Endospore Staining 50 FAQs and 30 MCQ
Master bacterial endospore staining with our ultimate resource featuring:
📚 50 Key FAQs Covering:
✓ Principles: Why endospores resist staining
✓ Protocols: Schaeffer-Fulton vs. Dorner methods
✓ Troubleshooting: Fixation errors, over-decolorization
✓ Clinical Relevance: Identifying Bacillus & Clostridium
✓ Safety: Handling spore-forming pathogens
✍️ 30 Practice MCQs On:
◼️ Stain composition (malachite green/safranin)
◼️ Optimal steaming durations
◼️ Diagnostic patterns in anthrax/gangrene
◼️ Differentiation from capsule staining
🎯 Perfect For:
• Microbiology students
• MLT/MLS certification prep
• USMLE/PLAB exam candidates
Includes detailed explanations for all answers!

Endospore Staining 50 FAQs
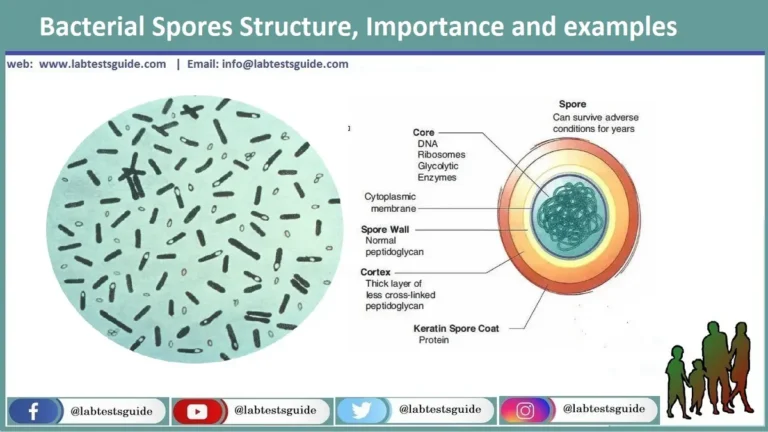
What is an endospore?
A dormant, tough, non-reproductive structure formed by some bacteria to survive harsh conditions.
Which bacterial families produce endospores?
Primarily Firmicutes, including Bacillus and Clostridium species.
Why are endospores resistant to staining?
Due to their tough outer protein and peptidoglycan layers, which resist dye penetration.
What environmental conditions trigger endospore formation?
Lack of nutrients, extreme temperatures, desiccation, and exposure to chemicals/radiation.
Are endospores reproductive structures?
No, they are survival structures, not for reproduction.
Name two pathogenic endospore-forming bacteria.
Bacillus anthracis (anthrax) and Clostridium botulinum (botulism).
How long can endospores survive in harsh conditions?
Years to decades, depending on the species and environment.
Can endospores be killed by normal sterilization methods?
They are highly resistant but can be destroyed by autoclaving (121°C, 15 psi).
What is the difference between a vegetative cell and an endospore?
Vegetative cells are metabolically active, while endospores are dormant and resistant.
Do all bacteria produce endospores?
No, only certain Gram-positive bacteria (e.g., Bacillus, Clostridium).
What is the purpose of endospore staining?
To detect, identify, and differentiate endospores from vegetative cells.
Why is heat used in endospore staining?
Heat helps the dye penetrate the tough spore coat.
What is the primary stain in the Schaeffer-Fulton method?
Malachite green.
What is the counterstain in the Schaeffer-Fulton method?
Safranin.
Why is water used as a decolorizer in Schaeffer-Fulton staining?
It washes away malachite green from vegetative cells but not from spores.
What color do endospores appear after Schaeffer-Fulton staining?
Green (from malachite green).
What color do vegetative cells appear after Schaeffer-Fulton staining?
Pink/red (from safranin).
What is the primary stain in Dorner’s method?
Carbolfuchsin.
What is the counterstain in Dorner’s method?
Nigrosin.
How does Dorner’s method differ from Schaeffer-Fulton?
Dorner uses carbolfuchsin + nigrosin, while Schaeffer-Fulton uses malachite green + safranin.
What color do endospores appear in Dorner’s method?
Red (from carbolfuchsin).
What color is the background in Dorner’s method?
Black (from nigrosin).
What is the decolorizer in Dorner’s method?
Acid-alcohol.
Which staining method is more commonly used in labs?
Schaeffer-Fulton (simpler and faster).
Can Gram staining detect endospores?
Yes, but they appear as clear, unstained areas inside Gram-positive cells.
What is the first step in preparing a slide for endospore staining?
Heat fixation to adhere bacteria to the slide.
Why is blotting paper used in staining?
To hold the dye and allow even heating.
How long should malachite green be steamed in Schaeffer-Fulton staining?
3-5 minutes.
What happens if you skip steaming in endospore staining?
The dye won’t penetrate the spore, leading to false negatives.
Why is safranin used after malachite green?
To stain vegetative cells for contrast.
What magnification is used to view endospores?
1000X (oil immersion).
What does a mature free endospore look like under the microscope?
A green (or red) oval not attached to any cell.
What does a vegetative cell with an endospore look like?
A pink cell with a green oval inside.
What happens if you over-decolorize in Schaeffer-Fulton staining?
Both spores and vegetative cells may lose color.
Can phase-contrast microscopy detect endospores without staining?
Yes, they appear as refractile bodies.
Why is endospore staining clinically important?
Helps diagnose infections caused by Bacillus or Clostridium.
What diseases are caused by endospore-forming bacteria?
Tetanus (C. tetani), botulism (C. botulinum), anthrax (B. anthracis).
Can endospore staining identify non-spore-forming bacteria?
No, it’s specific for spore-formers.
What is a disadvantage of endospore staining?
Only useful for specific bacteria (not all microbes).
How does endospore staining compare to Gram staining?
Gram staining differentiates Gram+ vs. Gram–, while endospore staining targets spores vs.
What is the Klein method of endospore staining?
Uses methylene blue instead of malachite green.
What is the role of acid-alcohol in Dorner’s method?
Decolorizes vegetative cells but not spores.
Can endospores survive boiling?
Yes, some can survive 100°C for hours.
What is the modified Ziehl-Neelsen method for endospores?
Uses carbolfuchsin + sulfuric acid + methylene blue.
How does the Moeller stain differ from Schaeffer-Fulton?
Uses carbolfuchsin + methylene blue.
What is the Abbott method for endospore staining?
Uses methylene blue + aniline fuchsin.
Why is nigrosin used in Dorner’s method?
Provides a black background for better contrast.
Can endospores be seen in a simple wet mount?
Yes, but staining improves visibility.
What is the best way to destroy endospores in lab settings?
Autoclaving (121°C, 15-20 min).
Why is malachite green used despite being toxic?
It binds strongly to spores and resists washing.
Endospore Staining 30 MCQ
- What is an endospore?
a) A reproductive structure of bacteria
b) A dormant, resistant form of some bacteria
c) A type of fungal spore
d) A viral inclusion body - Which bacterial genera commonly produce endospores?
a) Escherichia and Salmonella
b) Bacillus and Clostridium
c) Staphylococcus and Streptococcus
d) Mycobacterium and Pseudomonas - Endospores are formed in response to:
a) Abundant nutrients
b) Favorable temperatures
c) Harsh environmental conditions
d) High oxygen levels - The primary function of an endospore is:
a) Reproduction
b) Photosynthesis
c) Survival in adverse conditions
d) Motility - Which of the following is NOT a characteristic of endospores?
a) Heat resistance
b) Resistance to chemicals
c) Rapid metabolic activity
d) Dormancy
- Why is endospore staining considered a differential stain?
a) It uses multiple dyes
b) It distinguishes spores from vegetative cells
c) It only works on Gram-positive bacteria
d) It requires acid-fast techniques - The primary stain in the Schaeffer-Fulton method is:
a) Safranin
b) Crystal violet
c) Malachite green
d) Carbolfuchsin - Heat is used in endospore staining to:
a) Kill the bacteria
b) Help the dye penetrate the spore coat
c) Decolorize vegetative cells
d) Fix the smear - In Schaeffer-Fulton staining, vegetative cells appear:
a) Green
b) Pink/red
c) Blue
d) Colorless - The decolorizer in the Schaeffer-Fulton method is:
a) Acid-alcohol
b) Water
c) Ethanol
d) Iodine
- Which method uses carbolfuchsin as the primary stain?
a) Schaeffer-Fulton
b) Gram staining
c) Dorner’s method
d) Acid-fast staining - In Dorner’s method, the counterstain is:
a) Safranin
b) Nigrosin
c) Methylene blue
d) Malachite green - The background in Dorner’s method appears:
a) Green
b) Red
c) Black
d) Blue - Which staining method is most commonly used in labs?
a) Dorner’s method
b) Schaeffer-Fulton
c) Ziehl-Neelsen
d) Klein method - The mordant in endospore staining is:
a) Iodine
b) Heat
c) Alcohol
d) Acid
- Endospores appear _____ under the microscope after Schaeffer-Fulton staining.
a) Pink
b) Green
c) Blue
d) Purple - Vegetative cells appear _____ after Schaeffer-Fulton staining.
a) Green
b) Pink/red
c) Colorless
d) Blue - The best magnification to view endospores is:
a) 40X
b) 100X
c) 400X
d) 1000X (oil immersion) - A mature, free endospore appears as:
a) A green oval not attached to a cell
b) A pink rod-shaped cell
c) A purple cluster
d) A blue spiral - If malachite green is not properly steamed, what happens?
a) Spores will not stain
b) Vegetative cells will turn green
c) The slide will over-decolorize
d) Safranin will not work
- Which pathogen causes tetanus and forms endospores?
a) Bacillus anthracis
b) Clostridium tetani
c) Escherichia coli
d) Staphylococcus aureus - Endospore staining helps diagnose infections caused by:
a) Mycobacterium tuberculosis
b) Bacillus and Clostridium
c) Streptococcus pyogenes
d) Neisseria gonorrhoeae - Which sterilization method effectively kills endospores?
a) Boiling at 100°C
b) UV light
c) Autoclaving (121°C, 15 psi)
d) Ethanol disinfection - A patient with food poisoning may have ingested:
a) Bacillus cereus endospores
b) Mycobacterium leprae
c) Vibrio cholerae
d) Treponema pallidum - Endospores are NOT found in:
a) Soil
b) Dust
c) Sterilized surgical tools
d) Freshly boiled water
- The Klein method uses which dye instead of malachite green?
a) Safranin
b) Methylene blue
c) Carbolfuchsin
d) Nigrosin - Which method uses acid-alcohol as a decolorizer?
a) Schaeffer-Fulton
b) Dorner’s method
c) Gram staining
d) Capsule staining - Phase-contrast microscopy can detect endospores because they appear:
a) Fluorescent
b) Refractile (glowing)
c) Dark blue
d) Red - Why is malachite green used despite being toxic?
a) It binds permanently to spores
b) It is cheaper than other dyes
c) It stains Gram-negative bacteria
d) It works without heat - The Abbott method uses:
a) Methylene blue + aniline fuchsin
b) Malachite green + safranin
c) Carbolfuchsin + nigrosin
d) Crystal violet + iodine
🔑 Keywords to Target:
- “How to stain anthrax spores”
- “Endospore vs acid-fast staining differences”
- “Best stain for Clostridium identification”
- “Schaeffer-Fulton method step-by-step”