Discover the Enzyme Multiplied Immunoassay Technique (EMIT) used in clinical laboratories for accurate measurement of drugs, hormones, and other analytes. Learn about its principles, procedure, quality control, and safety precautions to ensure reliable results.

Methodology for Enzyme Multiplied Immunoassay Technique (EMIT) in Clinical Laboratory
Introduction
- Enzyme Multiplied Immunoassay Technique (EMIT) is a type of enzyme-linked immunoassay used for the quantitative measurement of substances such as drugs, hormones, and other analytes in biological fluids. It is widely used in clinical laboratories for therapeutic drug monitoring, drug abuse testing, and hormone level assessment.
Principle
- EMIT is based on competitive binding between an analyte in the sample and a labeled analyte (or hapten) for a limited number of antibody binding sites. The enzyme label on the analyte or hapten catalyzes a reaction that produces a detectable signal. The amount of signal is inversely proportional to the concentration of the analyte in the sample.
Specimen Requirements
- Type of specimen: Blood, serum, plasma, urine, or other biological fluids
- Volume of specimen required: Typically 1-5 mL
- Collection method: Standard clinical procedures for sample collection (e.g., venipuncture, urine collection)
- Handling and storage requirements: Store samples at 4°C for short-term storage or -20°C for long-term storage. Avoid repeated freeze-thaw cycles.
- Stability of the specimen: Analytes in biological fluids are generally stable if stored properly; specific stability details may vary for different analytes.
Reagents and Materials
- Antibody: Specific to the analyte of interest
- Enzyme-labeled analyte or hapten: Commonly used enzymes include horseradish peroxidase (HRP) or alkaline phosphatase (ALP)
- Substrate: For the enzyme, producing a measurable signal (e.g., tetramethylbenzidine for HRP)
- Buffer solutions: For maintaining pH and ionic strength during the assay
- Standards and controls: Known concentrations of the analyte for calibration and quality control
Equipment
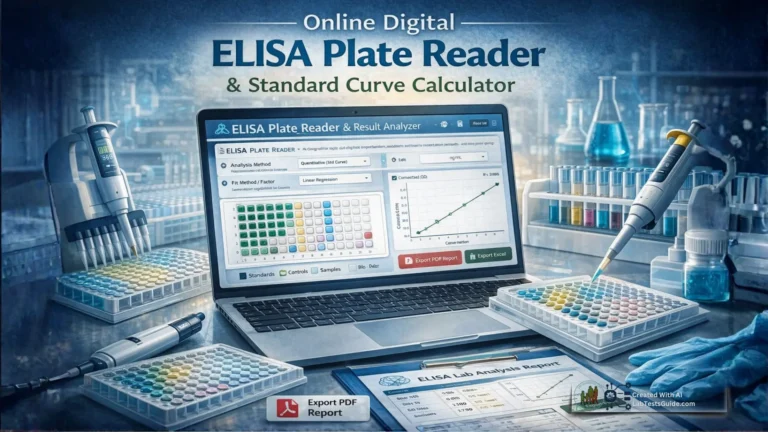
- Microplate reader: For measuring absorbance or fluorescence
- Micropipettes and tips: For accurate liquid handling
- Microplates: Typically 96-well plates
- Incubator: For maintaining the assay temperature
- Shaker: For mixing samples and reagents
Procedure
Preparation:
- Sample Preparation: Centrifuge blood samples to obtain serum or plasma. Filter or dilute urine samples if necessary.
- Reagent Preparation: Prepare enzyme-labeled analyte, antibodies, and substrate solutions according to the manufacturer’s instructions.
Assay Steps:
- Coat the Plate: Add the specific antibody to the wells of a microplate and incubate to allow binding. Wash to remove unbound antibody.
- Add Sample and Standards: Add samples, calibration standards, and controls to the wells. Include a range of concentrations to generate a standard curve.
- Add Enzyme-Labeled Analyte: Introduce the enzyme-labeled analyte or hapten to the wells. The enzyme-labeled analyte competes with the analyte in the sample for antibody binding sites.
- Incubation: Allow sufficient time for binding to occur. Incubate at the temperature specified by the assay protocol.
- Wash: Wash the wells to remove unbound components, leaving only the bound enzyme-labeled analyte.
- Add Substrate: Add the substrate solution to the wells. The enzyme catalyzes the conversion of the substrate to a detectable product, usually a color change.
- Stop Reaction: Add a stop solution if required to halt the enzyme reaction.
- Read Results: Measure the absorbance or fluorescence of each well using a microplate reader. The signal is inversely proportional to the concentration of the analyte in the sample.
Quality Control
- Calibration: Regularly calibrate the microplate reader and verify the accuracy of the assay using known standards.
- Controls: Run positive and negative controls to ensure the assay is functioning correctly.
- Reagent Quality: Use fresh reagents and check for any signs of contamination or degradation.
- Plate Washing: Ensure that washing steps are performed consistently to avoid cross-contamination and ensure accurate results.
Calculation and Interpretation
- Generate a Standard Curve: Plot the signal (e.g., absorbance) versus the known concentrations of the analyte to create a standard curve.
- Determine Analyte Concentration: Compare the signal from the samples to the standard curve to determine the concentration of the analyte.
- Report Results: Present the concentration of the analyte in the samples, including any necessary units and reference ranges.
Limitations
- Cross-Reactivity: The assay may show cross-reactivity with similar substances, leading to false results.
- Sensitivity and Specificity: EMIT may have limitations in detecting very low concentrations or distinguishing between similar analytes.
- Matrix Effects: Components in the biological matrix can interfere with the assay, requiring careful sample preparation and validation.
Safety Precautions
- PPE: Use appropriate PPE (gloves, lab coat, safety goggles) when handling samples and reagents.
- Chemical Handling: Follow safety guidelines for handling enzyme substrates and stop solutions.
- Waste Disposal: Dispose of waste according to local regulations and institutional guidelines.
References
- Glick, B. R. (2008). Methods of Enzymatic Analysis (3rd ed.). Wiley-VCH.
- Clinical Immunology: Principles and Practice by Robert R. Rich and David T. Rowe.
- Manufacturer’s guidelines for EMIT reagents and equipment.
- Clinical guidelines and standards from institutions such as the American Association for Clinical Chemistry (AACC) and the Clinical and Laboratory Standards Institute (CLSI).