A diuretic is a type of medication or substance that promotes diuresis, which is the increased production of urine by the kidneys. Diuretics are commonly used to manage conditions such as high blood pressure (hypertension), heart failure, and certain kidney disorders. They work by increasing the excretion of sodium and water from the body, which helps reduce the overall fluid volume and subsequently lower blood pressure.
What Are Diuretics?
Diuretics are a class of medications or substances that promote diuresis, which is the increased production of urine by the kidneys. They are commonly used in medical practice to manage various conditions, primarily those related to fluid retention and high blood pressure. Diuretics work by affecting the kidney’s ability to reabsorb certain substances, leading to increased urine output. This process can help reduce the overall volume of fluid in the body and lower blood pressure.
How Do Diuretics Work?
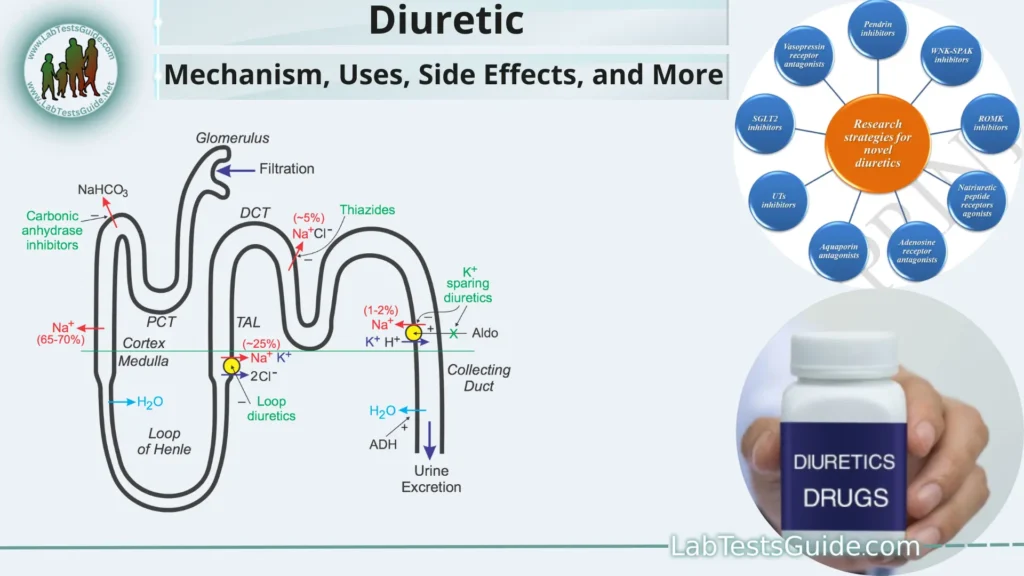
- Nephron and Kidney Function: The basic functional unit of the kidney is called the nephron. Nephrons consist of various structures, including the glomerulus, proximal tubule, loop of Henle, distal tubule, and collecting duct. Each of these segments plays a role in filtering and processing blood to produce urine.
- Sodium Reabsorption: In the proximal tubule, a significant portion of filtered sodium is reabsorbed back into the bloodstream. This sodium reabsorption creates an osmotic gradient that promotes the reabsorption of water, effectively conserving water in the body.
Diuretic Actions:
- Thiazide Diuretics: These diuretics act on the early part of the distal convoluted tubule. They inhibit the reabsorption of sodium and chloride ions, reducing the osmotic gradient and subsequently decreasing water reabsorption. This leads to increased urine production.
- Loop Diuretics: These diuretics work in the loop of Henle, particularly the thick ascending limb. They inhibit the reabsorption of sodium, potassium, and chloride ions. Loop diuretics are potent and can cause significant fluid and electrolyte loss, making them useful for managing conditions like congestive heart failure and edema.
- Potassium-Sparing Diuretics: These diuretics target the distal convoluted tubule and collecting ducts. They reduce sodium reabsorption while preserving potassium retention. This helps to promote diuresis without causing excessive potassium loss.
- Osmotic Diuretics: These substances are filtered at the glomerulus but are not reabsorbed in the tubules. They create an osmotic gradient that prevents water reabsorption, leading to increased urine production. Osmotic diuretics are often used in emergency situations or to reduce intracranial pressure.
- Effects on Electrolytes: The use of diuretics can lead to changes in electrolyte balance, particularly sodium and potassium levels. Loop and thiazide diuretics can result in loss of both sodium and potassium, which may require additional monitoring or supplementation.
- Clinical Applications: Diuretics are commonly used to treat conditions such as hypertension, congestive heart failure, edema, and certain kidney disorders. They help reduce blood volume and fluid accumulation in various body tissues.
Types of Diuretics:
Here are the main types of diuretics.
Thiazide Diuretics:
- Examples: Hydrochlorothiazide, Chlorthalidone
- Mechanism: Thiazide diuretics work by inhibiting the reabsorption of sodium and chloride in the early part of the distal convoluted tubule in the kidneys. This reduces the osmotic gradient for water reabsorption, leading to increased urine output.
- Clinical Use: Thiazide diuretics are commonly prescribed for hypertension management and mild fluid retention. They are often part of the first-line treatment for hypertension.
Loop Diuretics:
Examples: Furosemide, Bumetanide, Torsemide
Mechanism: Loop diuretics act on the thick ascending limb of the loop of Henle. They inhibit the reabsorption of sodium, potassium, and chloride ions, preventing the establishment of an osmotic gradient that promotes water reabsorption. This results in significant diuresis.
Clinical Use: Loop diuretics are potent diuretics used for severe edema (e.g., congestive heart failure, pulmonary edema) and conditions requiring rapid reduction of fluid volume.
Potassium-Sparing Diuretics:
- Examples: Spironolactone, Eplerenone, Amiloride, Triamterene
- Mechanism: Potassium-sparing diuretics work in the distal convoluted tubule and collecting ducts. They either block aldosterone (a hormone that promotes sodium and water retention) or directly inhibit sodium channels. This leads to increased sodium excretion while preserving potassium levels.
- Clinical Use: Potassium-sparing diuretics are used to counteract excessive potassium loss seen with other diuretics. They are often prescribed to patients at risk of low potassium levels (hypokalemia) or as part of combination therapy.
Osmotic Diuretics:
- Example: Mannitol
- Mechanism: Osmotic diuretics are not reabsorbed in the kidney tubules. They create an osmotic force that prevents water reabsorption, resulting in increased urine production. Osmotic diuretics also decrease intracranial pressure and intraocular pressure in certain medical situations.
- Clinical Use: Osmotic diuretics are used in emergencies to reduce brain swelling (cerebral edema), manage acute kidney injury, and lower intraocular pressure in conditions like glaucoma.
Mechanism of Action:
Thiazide Diuretics:
- Mechanism: Thiazide diuretics inhibit the sodium-chloride symporter (NCC) in the early part of the distal convoluted tubule. This reduces the reabsorption of sodium and chloride ions, disrupting the establishment of an osmotic gradient for water reabsorption.
- Result: Increased excretion of sodium and water in the urine, leading to diuresis and reduction in blood volume and pressure.
Loop Diuretics:
- Mechanism: Loop diuretics block the sodium-potassium-chloride cotransporter (NKCC2) in the thick ascending limb of the loop of Henle. By inhibiting the reabsorption of sodium, potassium, and chloride ions, loop diuretics prevent the establishment of the medullary osmotic gradient, reducing water reabsorption.
- Result: Significant increase in urine output, leading to rapid diuresis, fluid volume reduction, and blood pressure decrease.
Potassium-Sparing Diuretics:
- Mechanism: Potassium-sparing diuretics act on different parts of the distal tubule and collecting ducts. Some block the aldosterone receptor (spironolactone, eplerenone), reducing sodium reabsorption and potassium secretion. Others (amiloride, triamterene) directly block sodium channels, decreasing sodium reabsorption.
- Result: Moderate increase in urine output with minimal potassium loss. They are often used to counteract potassium loss caused by other diuretics.
Osmotic Diuretics:
- Mechanism: Osmotic diuretics are filtered at the glomerulus but are not reabsorbed in the tubules. They create an osmotic force in the renal tubules, preventing water reabsorption by maintaining a higher solute concentration in the tubular fluid.
- Result: Increased urine production and diuresis, reduction of intracranial or intraocular pressure (in certain situations), and promotion of fluid removal in cases of acute kidney injury.
Clinical Applications:
Here are the main clinical applications of diuretics.
- Hypertension (High Blood Pressure): Thiazide diuretics are often used as first-line treatment for hypertension. By reducing blood volume and cardiac output through increased urine output, they help lower blood pressure.
- Congestive Heart Failure (CHF): Loop diuretics are frequently prescribed to manage fluid retention in individuals with congestive heart failure. They reduce edema and fluid buildup in the lungs and extremities, improving breathing and overall cardiovascular function.
- Edema: Diuretics, especially loop diuretics, are effective in treating edema caused by conditions such as heart failure, liver cirrhosis, and kidney disorders. They help remove excess fluid and reduce swelling.
- Nephrotic Syndrome: Nephrotic syndrome is characterized by significant proteinuria (protein loss in urine) and edema. Diuretics can help manage the fluid retention and edema associated with this condition.
- Kidney Disorders: Diuretics can be used in certain kidney disorders to manage fluid and electrolyte imbalances. Loop diuretics are sometimes used to increase urine output in acute kidney injury, while thiazide diuretics may be used to treat specific types of kidney stones.
- Liver Cirrhosis: Liver cirrhosis often leads to fluid accumulation in the abdomen (ascites) and legs (peripheral edema). Diuretics can help manage these symptoms by promoting fluid excretion.
- Intracranial Pressure (ICP) Management: Osmotic diuretics like mannitol are used to reduce intracranial pressure in conditions such as traumatic brain injury, cerebral edema, and brain tumors. They decrease cerebral fluid volume and lower pressure within the skull.
- Glaucoma: Osmotic diuretics like mannitol can reduce intraocular pressure in cases of acute glaucoma or when rapid reduction of pressure is needed.
- Hypercalcemia: Loop diuretics can be used in combination with other treatments to promote the excretion of excess calcium in hypercalcemia.
Prescription and Usage:
Here are some important points to keep in mind when it comes to the prescription and usage of diuretics.
Medical Evaluation:
- Diuretics should be prescribed by a qualified healthcare professional, such as a doctor or a specialist. They will assess the patient’s medical history, current health status, and any existing conditions that might affect the choice of diuretic.
Type of Diuretic:
- The choice of diuretic depends on the specific medical condition being treated. Thiazide diuretics are commonly used for hypertension, while loop diuretics are preferred for edema associated with congestive heart failure and kidney disorders.
Dosage and Administration:
- The dosage of diuretics can vary widely based on the individual patient and the severity of the condition. Dosages should be tailored to achieve the desired therapeutic effect without causing excessive fluid and electrolyte imbalances.
- Diuretics are typically taken orally in the form of tablets or capsules. Dosages may be taken once daily or divided into multiple doses.
- Monitoring and Follow-Up: Regular medical follow-up appointments are essential when using diuretics. Healthcare professionals will monitor the patient’s fluid and electrolyte balance, blood pressure, kidney function, and overall response to treatment.
- Potassium-Sparing Diuretics: If prescribed potassium-sparing diuretics, healthcare professionals may monitor potassium levels more closely due to their potential to increase potassium retention.
- Combination Therapy: Diuretics may be prescribed alone or in combination with other medications, such as antihypertensives or medications for heart conditions. Combining diuretics with other drugs requires careful consideration of potential interactions and cumulative effects on fluid and electrolyte balance.
- Dietary Considerations: Patients using diuretics should be advised about dietary considerations, including the potential for potassium loss (especially with loop and thiazide diuretics). Eating foods rich in potassium, such as bananas, oranges, and leafy greens, can help counteract this effect.
- Fluid Intake: Patients are generally advised to maintain adequate fluid intake, as diuretics can lead to increased urine output and potential dehydration.
- Avoiding Abrupt Changes: Abruptly stopping diuretics can lead to rapid fluid retention and increased blood pressure. If discontinuation is necessary, it should be done under medical supervision.
- Special Populations: Dosages and usage of diuretics might need to be adjusted for pregnant women, older adults, children, and individuals with certain medical conditions (e.g., kidney disease, diabetes). Consultation with a healthcare provider is essential.
Monitoring and Side Effects:
Monitoring:
- Fluid and Electrolyte Levels: Regular monitoring of electrolyte levels, including sodium, potassium, and chloride, is important. Imbalances can lead to adverse effects such as muscle cramps, weakness, and heart rhythm disturbances.
Blood tests can help assess kidney function and electrolyte balance. Adjustments to the diuretic dosage may be needed based on these results. - Blood Pressure: Monitoring blood pressure is crucial, especially for individuals using diuretics to manage hypertension. Blood pressure should be regularly checked and adjusted as needed to achieve the target range.
- Kidney Function: Kidney function tests, such as serum creatinine and glomerular filtration rate (GFR), should be monitored to ensure that diuretics are not causing kidney impairment.
- Potassium Levels: For patients on loop diuretics or thiazide diuretics, monitoring potassium levels is particularly important. Low potassium levels (hypokalemia) can have serious health consequences.
Symptoms and Overall Well-being:
- Patients should report any unusual symptoms, such as excessive thirst, dry mouth, fatigue, irregular heartbeat, muscle cramps, or dizziness. These could indicate imbalances in fluid or electrolytes.
Common Side Effects:
- Dehydration: Increased urine output can lead to dehydration if fluid intake is insufficient.
Electrolyte Imbalances:
- Low sodium levels (hyponatremia) or low potassium levels (hypokalemia) can occur. Symptoms may include weakness, muscle cramps, irregular heartbeat, and more severe complications.
Dizziness and Lightheadedness: These can result from fluid and electrolyte imbalances. - Increased Urination: This is a common and expected side effect of diuretics.
Potassium-Sparing Diuretics:
These diuretics can cause hyperkalemia (high potassium levels) if not used carefully, leading to heart rhythm disturbances.
- Gout Flares: Diuretics can elevate uric acid levels, potentially triggering gout attacks in susceptible individuals.
- Impaired Kidney Function: Excessive diuresis without proper monitoring can strain the kidneys, especially in people with pre-existing kidney issues.
- Allergic Reactions: While rare, some individuals may experience allergic reactions to diuretics, such as skin rashes or difficulty breathing.
- Photosensitivity: Thiazide diuretics can increase sensitivity to sunlight, leading to sunburn more easily.
- Erectile Dysfunction: Some diuretics, especially thiazide diuretics, may contribute to erectile dysfunction in men.
Combination Therapy:
Hypertension Management:
- Diuretics are frequently used as part of combination therapy to manage hypertension. They are often combined with other antihypertensive medications such as beta-blockers, angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARBs), or calcium channel blockers.
- Combining diuretics with other antihypertensive agents can enhance blood pressure control through different mechanisms, resulting in improved overall management.
Heart Failure Treatment:
- Loop diuretics are commonly used in combination with other heart failure medications, such as ACE inhibitors or ARBs, beta-blockers, and aldosterone antagonists.
- Loop diuretics help alleviate fluid overload and congestion, while other medications target different aspects of heart function and remodeling.
Potassium-Sparing Diuretics and Thiazides:
- Sometimes, potassium-sparing diuretics (e.g., spironolactone) are used in combination with thiazide diuretics to counteract the potassium loss associated with thiazides.
- This combination can help prevent electrolyte imbalances while still achieving the diuretic effects needed for managing conditions like hypertension or heart failure.
Acute Edema Management:
- In cases of severe acute edema, such as pulmonary edema, a loop diuretic might be used in combination with other medications like oxygen therapy, vasodilators, and nitrates to rapidly relieve fluid buildup and improve oxygenation.
Individualized Approach:
- Combination therapy involving diuretics is tailored to the specific needs of the patient. The choice of medications and their dosages are determined based on the underlying medical condition, the patient’s health status, and any contraindications or potential interactions.
Regular Monitoring:
- When using combination therapy, close monitoring is essential. Healthcare professionals will assess the patient’s response to treatment, fluid and electrolyte balance, blood pressure, and any potential side effects.
Avoiding Duplication:
- Care should be taken to avoid duplication of effects. For example, combining two strong diuretics may lead to excessive fluid loss and electrolyte imbalances.
Communication and Education:
- Patients should be educated about the medications they are taking, their potential interactions, and the importance of adhering to the prescribed dosages and follow-up appointments.
Precautions and Contraindications:
Here are some precautions and contraindications to consider when using diuretics.
Precautions:
- Electrolyte Imbalances: Patients with a history of electrolyte imbalances, such as low potassium levels (hypokalemia) or high potassium levels (hyperkalemia), need close monitoring and may require adjustments to their diuretic therapy.
- Kidney Function: Diuretics affect kidney function, so individuals with impaired kidney function or chronic kidney disease should be monitored carefully. Dosages may need to be adjusted to prevent further kidney damage.
- Liver Dysfunction: Liver cirrhosis can lead to impaired metabolism of some diuretics. Special care is needed when prescribing diuretics to patients with liver disease.
- Gout: Diuretics, especially loop and thiazide diuretics, can increase uric acid levels, potentially triggering gout attacks in individuals prone to gout.
- Diabetes: Diuretics can affect blood glucose levels, particularly thiazide diuretics. Patients with diabetes should monitor their blood sugar levels closely and inform their healthcare provider.
- Pregnancy and Breastfeeding: Diuretics should be used cautiously during pregnancy and breastfeeding. Some diuretics, like thiazides, can affect fetal growth and electrolyte balance.
- Elderly Patients: Older adults are more susceptible to electrolyte imbalances and may require lower dosages of diuretics.
Contraindications:
- Allergy or Hypersensitivity: Patients with known allergies or hypersensitivity to specific diuretics should not use those medications.
- Severe Electrolyte Imbalances: Diuretics are contraindicated in patients with severe electrolyte imbalances, especially those with severe hypokalemia or hyperkalemia.
- Anuria: Anuria is the absence of urine production. Diuretics are contraindicated in individuals who are not producing urine, as their mechanism of action depends on existing urine production.
- Severe Renal Dysfunction: Patients with severe renal impairment may not tolerate diuretics well and may experience worsening kidney function.
- Severe Liver Dysfunction: Diuretics may be contraindicated in individuals with severe liver disease, as they could further stress liver function.
- Addison’s Disease: Potassium-sparing diuretics are generally contraindicated in individuals with Addison’s disease due to their potential to elevate potassium levels.
- Certain Medications: Certain medications, such as lithium, can interact adversely with diuretics. These interactions can lead to lithium toxicity or other serious effects.
Lifestyle and Dietary Considerations:
Here are some important considerations:
Fluid Intake:
- Adequate Hydration: While diuretics promote increased urine output, maintaining adequate hydration is crucial to prevent dehydration. Patients should be encouraged to drink enough fluids, especially water, to counterbalance the diuretic-induced fluid loss.
- Monitor Thirst: Patients should pay attention to their body’s signals for thirst and drink fluids accordingly.
Dietary Considerations:
- Sodium Intake: Diuretics often lead to sodium excretion, and reducing sodium intake can help maintain fluid balance. Patients should aim to limit their sodium intake by avoiding processed and high-sodium foods.
Potassium Intake:
- Loop and thiazide diuretics can lead to potassium loss. Consuming potassium-rich foods like bananas, oranges, spinach, and potatoes can help prevent potassium depletion.
- However, patients on potassium-sparing diuretics should be cautious with high-potassium foods to prevent hyperkalemia.
- Magnesium and Calcium Intake: Diuretics may also lead to magnesium and calcium loss. Patients should consume foods rich in these minerals, such as nuts, seeds, leafy greens, and dairy products.
- Alcohol and Caffeine: Both alcohol and caffeine can contribute to fluid loss and dehydration. Patients using diuretics should moderate their consumption of alcoholic and caffeinated beverages.
- Fluid-Rich Foods: Consuming foods with high water content, such as fruits and vegetables, can contribute to overall hydration.
- Balance and Moderation: A well-balanced diet that includes a variety of nutrient-rich foods is essential for supporting overall health and mitigating the effects of diuretics.
Supplements:
- Potassium Supplements: In consultation with a healthcare provider, patients might be advised to take potassium supplements to prevent hypokalemia, especially if using loop or thiazide diuretics.
- Other Minerals and Vitamins: Patients may also consider supplements for other essential minerals and vitamins that could be affected by diuretics. However, medical guidance is recommended before starting any new supplements.
Medication Timing:
- Loop Diuretics: Taking loop diuretics in the morning can help prevent excessive nighttime urination, which could interfere with sleep.
- Thiazide Diuretics: Taking thiazide diuretics earlier in the day can reduce the risk of frequent nighttime urination.
Avoid Self-Adjustment:
- Dosage Changes: Patients should never adjust their diuretic dosage without consulting their healthcare provider. Any changes to medication should be done under medical supervision.
Regular Monitoring:
- Electrolyte Levels: Regular monitoring of electrolyte levels is essential to detect and address imbalances promptly.
Communication:
- Healthcare Provider: Patients should maintain open communication with their healthcare provider about their dietary habits, lifestyle choices, and any concerns they have related to diuretic therapy.
FAQs:
What are diuretics used for?
Diuretics are medications that promote diuresis, which is increased urine production. They are used to manage conditions such as hypertension (high blood pressure), edema (fluid retention), heart failure, kidney disorders, and certain types of glaucoma.
How do diuretics work?
Diuretics work by affecting the kidney’s filtration and reabsorption processes, leading to increased urine production. They target different segments of the kidney’s tubular system and alter the reabsorption of sodium, water, and other electrolytes.
What are the main types of diuretics?
The main types of diuretics include thiazide diuretics, loop diuretics, potassium-sparing diuretics, and osmotic diuretics. Each type has a different mechanism of action and is used for specific medical conditions.
What are the potential side effects of diuretics?
Common side effects of diuretics include increased urination, electrolyte imbalances (such as low potassium levels), dehydration, dizziness, and muscle cramps. Serious side effects may include severe electrolyte disturbances or impaired kidney function.
Can diuretics interact with other medications?
Yes, diuretics can interact with other medications, especially those that affect electrolyte balance, blood pressure, or kidney function. It’s important to inform your healthcare provider about all the medications you’re taking to avoid potential interactions.
How should I take diuretics?
Diuretics should be taken as prescribed by your healthcare provider. Follow the recommended dosage and administration instructions. It’s important to take diuretics consistently and not make dosage adjustments without consulting your doctor.
Can diuretics cause potassium loss?
Yes, certain types of diuretics, such as loop and thiazide diuretics, can lead to potassium loss. This is why potassium-rich foods or supplements might be recommended alongside these diuretics to prevent imbalances.
Should I adjust my diet while taking diuretics?
Yes, dietary adjustments are often recommended when taking diuretics. It’s important to maintain proper hydration, consume foods rich in essential electrolytes (sodium, potassium, magnesium), and monitor your intake of alcohol, caffeine, and processed foods.
Can diuretics lead to dehydration?
Diuretics can increase urine output and potentially lead to dehydration if fluid intake is inadequate. It’s important to drink enough fluids to stay properly hydrated while using diuretics.
Can diuretics be used during pregnancy?
The use of diuretics during pregnancy should be carefully considered and prescribed by a healthcare provider. Some diuretics may have risks for the developing fetus, so medical guidance is essential.
Conclusion:
In conclusion, diuretics are a class of medications used to manage conditions related to fluid retention and high blood pressure. They work by influencing the kidney’s filtration and reabsorption processes, leading to increased urine production and reduction of fluid volume in the body. There are different types of diuretics, including thiazide diuretics, loop diuretics, potassium-sparing diuretics, and osmotic diuretics, each with its own mechanism of action and clinical applications.
Diuretics play a crucial role in various medical scenarios, such as managing hypertension, heart failure, edema, and kidney disorders. However, their use requires careful medical supervision and monitoring due to potential side effects like electrolyte imbalances and dehydration. Lifestyle factors, dietary considerations, and potential interactions with other medications should also be taken into account to ensure the safe and effective use of diuretics.
Home | Blog | About Us | Contact Us | Disclaimer