:
Some of the potential complications associated with ascites include.
- Spontaneous Bacterial Peritonitis (SBP): Ascitic fluid provides an environment conducive to bacterial growth. In SBP, bacteria enter the ascitic fluid without an obvious source of infection, leading to abdominal pain, fever, and other signs of infection. SBP can be life-threatening and requires immediate medical attention.
- Kidney Dysfunction (Hepatorenal Syndrome): Ascites can put pressure on the kidneys and reduce blood flow to these organs, potentially leading to kidney dysfunction or hepatorenal syndrome. This condition results in impaired kidney function and can be serious, especially in individuals with advanced liver disease.
- Hyponatremia: Diuretic use in the treatment of ascites can lead to electrolyte imbalances, including low sodium levels (hyponatremia). Severe hyponatremia can cause confusion, seizures, and other neurological symptoms.
- Abdominal Hernias: The increased abdominal pressure from ascites can weaken the abdominal muscles and lead to the development of hernias, such as umbilical hernias or inguinal hernias.
- Respiratory Complications: Severe ascites can cause compression of the diaphragm and reduce lung expansion, leading to difficulty breathing, particularly when lying flat (orthopnea). This can result in reduced oxygen levels and respiratory distress.
- Malnutrition: Ascites can be associated with malnutrition due to decreased appetite, impaired nutrient absorption, and altered metabolism. Malnutrition can further weaken the individual’s overall health.
- Circulatory Problems: Ascites can lead to changes in blood circulation, potentially causing varices (enlarged veins) in the esophagus and stomach. These varices are prone to bleeding, which can be life-threatening.
- Reduced Quality of Life: The discomfort and limitations imposed by ascites can significantly reduce an individual’s quality of life, affecting their ability to perform daily activities and enjoy a normal lifestyle.
- Risk of Infection: The presence of ascites can increase the risk of skin infections, particularly in areas where the abdominal skin is stretched and compromised.
- Psychological Distress: The physical and emotional impact of ascites can lead to psychological distress, including depression and anxiety.
Prognosis:
Here are some key factors that influence the prognosis for individuals with ascites.
- Underlying Cause: The underlying medical condition responsible for ascites plays a significant role in determining the prognosis. For example, if the cause is reversible and can be effectively treated (e.g., treating an infection, stopping alcohol consumption, or managing heart failure), the prognosis may be favorable. However, if the cause is advanced and not easily treatable (e.g., end-stage liver cirrhosis), the prognosis may be less favorable.
- Timely Diagnosis: Early diagnosis and intervention are crucial for improving the prognosis. Identifying ascites and its underlying cause at an early stage can lead to more effective treatment and better outcomes.
- Treatment and Management: The success of treatment and management strategies is a critical factor in the prognosis. Proper management of the underlying condition, such as liver disease or heart failure, can help control ascites and prevent complications. Regular follow-up care and adherence to treatment plans are essential.
- Complications: The development of complications, such as spontaneous bacterial peritonitis (SBP), hepatorenal syndrome, hyponatremia, or variceal bleeding, can significantly worsen the prognosis. Prompt recognition and treatment of these complications are essential for better outcomes.
- Patient’s Overall Health: The patient’s general health, including the presence of other medical conditions or comorbidities, can influence the prognosis. Patients with good overall health may have a better prognosis and be better able to tolerate treatments and interventions.
- Response to Treatment: The individual response to diuretic medications, paracentesis, and other therapeutic interventions can affect the prognosis. Some individuals may respond well to treatment and experience a reduction in ascites, while others may have persistent or recurrent fluid buildup.
- Liver Transplantation: In cases where ascites is primarily due to end-stage liver disease, liver transplantation may offer a chance for a cure and improved long-term prognosis.
- Lifestyle Factors: Lifestyle changes, such as alcohol cessation, following a low-sodium diet, and maintaining a healthy lifestyle, can positively impact the prognosis by preventing the progression of underlying conditions.
FAQs:
What is ascites?
Ascites is a medical condition characterized by the abnormal accumulation of fluid in the abdominal cavity, leading to abdominal swelling and discomfort.
What are the common causes of ascites?
The most common cause of ascites is liver cirrhosis. Other causes include heart failure, kidney disease, cancer, infections, and more.
What are the symptoms of ascites?
Common symptoms include abdominal swelling, weight gain, difficulty breathing, abdominal discomfort or pain, nausea, and fatigue.
How is ascites diagnosed?
Diagnosis involves physical examination, medical history review, imaging tests (e.g., ultrasound, CT scan), and analysis of ascitic fluid obtained through paracentesis.
What is the treatment for ascites?
Treatment aims to manage the underlying cause and may include dietary sodium restriction, diuretic medications, paracentesis (fluid removal), and addressing complications.
What are the complications of ascites?
Complications can include spontaneous bacterial peritonitis (SBP), kidney dysfunction, hyponatremia, hernias, respiratory problems, and more.
Can ascites be prevented?
Prevention often involves managing underlying conditions (e.g., liver disease, heart disease), limiting alcohol consumption, following a low-sodium diet, and maintaining a healthy lifestyle.
What is the prognosis for ascites?
Prognosis varies based on the underlying cause, the effectiveness of treatment, the presence of complications, and the patient’s overall health. Early diagnosis and treatment can improve outcomes.
Is ascites a disease itself?
No, ascites is not a disease but a symptom of an underlying medical condition. It indicates a problem within the body, often related to the liver, heart, or kidneys.
When should I seek medical attention for ascites?
If you experience symptoms of ascites, such as abdominal swelling, it’s essential to seek medical attention promptly. Ascites is usually a sign of an underlying medical problem that requires evaluation and treatment.
Conclusion:
In conclusion, ascites is a medical condition characterized by the accumulation of excess fluid in the abdominal cavity, typically signaling an underlying health issue such as liver disease, heart failure, or kidney dysfunction. Early diagnosis and appropriate management are crucial in addressing both the ascites itself and its root cause. With timely medical attention, effective treatment, lifestyle modifications, and close monitoring, individuals can improve their prognosis, alleviate symptoms, and enhance their overall quality of life. Ascites underscores the importance of regular medical check-ups and proactive health measures to prevent and address underlying conditions that may lead to this challenging symptom.
Possible References Used