Differences | Similarities | Definitions | Functions | FAQs
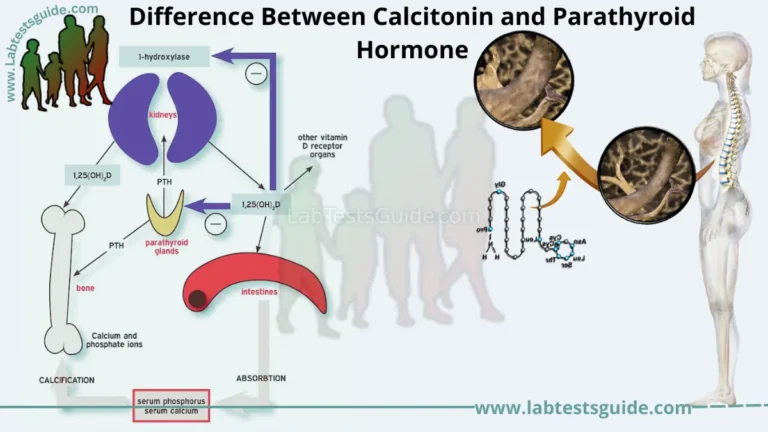
Parathyroid Hormone vs Intact Parathyroid Hormone: Parathyroid hormone (PTH) and intact parathyroid hormone (iPTH) are both forms of the hormone produced by the parathyroid glands, which are located in the neck and play a critical role in regulating calcium and phosphorus levels in the body.

Definations:
Definition of Parathyroid Hormone:
Parathyroid hormone (PTH) is a hormone secreted by the parathyroid glands that plays a critical role in regulating calcium and phosphorus levels in the body. PTH acts on the bones, kidneys, and intestines to increase calcium levels in the bloodstream.
Definition of Intact Parathyroid Hormone:
Intact parathyroid hormone (iPTH) is a specific form of parathyroid hormone that consists of the full-length, biologically active molecule. It is distinguished from other fragments of PTH that may be present in the bloodstream, which are produced during the degradation of PTH in the liver and kidneys. iPTH is often used in the diagnosis and monitoring of disorders related to parathyroid gland function.
Functions:
Functions of Parathyroid Hormone:
Here are some functions of parathyroid hormone (PTH):
- Regulates Calcium Homeostasis: PTH plays a key role in maintaining calcium balance in the body by increasing calcium levels in the blood. It does this by promoting the release of calcium from bones, reducing calcium excretion in the kidneys, and increasing calcium absorption in the intestines.
- Increases Phosphorus Levels: PTH also increases the levels of phosphorus in the blood by promoting the release of phosphorus from bones and increasing the reabsorption of phosphorus in the kidneys.
- Stimulates Vitamin D Production: PTH stimulates the production of active vitamin D (calcitriol) in the kidneys, which helps to increase calcium and phosphorus absorption in the intestines.
- Regulates Bone Remodeling: PTH plays a role in bone remodeling by stimulating osteoclasts to break down bone tissue, which releases calcium and phosphorus into the bloodstream.
- Maintains Normal Heart and Muscle Function: Calcium is essential for normal heart and muscle function, and PTH helps to ensure that calcium levels are maintained within the appropriate range.
These are some of the main functions of parathyroid hormone, although there may be other roles that PTH plays in the body as well.
Functions of Intact Parathyroid Hormone:
Intact parathyroid hormone (iPTH) is the full-length, biologically active form of parathyroid hormone (PTH). Its functions include:
- Regulating Calcium and Phosphorus Levels: Like PTH, iPTH helps to regulate calcium and phosphorus levels in the body by stimulating the release of calcium from bones, increasing calcium and phosphorus absorption in the intestines, and reducing calcium and phosphorus excretion in the kidneys.
- Maintaining Bone Health: iPTH plays a role in maintaining bone health by stimulating bone remodeling and helping to prevent bone loss.
- Supporting Kidney Function: iPTH helps to regulate kidney function by promoting the reabsorption of calcium and phosphorus in the kidneys.
- Diagnosing and Monitoring Parathyroid Disorders: iPTH levels can be used to diagnose and monitor disorders related to the parathyroid gland, such as hyperparathyroidism and hypoparathyroidism.
- Evaluating Bone Mineral Density: iPTH levels can also be used in conjunction with other tests to evaluate bone mineral density and assess the risk of osteoporosis.
These are some of the main functions of intact parathyroid hormone, although there may be other roles that iPTH plays in the body as well.
Differences Between Parathyroid Hormone vs Intact Parathyroid Hormone :
Here are differences between parathyroid hormone (PTH) and intact parathyroid hormone (iPTH) with headings and brief explanations:
- Definition and Structure:
- PTH is a hormone produced by the parathyroid glands that plays a critical role in regulating calcium and phosphorus levels in the body.
- iPTH is a specific form of PTH that consists of the full-length, biologically active molecule.
- Production:
- PTH is synthesized and secreted by the parathyroid glands in response to changes in blood calcium levels.
- iPTH is produced and secreted in the same way as PTH.
- Measurement:
- PTH levels are measured using various assays that detect fragments of PTH in the bloodstream, including intact and fragmented forms.
- iPTH levels are specifically measured using an assay that detects only the full-length, intact molecule of PTH.
- Clinical Applications:
- PTH levels are used to diagnose and monitor disorders related to calcium and phosphorus metabolism, such as hyperparathyroidism and hypoparathyroidism.
- iPTH levels are primarily used to assess parathyroid function and diagnose disorders related to the parathyroid gland, such as primary hyperparathyroidism.
- Reference Ranges:
- The reference range for PTH levels varies depending on the assay used and the laboratory performing the test.
- The reference range for iPTH levels is generally narrower and more standardized across laboratories.
- Stability:
- PTH is relatively unstable and has a short half-life in the bloodstream.
- iPTH is more stable than PTH and has a longer half-life in the bloodstream.
- Molecular Weight:
- PTH has a larger molecular weight than iPTH.
- iPTH has a smaller molecular weight than PTH.
- Processing:
- PTH is processed into various fragments in the liver and kidneys.
- iPTH is not subject to processing in the same way as PTH.
- Biological Activity:
- PTH fragments may have different biological activities and potencies than intact PTH.
- iPTH is the biologically active form of PTH and has the highest potency in terms of its effects on calcium and phosphorus metabolism.
- Cost:
- PTH assays are generally less expensive than iPTH assays.
- iPTH assays are generally more expensive than PTH assays.
These are some of the main differences between PTH and iPTH, although there may be other distinctions as well.
Table of Differences:
| Difference | PTH | iPTH |
|---|---|---|
| Definition | A peptide hormone | The full-length, biologically active form of PTH |
| Structure | Large, complex molecule | Full-length, intact molecule of PTH |
| Measurement | Detected in various assays, including intact and fragmented forms | Specifically measured using an assay that detects only the full-length, intact molecule of PTH |
| Clinical Applications | Used to diagnose and monitor disorders related to calcium and phosphorus metabolism, such as hyperparathyroidism and hypoparathyroidism | Used to assess parathyroid function and diagnose disorders related to the parathyroid gland, such as primary hyperparathyroidism |
| Reference Ranges | Varies depending on assay and laboratory | Narrower and more standardized across laboratories |
| Stability | Relatively unstable with a short half-life in the bloodstream | More stable with a longer half-life in the bloodstream |
| Molecular Weight | Larger molecular weight | Smaller molecular weight |
| Processing | Processed into various fragments in the liver and kidneys | Not subject to processing in the same way as PTH |
| Biological Activity | Fragments may have different biological activities and potencies than intact PTH | Biologically active form of PTH with highest potency |
| Cost | Generally less expensive than iPTH assays | Generally more expensive than PTH assays |
Similaritires Between Parathyroid Hormone vs Intact Parathyroid Hormone:
- Source:
- Both PTH and iPTH are produced by the parathyroid glands.
- Regulation:
- The secretion of both PTH and iPTH is regulated by the same feedback mechanisms that sense changes in blood calcium and phosphorus levels.
- Biological Function:
- Both PTH and iPTH play a critical role in regulating calcium and phosphorus levels in the body.
- Chemical Composition:
- Both PTH and iPTH are composed of amino acids.
- Target Tissues:
- Both PTH and iPTH act on target tissues, such as bones and kidneys, to regulate calcium and phosphorus metabolism.
- Receptor Binding:
- Both PTH and iPTH bind to the same receptors on target tissues, such as the parathyroid hormone receptor (PTH1R) and the calcium-sensing receptor (CaSR).
- Signal Transduction Pathways:
- Both PTH and iPTH activate similar signal transduction pathways in target tissues, including the cyclic adenosine monophosphate (cAMP) and protein kinase A (PKA) pathways.
- Diagnostic Use:
- Both PTH and iPTH levels can be used to diagnose and monitor various disorders related to calcium and phosphorus metabolism.
- Clinical Interpretation:
- Interpretation of both PTH and iPTH levels requires consideration of clinical factors, such as medications and renal function.
- Therapeutic Use:
- Both PTH and iPTH can be used therapeutically in certain conditions, such as osteoporosis.
Table of Similaritires:
| Similarity | PTH | iPTH |
|---|---|---|
| Source | Produced by parathyroid glands | Produced by parathyroid glands |
| Regulation | Secretion regulated by feedback mechanisms | Secretion regulated by feedback mechanisms |
| Biological Function | Regulate calcium and phosphorus levels in the body | Regulate calcium and phosphorus levels in the body |
| Chemical Composition | Composed of amino acids | Composed of amino acids |
| Target Tissues | Act on target tissues, such as bones and kidneys | Act on target tissues, such as bones and kidneys |
| Receptor Binding | Bind to the same receptors on target tissues | Bind to the same receptors on target tissues |
| Signal Transduction Pathways | Activate similar signal transduction pathways in target tissues | Activate similar signal transduction pathways in target tissues |
| Diagnostic Use | Can be used to diagnose and monitor various disorders related to calcium and phosphorus metabolism | Can be used to diagnose and monitor various disorders related to calcium and phosphorus metabolism |
| Clinical Interpretation | Interpretation requires consideration of clinical factors, such as medications and renal function | Interpretation requires consideration of clinical factors, such as medications and renal function |
| Therapeutic Use | Can be used therapeutically in certain conditions, such as osteoporosis | Can be used therapeutically in certain conditions, such as osteoporosis |
FAQs:
What is the normal range for PTH?
The normal range for PTH is typically between 10-65 pg/mL, although the range may vary slightly depending on the laboratory.
What is the normal range for iPTH?
The normal range for iPTH is typically between 10-55 pg/mL, although the range may vary slightly depending on the laboratory.
What causes high PTH levels?
High PTH levels can be caused by various factors, such as vitamin D deficiency, chronic kidney disease, primary hyperparathyroidism, and certain medications.
What causes low PTH levels?
Low PTH levels can be caused by various factors, such as hypoparathyroidism, autoimmune disorders, magnesium deficiency, and certain medications.
What causes high iPTH levels?
High iPTH levels can be caused by similar factors as high PTH levels, such as vitamin D deficiency and primary hyperparathyroidism.
What causes low iPTH levels?
Low iPTH levels can be caused by similar factors as low PTH levels, such as hypoparathyroidism and magnesium deficiency.
What is the role of PTH in bone metabolism?
PTH stimulates bone resorption by activating osteoclasts, which breaks down bone tissue to release calcium and phosphate into the blood.
What is the role of iPTH in bone metabolism?
iPTH has the same role as PTH in bone metabolism, as it also stimulates bone resorption to release calcium and phosphate into the blood.
How is PTH measured?
PTH is typically measured using a blood test, which measures the concentration of PTH in the blood.
How is iPTH measured?
iPTH is also measured using a blood test, which measures the concentration of intact PTH in the blood.
What are the clinical uses of PTH testing?
PTH testing can be used to diagnose and monitor various disorders related to calcium and phosphorus metabolism, such as primary hyperparathyroidism and hypoparathyroidism.
What are the clinical uses of iPTH testing?
iPTH testing can also be used to diagnose and monitor various disorders related to calcium and phosphorus metabolism, such as primary hyperparathyroidism and hypoparathyroidism.
Can PTH or iPTH be used therapeutically?
Yes, PTH and iPTH analogues can be used therapeutically in certain conditions, such as osteoporosis. However, their use is typically reserved for specific cases and requires medical supervision.
Conclusion:
In conclusion, parathyroid hormone (PTH) and intact parathyroid hormone (iPTH) are hormones that play important roles in calcium and phosphorus metabolism in the body. While PTH and iPTH have similar functions, they differ in their molecular structure and the way they are measured. Understanding the differences and similarities between PTH and iPTH is important for diagnosing and managing disorders related to calcium and phosphorus metabolism. Both hormones can be measured through blood tests and used therapeutically in certain cases under medical supervision.
Possible References Used