Acute Promyelocytic Leukemia (APL) Test: PML-RARA Detection, Diagnosis, Procedure & Results Guide
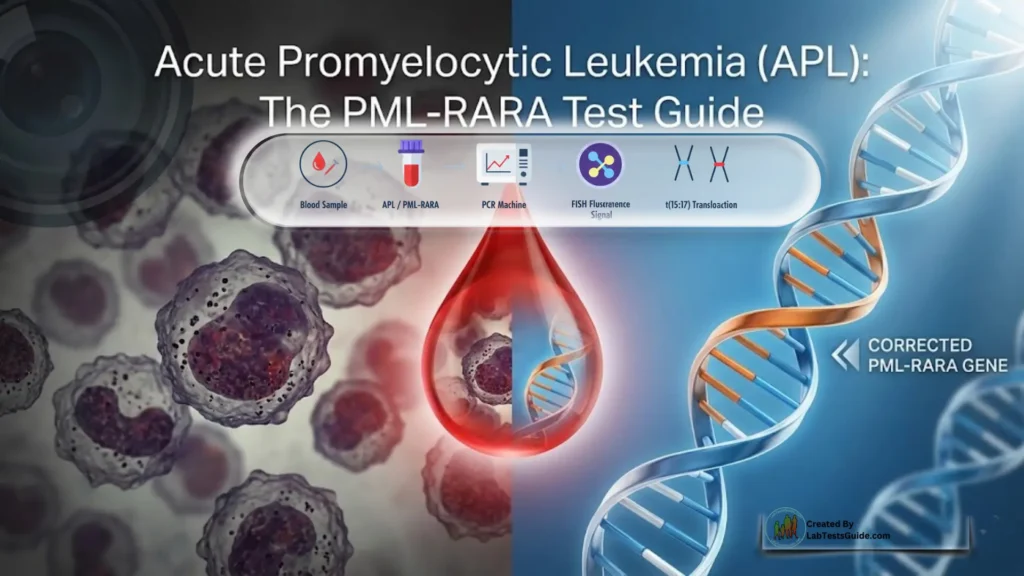
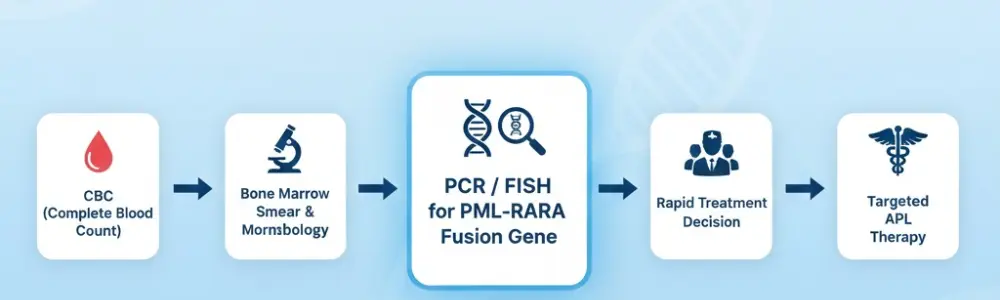
An acute promyelocytic leukemia (APL) test includes blood tests (complete blood count, coagulation studies), a bone marrow biopsy, and specialized genetic tests such as fluorescence in situ hybridization (FISH) and polymerase chain reaction (PCR) to identify the specific PML/RARα gene fusion, confirming the diagnosis and guiding urgent and highly effective treatment, often with all-trans retinoic acid (ATRA). These tests analyze cell appearance, counts, chromosomal changes, and genetic mutations to differentiate APL from other leukemias.
Understand Your Test Results:
Understand your Acute Promyelocytic Leukemia (APL) Test: PML-RARA Detection, Diagnosis, Procedure & Results Guide Results
AI-powered Lab Test Results Meaning tool 🤖
Acute Promyelocytic Leukemia (APL) Test Quick Review:
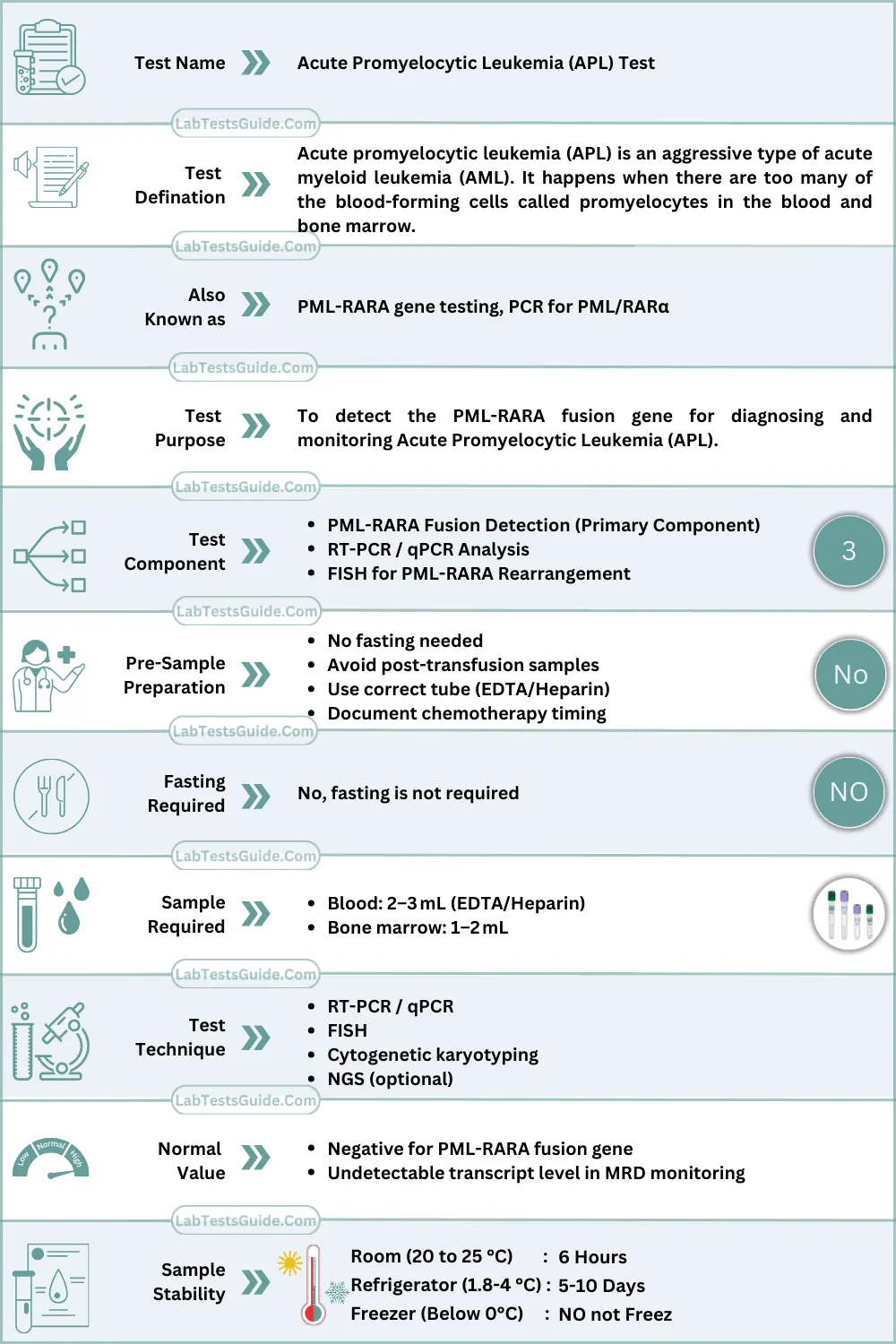
What is Acute Promyelocytic Leukemia Test?
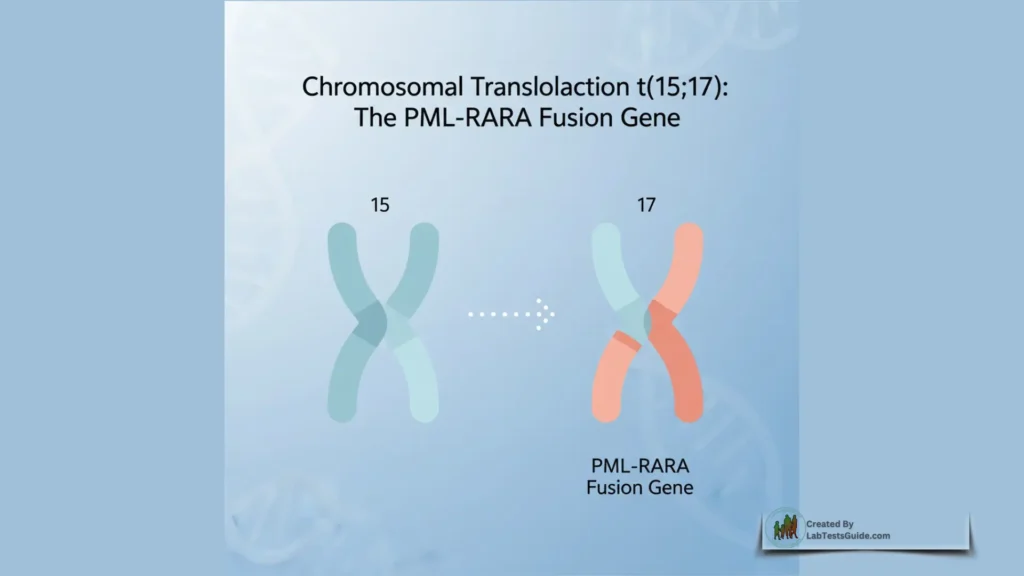
The Acute Promyelocytic Leukemia (APL) Test detects the abnormal fusion gene PML-RARA, which occurs due to a chromosomal translocation t(15;17). This test helps diagnose APL, guide immediate treatment, and monitor patients for remission or relapse.
Why Is Acute Promyelocytic Leukemia Test Done? (Indications)
For Patients / General Use:
- Unexplained bleeding or bruising
- Frequent nosebleeds or gum bleeding
- Fatigue, weakness
- Fever or recurrent infections
- Unusual skin spots or petechiae
- Bone pain or unexplained anemia
- Elevated or low white blood cell count in routine tests
For Doctors / Clinical Use:
- Confirming diagnosis of suspected APL
- Detecting PML-RARA gene abnormality using PCR or FISH
- Determining treatment strategy (ATRA/arsenic)
- Monitoring minimal residual disease (MRD)
- Assessing molecular remission
- Detecting early relapse
- Classification of leukemia subtypes in acute leukemia panels
How the Acute Promyelocytic Leukemia Test Works (Principle / Methodology):
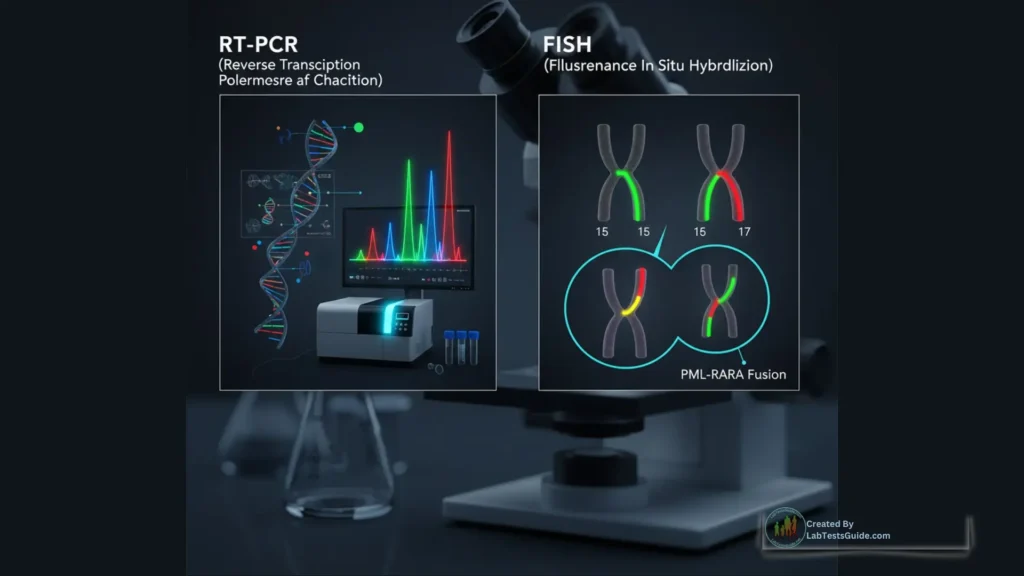
- RT-PCR / qPCR: Detects and quantifies the PML-RARA fusion transcript created by t(15;17). Highly sensitive; used for MRD monitoring.
- FISH (Fluorescence In Situ Hybridization): Uses fluorescent probes to visualize fusion of the PML and RARA genes.
- Cytogenetic Karyotyping: Identifies the characteristic t(15;17) translocation under the microscope.
- Next-Generation Sequencing (NGS): Detects rare or variant fusion patterns.
These methods identify the presence or absence of the fusion gene responsible for APL.
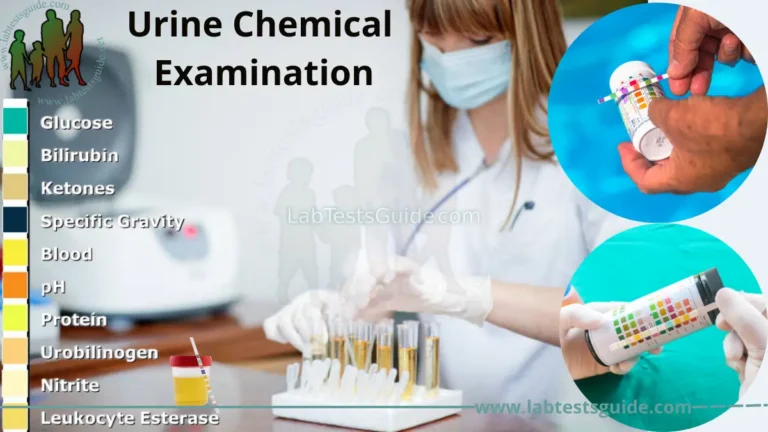
Acute Promyelocytic Leukemia Test Specimen Requirements & Collection
Specimen Type
- Peripheral blood
- Bone marrow aspirate (preferred for initial diagnosis)
Tube Type
- EDTA tube for PCR (lavender top)
- Sodium heparin tube for FISH/cytogenetics (green top)
Volume
- Blood: 2–3 mL
- Bone marrow: 1–2 mL
Patient Preparation
- No fasting required
- Avoid collection post-transfusion if possible
Collection Steps
- Perform venipuncture under aseptic technique.
- Collect required volume gently to avoid clots.
- Invert tube 6–8 times to mix anticoagulant.
- Avoid delays to preserve cell and RNA integrity.
Transport & Storage
- Transport at room temperature within 24 hours.
- Do NOT freeze whole blood for molecular testing.
- If delay expected, store at 2–8°C (short period).
- RNA samples should be stabilized if shipping long-distance.
Acute Promyelocytic Leukemia Test Reference Ranges
| Population | Reference Range | Units |
|---|---|---|
| Adults | Not Detected for PML-RARA | Qualitative |
| Children | Not Detected for PML-RARA | Qualitative |
| MRD Monitoring | Undetectable transcript level | Quantitative |
Note: Reference ranges vary by laboratory.
In pregnancy, interpretation is same as adult ranges.
Acute Promyelocytic Leukemia Test Interpretation of Results
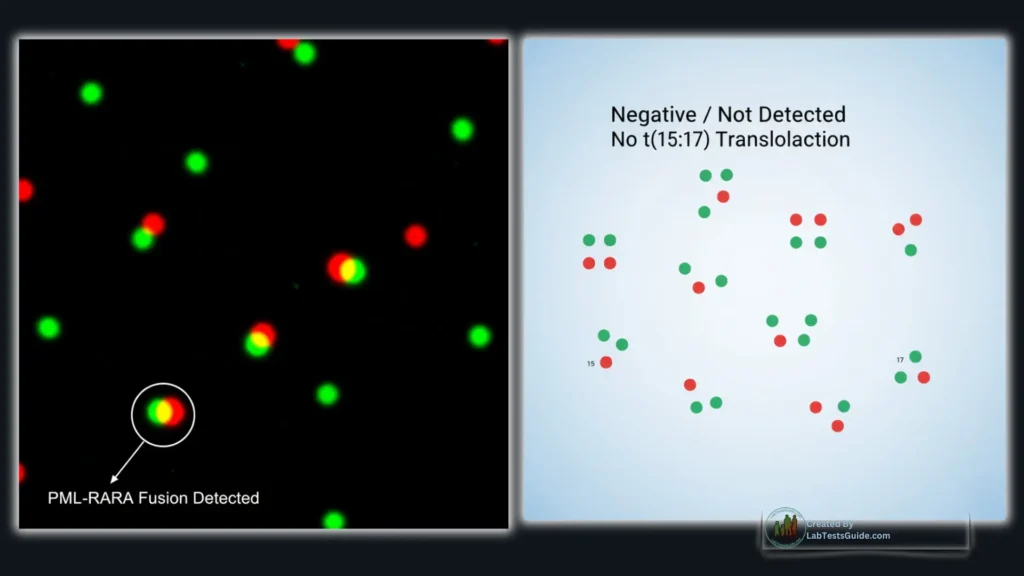
Positive for PML-RARA (High Levels / Abnormal)
Causes
- Acute Promyelocytic Leukemia (APL)
Differential Diagnoses
- Variant APL with atypical fusion partners
- Acute myeloid leukemia (other translocations—rare overlap)
Clinical Relevance
- Confirms diagnosis of APL
- Requires immediate treatment due to risk of fatal bleeding
- Helps guide therapy with ATRA + arsenic trioxide
- Used for baseline and follow-up MRD levels
Negative for PML-RARA (Low or Undetectable Levels)
Causes
- No APL
- Leukemia subtype other than APL
- Technical issues (poor sample, degraded RNA)
Differential Diagnoses
- Acute Myeloid Leukemia (AML) without t(15;17)
- Cytopenias from other causes (infection, aplastic anemia, drugs)
Clinical Relevance
- Rules out classic APL
- If clinical suspicion persists, repeat test or use NGS/fusion panels
Acute Promyelocytic Leukemia Test Interfering Factors / Pre-Analytical Errors:

- Hemolysis: May degrade RNA quality
- Lipemia: Can affect extraction purity
- Icterus: Mild effect on PCR quantification
- Medications: Chemotherapy may reduce detectable transcripts
- Sample handling: Delayed processing → RNA degradation
- Improper tube: Heparin may inhibit PCR
- Biological variation: Low transcript levels early in remission
Acute Promyelocytic Leukemia Test Nursing / Phlebotomy Notes
- Use EDTA (lavender) or heparin (green) tube depending on the test method.
- Mix gently after collection.
- Label sample with full patient identifiers.
- Do not refrigerate for extended periods.
- Avoid freezing whole blood.
- Send to the molecular/cytogenetic lab immediately.
Acute Promyelocytic Leukemia Test Lab Student Key Points
- APL is linked to t(15;17) → PML-RARA fusion.
- PCR is most sensitive; FISH is confirmatory.
- APL is a medical emergency due to DIC risk.
- MRD monitoring requires qPCR.
- Sample integrity is crucial for RNA tests.
Understand Your Test Results:
Understand your Acute Promyelocytic Leukemia (APL) Test: PML-RARA Detection, Diagnosis, Procedure & Results Guide Results
AI-powered Lab Test Results Meaning tool 🤖
Is this test only for leukemia?
Yes, it specifically detects APL-related gene changes.
How long does the test take?
PCR results may be available within 24–48 hours.
Is bone marrow mandatory?
Blood can be used, but bone marrow is more accurate for diagnosis.
Do I need to fast?
No fasting is required.
Can the test show if my treatment is working?
Yes, PCR monitoring is used to track remission and relapse.
Can medications affect the result?
Chemotherapy may reduce detectable transcripts.
Is the test painful?
Blood tests are simple; bone marrow tests may cause temporary discomfort.