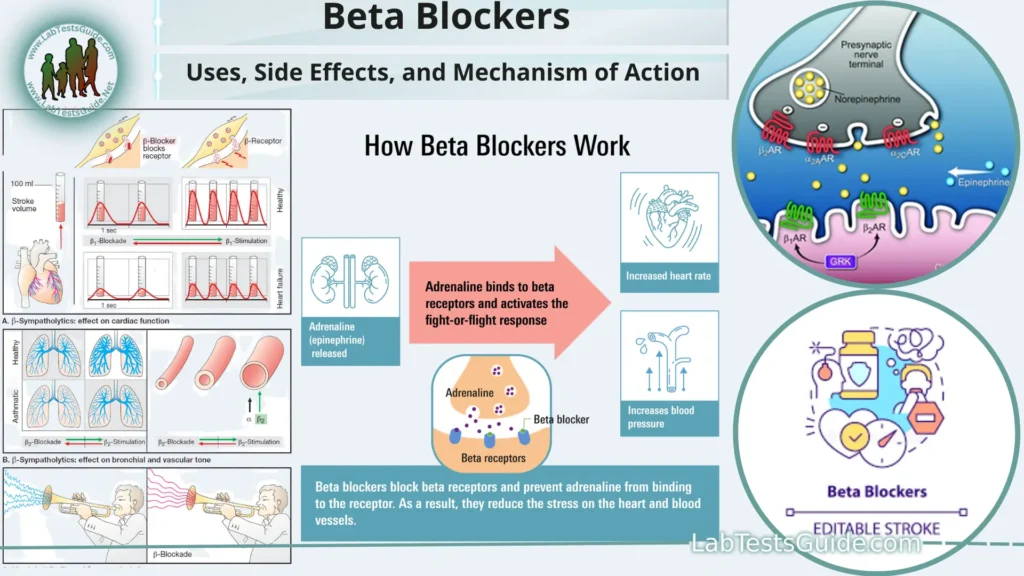
Beta blockers, also known as beta-adrenergic blocking agents, are a class of medications commonly used to treat various cardiovascular conditions. They work by blocking the effects of the hormone epinephrine (adrenaline) on beta receptors found in the heart and other parts of the body. By doing so, beta blockers help reduce heart rate, lower blood pressure, and improve the heart’s overall efficiency.
Definition of Beta Blockers.
Beta blockers, also known as beta-adrenergic blocking agents, are a class of medications used to treat various cardiovascular and medical conditions. These drugs work by blocking the effects of the hormone epinephrine (adrenaline) and related compounds on beta-adrenergic receptors in the body.
Indications for Beta Blockers:
Here are some common indications for beta blockers.
- Hypertension (High Blood Pressure): Beta blockers reduce heart rate and cardiac output, leading to decreased blood pressure. They are often used as a first-line or second-line treatment for hypertension.
- Angina (Chest Pain): Beta blockers help relieve angina symptoms by reducing the heart’s demand for oxygen. This is achieved through lowering heart rate and blood pressure, which in turn decreases the workload on the heart.
- Arrhythmias (Irregular Heartbeats): Beta blockers are used to manage certain types of arrhythmias, especially those that involve excessive heart rate or irregular rhythms. They can help stabilize the heart’s electrical activity.
- Heart Failure: Some beta blockers are prescribed to individuals with heart failure. They improve heart function by reducing the workload on the heart and promoting more efficient pumping.
- Myocardial Infarction (Heart Attack): Beta blockers can be given to patients who have had a heart attack to reduce the risk of subsequent heart attacks and improve cardiac function during the recovery phase.
Migraine Prevention: Certain beta blockers, such as propranolol, are used to prevent migraines. The exact mechanism by which they prevent migraines is not fully understood, but it may involve reducing the sensitivity of blood vessels and the transmission of pain signals.
Essential Tremor: Beta blockers, particularly propranolol, are sometimes prescribed to manage essential tremor, a neurological disorder characterized by involuntary shaking.
Thyrotoxicosis (Thyroid Storm): In cases of severe hyperthyroidism or thyroid storm, beta blockers can help control symptoms like rapid heart rate and high blood pressure until more specific treatments for thyroid function can take effect.
Glaucoma: Eye drops containing beta blockers may be used to lower intraocular pressure in patients with open-angle glaucoma, reducing the risk of optic nerve damage and vision loss.
Performance Anxiety and Stage Fright: Beta blockers can be taken on an as-needed basis by individuals who experience performance anxiety or stage fright. They can help reduce symptoms like trembling and a racing heart.
Types of Beta Blockers:
Here are the two main types of beta blockers.
Selective (Cardioselective) Beta Blockers:
- These beta blockers primarily target beta-1 adrenergic receptors, which are mainly found in the heart and kidneys. By selectively blocking these receptors, they have a more specific effect on the heart without significantly affecting beta-2 receptors in other parts of the body. This selectivity reduces the risk of side effects associated with beta-2 receptor blockade, such as bronchoconstriction (narrowing of the airways) and peripheral vasoconstriction (constriction of blood vessels). Selective beta blockers are often preferred for patients with certain medical conditions, such as asthma or chronic obstructive pulmonary disease (COPD).
Examples of selective beta blockers include:
- Metoprolol (brand names: Lopressor, Toprol XL)
- Atenolol (brand names: Tenormin)
- Bisoprolol (brand names: Zebeta, Ziac)
Nonselective Beta Blockers:
- Nonselective beta blockers block both beta-1 and beta-2 adrenergic receptors, which can have a more comprehensive effect on the body. While these medications are effective in reducing heart rate and blood pressure, they may also lead to side effects related to beta-2 receptor blockade, such as bronchospasm, cold extremities, and alterations in glucose metabolism.
- Examples of nonselective beta blockers include:
- Propranolol (brand names: Inderal, InnoPran XL)
- Nadolol (brand names: Corgard)
- Timolol (brand names: Blocadren, Timoptic)
Commonly Prescribed Beta Blockers:
Here are some of the commonly prescribed beta blockers.
Metoprolol:
- Brand Names: Lopressor, Toprol XL
- Type: Selective beta-1 blocker
- Indications: Hypertension, angina, heart failure, post-heart attack care, and arrhythmias.
Atenolol:
- Brand Names: Tenormin
- Type: Selective beta-1 blocker
- Indications: Hypertension, angina, and prevention of future heart attacks.
Propranolol:
- Brand Names: Inderal, InnoPran XL
- Type: Nonselective beta blocker
- Indications: Hypertension, angina, migraines, essential tremor, anxiety disorders, and arrhythmias.
Bisoprolol:
- Brand Names: Zebeta, Ziac
- Type: Selective beta-1 blocker
- Indications: Hypertension, heart failure.
Nadolol:
- Brand Names: Corgard
- Type: Nonselective beta blocker
- Indications: Hypertension, angina, and prevention of migraines.
Carvedilol:
- Brand Names: Coreg, Coreg CR
- Type: Nonselective beta blocker with alpha-1 blocking activity
- Indications: Hypertension, heart failure, and post-heart attack care.
Labetalol:
- Brand Names: Trandate, Normodyne
- Type: Nonselective beta blocker with alpha-1 blocking activity
- Indications: Hypertension, particularly in emergencies.
Timolol:
- Brand Names: Blocadren, Timoptic
- Type: Nonselective beta blocker
- Indications: Glaucoma (as eye drops), hypertension, and prevention of migraines.
Sotalol:
- Brand Names: Betapace, Sorine
- Type: Nonselective beta blocker with Class III antiarrhythmic properties
- Indications: Arrhythmias, including atrial fibrillation and ventricular tachycardia.
Acebutolol:
- Brand Name: Sectral
- Type: Cardioselective beta-1 blocker with intrinsic sympathomimetic activity (ISA)
- Indications: Hypertension and arrhythmias.
Mechanism of Action:
There are primarily two types of beta receptors: beta-1 and beta-2.
Blocking Beta-1 Receptors:
- Beta-1 receptors are primarily located in the heart and kidneys. When stimulated by epinephrine or norepinephrine (stress hormones), they lead to increased heart rate and the force of heart contractions. This, in turn, increases cardiac output and blood pressure.
- Beta blockers, particularly selective beta blockers, block these beta-1 receptors. By doing so, they reduce the heart’s response to stress hormones. This results in:
- Lower heart rate: Beta blockers slow down the heart rate, reducing the number of beats per minute.
- Decreased force of contraction: Beta blockers decrease the strength with which the heart contracts, reducing its workload.
- Lower blood pressure: As a consequence of reduced heart rate and force of contraction, blood pressure is lowered.
Potential Blockade of Beta-2 Receptors (in nonselective beta blockers):
- Beta-2 receptors are primarily found in the lungs, blood vessels, and certain other tissues. Activation of beta-2 receptors causes bronchodilation (widening of the airways), vasodilation (relaxation of blood vessels), and other effects.
- Nonselective beta blockers block both beta-1 and beta-2 receptors. This can lead to side effects such as bronchoconstriction (narrowing of the airways) and vasoconstriction (constriction of blood vessels), which may be undesirable in some patients.
Side Effects and Precautions:
Here are some common side effects and precautions associated with beta blocker use.
Common Side Effects:
- Fatigue or Tiredness: Beta blockers can cause fatigue or a feeling of tiredness, which may affect daily activities. This is due to the medication’s ability to lower heart rate and reduce cardiac output.
- Cold Hands or Feet: Some people may experience cold extremities (hands and feet) as beta blockers can reduce blood flow to the extremities.
- Dizziness or Lightheadedness: Changes in blood pressure or heart rate can lead to dizziness or lightheadedness, especially when getting up quickly from a sitting or lying position.
- Slow Heart Rate (Bradycardia): Beta blockers can lower heart rate, which is typically desirable in certain medical conditions. However, excessive slowing of the heart rate (bradycardia) can be a concern and may require dosage adjustments.
- Insomnia or Sleep Disturbances: Some people may experience sleep problems, including difficulty falling asleep or staying asleep, while taking beta blockers.
- Gastrointestinal Distress: Gastrointestinal symptoms such as nausea, vomiting, or diarrhea can occur in some individuals.
- Depression or Mood Changes: Beta blockers can affect mood in some people, leading to feelings of depression or mood changes. It’s essential to communicate any significant mood changes with a healthcare provider.
Precautions and Considerations:
- Asthma and Respiratory Conditions: Nonselective beta blockers may worsen respiratory conditions like asthma or chronic obstructive pulmonary disease (COPD) due to their potential to block beta-2 receptors in the lungs. Cardioselective beta blockers are usually preferred for individuals with these conditions, but caution is still necessary.
- Diabetes: Beta blockers can mask some of the early signs of low blood sugar (hypoglycemia) in individuals with diabetes. People with diabetes should monitor their blood sugar levels closely when taking beta blockers.
- Abrupt Discontinuation: Beta blockers should not be stopped suddenly without consulting a healthcare provider. Abrupt discontinuation can lead to rebound high blood pressure, angina, or arrhythmias.
- Heart Failure: Beta blockers are commonly used to treat heart failure, but initiation and dose adjustments should be carefully monitored by a healthcare provider to avoid worsening heart failure symptoms.
- Allergies: Patients with a history of severe allergic reactions (anaphylaxis) should be cautious when using beta blockers, as they may make it more challenging to treat such reactions.
- Peripheral Vascular Disease: Beta blockers can potentially worsen peripheral vascular disease, leading to reduced blood flow in the limbs. Close monitoring is essential in individuals with this condition.
- Pregnancy and Breastfeeding: The use of beta blockers during pregnancy should be carefully considered, and their safety during breastfeeding should be discussed with a healthcare provider.
Monitoring and Consultation:
Regular Follow-Up Appointments:
- Patients prescribed beta blockers should schedule and attend regular follow-up appointments with their healthcare provider.
- These appointments allow the healthcare provider to monitor the patient’s response to the medication, check for potential side effects, and make any necessary adjustments to the treatment plan.
- Blood Pressure Monitoring: Monitoring blood pressure is a crucial part of managing conditions like hypertension (high blood pressure).
Patients may be advised to measure their blood pressure at home regularly and record the results to share with their healthcare provider. - Heart Rate Monitoring: For certain conditions like arrhythmias, monitoring heart rate is important.
Patients may be asked to keep track of their heart rate at home using a pulse oximeter or similar device, especially if they have a history of irregular heartbeats. - Symptoms Assessment: Patients should pay attention to how they feel and report any new or worsening symptoms to their healthcare provider.
This includes symptoms like dizziness, lightheadedness, shortness of breath, changes in mood, or any unusual side effects. - Medication Adherence: It’s crucial to take beta blockers as prescribed by your healthcare provider. Missing doses or discontinuing the medication without consultation can have adverse effects.
- Dosage Adjustments: Beta blocker dosages may need to be adjusted over time, especially during the initial phase of treatment.
Dosage adjustments are typically made based on the patient’s response, blood pressure readings, and any side effects experienced. - Addressing Concerns and Questions: Patients should not hesitate to ask questions or express concerns about their beta blocker therapy during follow-up appointments.
Open communication with the healthcare provider helps ensure that the treatment plan is tailored to the patient’s needs. - Regular Health Check-ups: In addition to monitoring the effects of beta blockers, healthcare providers may recommend routine health check-ups to assess overall cardiovascular health and address other risk factors, such as cholesterol levels and diabetes management.
- Specialized Testing: Depending on the specific condition being treated, healthcare providers may order specialized tests, such as electrocardiograms (ECGs or EKGs), echocardiograms, or Holter monitoring, to assess cardiac function and rhythm.
- Consultation for Lifestyle Modifications: Healthcare providers may offer guidance on lifestyle modifications to complement beta blocker therapy. These may include recommendations for diet, exercise, smoking cessation, and alcohol consumption.
- Emergency Situations: Patients should be aware of the signs of worsening conditions, such as chest pain, severe shortness of breath, or irregular heart rhythms, and know how to seek immediate medical attention in case of emergencies.
Discontinuation of Beta Blockers:
Here are important considerations regarding the discontinuation of beta blockers.
Consultation with a Healthcare Provider:
- Before discontinuing beta blockers, it is essential to consult with your healthcare provider. Do not stop taking beta blockers without their guidance.
Gradual Tapering:
- Beta blockers should be gradually tapered rather than stopped abruptly. Tapering involves reducing the dose of the medication over a period of time.
- The specific tapering schedule depends on factors such as the type of beta blocker, the dosage, and the reason for discontinuation.
Reasons for Discontinuation:
- There are various reasons why a healthcare provider may consider discontinuing beta blockers. Some common reasons include:
- Improvement in the medical condition for which beta blockers were prescribed.
- The development of side effects that outweigh the benefits of treatment.
- Transition to alternative treatments or medications.
Monitoring During Tapering:
- During the tapering process, the healthcare provider will monitor the patient’s vital signs, such as blood pressure and heart rate, to assess how the body responds to the reduction in medication.
- Patients may also be monitored for any return of symptoms that were initially being treated with beta blockers.
Individualized Approach:
- The tapering schedule is individualized and can vary widely. It depends on factors such as the patient’s overall health, the condition being treated, the duration of beta blocker use, and the specific beta blocker used.
Potential Rebound Effects:
- Discontinuation of beta blockers may lead to rebound effects, including:
- Rebound hypertension (a sudden increase in blood pressure).
- Rebound tachycardia (a sudden increase in heart rate).
- Rebound angina (chest pain in individuals with angina).
- These effects can be more pronounced if the medication is stopped abruptly.
Alternative Therapies:
- In some cases, discontinuation of beta blockers may be part of a treatment plan that involves transitioning to alternative therapies or medications.
- Healthcare providers will consider the most appropriate treatment options for the patient’s specific medical condition.
- Communicate with the Healthcare Provider: Patients should communicate any symptoms or concerns they experience during the tapering process to their healthcare provider promptly.
- Follow-Up Care: After discontinuing beta blockers, patients may need ongoing follow-up care to monitor their health and adjust treatment as needed.
- Lifestyle Management: Depending on the underlying condition, lifestyle modifications, such as dietary changes and exercise, may play a role in managing health after discontinuation of beta blockers.
FAQs:
What are beta blockers?
Beta blockers, also known as beta-adrenergic blocking agents, are a class of medications used to treat various cardiovascular conditions. They work by blocking the effects of adrenaline on beta receptors in the body.
What conditions are beta blockers commonly used to treat?
Beta blockers are used to treat conditions such as hypertension (high blood pressure), angina (chest pain), arrhythmias (irregular heartbeats), heart failure, migraines, and essential tremor.
How do beta blockers work?
Beta blockers primarily reduce heart rate, lower blood pressure, and decrease the force of heart contractions by blocking the action of adrenaline on beta receptors in the heart.
Are all beta blockers the same?
No, there are different types of beta blockers, including selective (cardioselective) and nonselective beta blockers. Selective beta blockers primarily target beta-1 receptors in the heart, while nonselective beta blockers affect both beta-1 and beta-2 receptors.
Can beta blockers cause side effects?
Yes, beta blockers can cause side effects, including fatigue, cold extremities, dizziness, slow heart rate (bradycardia), insomnia, and gastrointestinal disturbances. The specific side effects can vary depending on the type and dosage of the beta blocker.
Can beta blockers be used in patients with respiratory conditions like asthma?
Selective beta blockers are generally preferred for patients with asthma or chronic obstructive pulmonary disease (COPD) because they have a reduced effect on beta-2 receptors in the lungs. However, caution is still necessary, and these patients should be closely monitored.
Is it safe to stop beta blockers abruptly?
No, it is not safe to stop beta blockers abruptly. Stopping these medications suddenly can lead to rebound effects, including an increase in blood pressure, heart rate, or chest pain. The discontinuation should be done gradually under the guidance of a healthcare provider.
Can beta blockers be used during pregnancy or while breastfeeding?
The use of beta blockers during pregnancy or while breastfeeding should be carefully considered and discussed with a healthcare provider. The benefits and risks must be weighed on an individual basis.
Are there interactions with other medications?
Yes, beta blockers can interact with other medications, including some over-the-counter drugs and supplements. It’s important to inform your healthcare provider of all medications you are taking to avoid potential interactions.
Can beta blockers be used to treat anxiety or stage fright?
Yes, beta blockers like propranolol are sometimes used off-label to manage symptoms of performance anxiety or stage fright. They can help reduce physical symptoms such as trembling and a racing heart.
Conclusion:
In conclusion, beta blockers are a versatile class of medications widely used in the treatment of various cardiovascular conditions, including hypertension, angina, arrhythmias, and heart failure. Their mechanism of action, which involves blocking the effects of adrenaline on beta receptors, leads to a reduction in heart rate, lowered blood pressure, and improved cardiac function. While beta blockers can be highly effective, their administration, dosage, and discontinuation require careful monitoring and consultation with a healthcare provider to ensure patient safety and the optimal management of specific medical conditions. Patients should actively engage in their healthcare, report any side effects or concerns, and follow their healthcare provider’s guidance for the best possible outcomes.