Clotting Factor Assay Calculator: Essential Tool for Coagulation Disorders:

Introduction
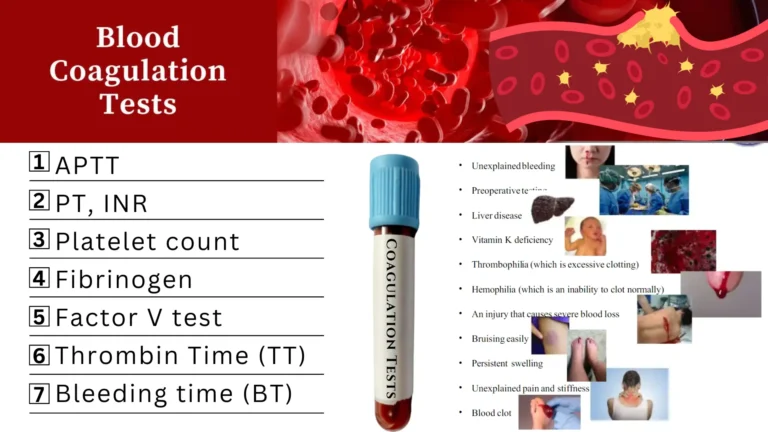
Clotting factor assays quantify specific coagulation factor activity to diagnose bleeding disorders and monitor treatment. These calculations transform coagulation times (PT/aPTT) into factor activity percentages, guiding clinical decisions for:
- Hemophilia A/B (Factor VIII/IX deficiency)
- von Willebrand disease
- Liver failure coagulopathies
- Anticoagulant reversal management
Core Calculation Formulas:
• Dilution Factor: Plasma dilution ratio (e.g., 1:10)
• Reference Concentration: Calibrator value (mg/dL)
• Control Time: Normal pooled plasma clotting time
• Normal Range: 50-150% (factors), 200-400 mg/dL (fibrinogen)
• Dilution Curve: For low-activity samples
• Clauss Method: Gold standard for fibrinogen
• Chromogenic assays preferred for factors VIII, IX, XI
• Immunoassays for antigenic quantification
• Normal PT: 30s, Patient PT: 60s
• Activity = (30/60) × 100 = 50% (mild deficiency)
Fibrinogen (Clauss):
• Ref. time: 15s, Patient: 30s, Calibrator: 300 mg/dL
• Fibrinogen = (15/30) × 300 = 150 mg/dL (hypofibrinogenemia)
• Clauss principle: Thrombin-induced fibrin polymerization
• Inverse relationship: Clotting time ∝ 1/Factor concentration
• Dilution curves account for non-linear kinetics
• Requires factor-deficient plasma as reagent
• Fibrinogen < 100 mg/dL: Spontaneous bleeding risk
• Factor V < 10%: Rare parahemophilia
• Factor XIII deficiency: Normal screening tests
• Factor II < 20%: Severe bleeding diathesis
• Liver disease coagulopathy assessment
• DIC workup: Consumptive factor depletion
• VWD typing: Factor VIII correlation
• Preoperative screening
• Anticoagulant reversal monitoring
• Lupus anticoagulants: May prolong clotting times
• High hematocrit: Affects citrate concentration
• Cold activation: Factor VII overestimation
• Hemolyzed samples: Releases thromboplastins
• Icteric/lipemic samples: Optical interference
• Variable sensitivity to inhibitors
• Reagent-dependent reference ranges
• Dilution errors affect accuracy
• Temperature-sensitive reagents
• Clauss method inaccurate with heparin >1 U/mL
• Factor VIII:C required for hemophilia A diagnosis (normal: 50-150%)
• Clauss method preferred over PT-derived fibrinogen in DIC
• 1:10 dilution minimizes inhibitor interference in factor assays
• Critical fibrinogen < 50 mg/dL → administer cryoprecipitate
• Factor XIII requires urea solubility testing (not detected in clotting assays)
🧪 Clotting Factor & Fibrinogen Assay Calculator
🔍 Overview:
This calculator includes three methods to estimate clotting factor activity or fibrinogen levels. It is useful in diagnosing bleeding disorders and monitoring therapy.
📌 Formula 1 – One-Stage Clotting Assay
📌 Formula 2 – Dilution Curve Method
📌 Formula 3 – Clauss Method for Fibrinogen
1. One-Stage Clotting Assay (Standard Method):
Used for: Factors II, V, VII, VIII, IX, X, XI, XII
Components:
- Normal Plasma Time: Clotting time of control plasma (seconds)
- Patient Plasma Time: Clotting time of diluted patient plasma (typically 1:10 dilution)
Example (Factor VIII):
- Normal plasma time = 35 sec
- Patient plasma time = 70 sec (1:10 dilution)
- Factor VIII = (35 / 70) × 100 = 50% → Mild hemophilia A
2. Factor Activity via Dilution Curve:
For low-activity factors (<20%), use serial dilutions:
Example (Severe Factor IX deficiency):
- 1:100 dilution, Control = 40 sec, Patient = 42 sec
- Factor IX = (1/100) × (40/42) × 100 = 0.95% → Severe hemophilia B
3. Fibrinogen (Factor I) Assay (Clauss Method):
Interpretation Guide:
| Factor Activity | Clinical Significance | Disorder Severity |
|---|---|---|
| >50% | Normal | None |
| 25-50% | Mild deficiency | Mild bleeding |
| 5-25% | Moderate deficiency | Post-traumatic bleeding |
| <5% | Severe deficiency | Spontaneous bleeding |
Key Clinical Applications:
1. Hemophilia Diagnosis
| Disorder | Deficient Factor | Prolonged Test | Typical Activity |
|---|---|---|---|
| Hemophilia A | Factor VIII | aPTT | 0-40% |
| Hemophilia B | Factor IX | aPTT | 0-45% |
2. Liver Disease Coagulopathy
- First affected: Factor VII (shortest half-life)
- Pattern: ↓VII → ↓II, X → ↓V, I
- Critical threshold: Combined factors <20% → High bleeding risk
3. DIC Screening
- Key factors consumed: I, II, V, VIII
- Diagnostic triad:
- ↓Fibrinogen (<150 mg/dL)
- ↑PT/INR
- ↓Platelets
Step-by-Step Calculation Workflow:
- Collect: Patient plasma (citrated tube)
- Dilute: 1:10 in buffered saline (for Factors VIII, IX, XI)
- Perform assay:
- Extrinsic pathway: PT (Factors II, V, VII, X)
- Intrinsic pathway: aPTT (Factors VIII, IX, XI, XII)
- Calculate:
- Compare to normal pooled plasma
- Use dilution correction if needed
- Interpret:
- Isolated factor deficiency → Genetic disorder
- Multiple deficiencies → Acquired condition (liver, DIC)
Critical Considerations
Pre-analytical Errors
❌ Tube overfill/underfill (alters citrate:blood ratio)
❌ Delayed processing (>4 hours for Factor VIII)
❌ Hemolyzed/lipemic samples
Limitations
- Not reliable for:
- Direct oral anticoagulants (DOACs) in sample
- Factor XIII (requires urea solubility test)
- Lupus anticoagulant interference
Case Examples
Case 1: Hemophilia A
- aPTT: 78 sec (normal 25-35 sec)
- Factor VIII: 12%
- Interpretation: Moderate hemophilia A
- Treatment: Recombinant Factor VIII infusion
Case 2: Liver Cirrhosis
- PT: 22 sec (normal 12 sec)
- Factor VII: 18%
- Factor V: 32%
- Action: Vitamin K + FFP before paracentesis
Factor-Specific Notes
| Factor | Stability | Special Handling |
|---|---|---|
| V | Labile (4 hr) | Process immediately |
| VIII | Labile (4 hr) | Snap freeze plasma |
| vWF | Stable | Requires ristocetin cofactor test |
| XIII | Stable | Requires urea solubility test |
Conclusion
Clotting factor assays transform coagulation times into quantitative factor activity percentages that guide diagnosis and management of bleeding disorders. Key principles:
- Use 1:10 dilution for intrinsic factors
- Apply dilution correction formulas for levels <20%
- Always correlate with clinical context