Test your knowledge of Liver and Kidney Function Tests with this Biochemistry Mock Test (Part 53) .ASCP MLS , AMT , and Clinical Biochemistry exam preparation.
📘 Topics Included Liver enzymes and their diagnostic interpretation Bilirubin metabolism and jaundice classification Kidney markers: urea, creatinine, uric acid GFR estimation and renal clearance concepts Laboratory evaluation of hepatic and renal diseases 🧠 Why Take This Mock Test? Prepare confidently for exam questions on LFTs and KFTs. Reinforce your knowledge of hepatic and renal biochemistry. Practice ASCP-style clinical chemistry questions. Improve your test interpretation and diagnostic reasoning.
Report a question
ASCP MLS Exam MCQs Chapter 53
Why Take This Mock Test? Strengthens exam confidence Highlights areas for improvement Provides practice with clinically relevant scenarios This mock test (60 MCQs (4121 – 4180) ) is part of our ongoing ASCP MLS Exam Practice Series , giving you structured preparation for all major immunology topics.
Our Biochemistry – Liver & Kidney Function Tests Mock Test is specifically designed for candidates appearing in ASCP MLS, AMT MLT/MT, AIMS, CSMLS, IBMS, HAAD/DOH, DHA, and MOH exams. This mock test mirrors the structure, difficulty level, and question style you can expect in the actual examination.
Take this test to:ASCP MLS Exam .
Who Should Use This Mock Test? Medical Laboratory Scientists and Technicians
Pathology Students
Professionals preparing for international laboratory certification exams
Anyone seeking to strengthen their knowledge of Biochemistry – Liver & Kidney Function Tests
How to Use This Mock Test Effectively Simulate Exam Conditions: Attempt the test in one sitting without referring to notes.
Track Your Time: Keep within the allotted time limit to build speed.
Review Explanations: Study the answer explanations to strengthen understanding.
Repeat for Retention: Re-attempt after revision to measure improvement.
1 / 60
Category:
ASCP Exam Questions
The BUN/creatinine ratio helps differentiate:
The BUN/creatinine ratio is primarily used to help determine the cause of acute kidney injury or uremia.
A high ratio (>20:1) often suggests pre-renal causes (like dehydration, heart failure) or post-renal causes (like urinary obstruction).
A normal ratio (10-20:1) typically points to intrinsic renal causes (damage to the kidney itself).
Option breakdown:
a) Liver from kidney failure → Not determined by this ratio.
b) Pre-renal, renal, and post-renal causes of uremia → Correct
c) Bone disease from muscle disease → Involves enzymes (ALP, CK), not BUN/creatinine.
d) Acute from chronic liver injury → Based on ALT/AST, not BUN/creatinine.
2 / 60
Category:
ASCP Exam Questions
Which of the following conditions shows elevated unconjugated bilirubin?
Unconjugated (indirect) bilirubin increases when there is excessive breakdown of red blood cells (RBCs) , producing more bilirubin than the liver can conjugate.
This happens in hemolytic anemia , where accelerated RBC destruction leads to high levels of unconjugated bilirubin in the blood.
Why the other options are incorrect:
b) Bile Duct Obstruction: This causes post-hepatic jaundice . The conjugated bilirubin cannot be excreted into the intestines due to the blockage, so it backs up into the blood.
c) Hepatitis & d) Cirrhosis: These cause hepatic jaundice . Liver cell damage impairs the liver’s ability to take up, conjugate, and/or secrete bilirubin. While both types can be elevated, the hallmark is a buildup of conjugated bilirubin because the damaged hepatocytes leak it back into the bloodstream, and the intrahepatic bile flow is often disrupted.
3 / 60
Category:
ASCP Exam Questions
The normal pathway for bilirubin excretion is through the:
Bilirubin is processed in the liver , where it becomes conjugated (direct) bilirubin .
It is then excreted into bile , which flows into the intestine .
In the intestine, bacteria convert it into urobilinogen and stercobilin , which are excreted mainly in the feces , giving stool its brown color .
A small amount of urobilinogen is reabsorbed and excreted in the urine , but this is not the main route .
Why the other options are incorrect:
a) Urine: Conjugated bilirubin is water-soluble and can be excreted in the urine, but this only happens in significant amounts when there is a pathology, such as biliary obstruction or liver disease. In a healthy person, very little bilirubin is found in the urine.
b) Sweat glands & d) Saliva: These are not routes for bilirubin excretion.
5 / 60
Category:
ASCP Exam Questions
In pre-renal azotemia, the BUN/creatinine ratio is typically:
In pre-renal azotemia (caused by reduced blood flow to the kidneys), the kidneys reabsorb more urea in an effort to conserve water. Creatinine reabsorption is not significantly affected. This disproportionate increase in BUN compared to creatinine results in a high BUN/creatinine ratio (typically >20:1) .
Option breakdown:
a) Normal → Seen in some non-renal conditions, not pre-renal azotemia.
b) Increased (>20:1) → Typical of pre-renal azotemia.
c) Decreased (<10:1) → Seen in renal (intrinsic) azotemia where tubular function is impaired.
d) Unchanged → Incorrect.
6 / 60
Category:
ASCP Exam Questions
In which condition does decreased activity of glucuronyl transferase result in increased unconjugated bilirubin and kernicterus in neonates?
Crigler-Najjar Syndrome is caused by a severe deficiency or absence of the liver enzyme UDP-glucuronosyltransferase (glucuronyl transferase) .
This enzyme is essential for conjugating bilirubin. Its absence leads to a severe buildup of unconjugated bilirubin .
In neonates, this high level of unconjugated bilirubin can cross the blood-brain barrier and cause kernicterus , a form of brain damage.
Gilbert syndrome (a) causes a mild, benign increase in unconjugated bilirubin, but not kernicterus. Rotor (b) and Dubin-Johnson (c) syndromes cause conjugated hyperbilirubinemia.
7 / 60
Category:
ASCP Exam Questions
The conversion of ammonia to urea occurs in the:
The urea cycle (also called the ornithine cycle) is the primary metabolic pathway that converts toxic ammonia into urea for excretion. This vital detoxification process occurs almost exclusively in the liver .
Ammonia, produced from the breakdown of amino acids and other sources in the body, is transported to the liver.
In the liver cells (hepatocytes), the urea cycle converts ammonia and carbon dioxide into urea .
The urea is then released into the bloodstream, filtered by the kidneys, and excreted in the urine.
Why the other options are incorrect:
a) Kidney: The kidneys are responsible for filtering and excreting urea that was produced by the liver. They do not synthesize it.
c) Pancreas: The pancreas produces digestive enzymes and hormones like insulin and glucagon. It is not involved in the urea cycle.
d) Intestine: The intestine can produce ammonia from bacterial action on urea and other compounds, but it does not convert ammonia into urea.
8 / 60
Category:
ASCP Exam Questions
A patient has these findings: total serum bilirubin 8.5 mg/dL, conjugated bilirubin 6.1 mg/dL, increased urine urobilinogen, decreased fecal urobilinogen, positive urine bilirubin, AST 300 U/L. This best represents:
Predominantly conjugated bilirubin (6.1 out of 8.5 mg/dL) → indicates a conjugated hyperbilirubinemia.
Positive urine bilirubin → confirms the presence of water-soluble conjugated bilirubin.
Increased urine urobilinogen → indicates that some conjugated bilirubin is making it to the intestine, being converted to urobilinogen, and being reabsorbed, but the liver is too damaged (hepatocellular disease) to re-process it, so it spills into the urine.
Markedly elevated AST (300 U/L) → direct evidence of hepatocellular injury/damage.
This combination (conjugated hyperbilirubinemia, bilirubinuria, elevated urobilinogen, and high transaminases) is classic for hepatocellular disease (e.g., hepatitis). Pure biliary obstruction (d) would typically show very low or absent urine urobilinogen.
10 / 60
Category:
ASCP Exam Questions
Creatinine clearance is used to estimate the:
Creatinine clearance is a commonly used test to estimate the Glomerular Filtration Rate (GFR) — the rate at which the kidneys filter blood through the glomeruli.
Other Options (for comparison): (a) Tubular Secretion Rate: Measured using substances like PAH (para-aminohippuric acid) .
(c) Renal Blood Flow: Also estimated with PAH clearance .
(d) Urine Concentrating Ability: Evaluated by measuring urine osmolality or specific gravity , not creatinine clearance.
11 / 60
Category:
ASCP Exam Questions
The most sensitive enzymatic indicator for liver damage from chronic ethanol intake is:
GGT is very sensitive for detecting chronic alcohol use and alcohol-related liver injury.
In chronic ethanol intake, GGT rises more consistently and prominently than ALT, AST, or ALP.
AST is often elevated more than ALT in alcoholic liver disease (AST:ALT > 2), but GGT is the most sensitive screening marker for chronic alcohol consumption.
ALP is less specific and more related to cholestasis or bone disease.
12 / 60
Category:
ASCP Exam Questions
Uric acid is the end product of:
Uric acid is the final waste product formed when the body breaks down purines , which are nitrogen-containing compounds found in certain foods (like red meat and seafood) and are also part of the body’s own cells and DNA.
Option breakdown:
a) Protein metabolism → End product is urea , not uric acid.
b) Fat metabolism → End products are ketone bodies or fatty acids .
c) Purine metabolism → Forms uric acid .
d) Pyrimidine metabolism → End products are β-alanine and ammonia , not uric acid.
13 / 60
Category:
ASCP Exam Questions
The first enzyme to become elevated after a myocardial infarction is:
After a myocardial infarction (MI) , Creatine Kinase-MB (CK-MB) is the first enzyme to rise, usually within 3–6 hours of the event.
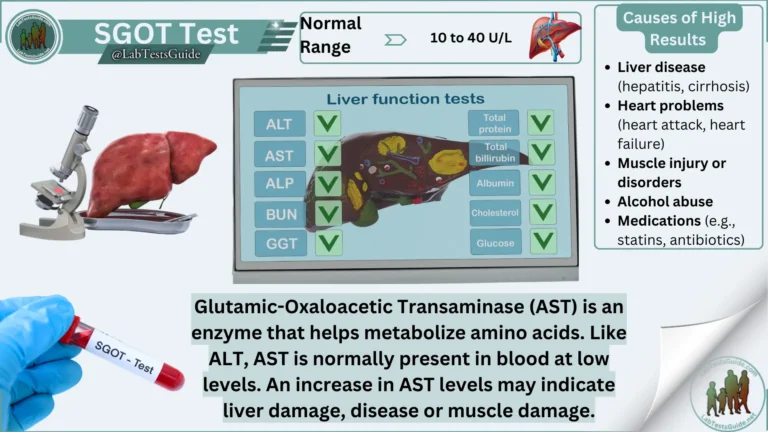
AST (Aspartate Aminotransferase) rises later, around 6–12 hours.
LDH (Lactate Dehydrogenase) peaks even later, around 24–48 hours.
ALT (Alanine Aminotransferase) is primarily a liver enzyme and is not used to detect MI.
14 / 60
Category:
ASCP Exam Questions
The De Ritis ratio (AST/ALT) greater than 2 is indicative of:
The De Ritis ratio (AST/ALT ratio) is a useful clinical marker.
A ratio greater than 2 is classically associated with alcoholic liver disease (ALD) .
In ALD, AST is typically elevated to a greater degree than ALT. This occurs for a few reasons:
Alcohol causes mitochondrial damage, and AST is found in both the cytoplasm and mitochondria, leading to a greater release.
Alcohol consumption can lead to a deficiency of pyridoxal 5′-phosphate (vitamin B6), which is a cofactor for ALT synthesis, disproportionately lowering ALT levels.
Why the other options are incorrect:
a) Viral hepatitis: In acute viral hepatitis, the AST/ALT ratio is usually less than 1 (ALT is higher than AST) in the initial phase.
c) Cirrhosis: While a ratio >1 can be seen in cirrhosis from any cause, a ratio greater than 2 is much more specific for alcoholic etiology.
d) Fatty liver: Non-alcoholic fatty liver disease (NAFLD) typically presents with an AST/ALT ratio less than 1 .
15 / 60
Category:
ASCP Exam Questions
The major plasma protein synthesized by the liver is:
The liver is the primary site of synthesis for most plasma proteins, and albumin is the most abundant one it produces.
Albumin constitutes about 50-60% of total plasma protein. Its main functions are to maintain oncotic pressure (which keeps fluid in the bloodstream) and to transport various substances like hormones, fatty acids, and drugs.
Why the other options are incorrect:
a) Transferrin: While the liver does synthesize transferrin (an iron-transport protein), it is not the most abundant plasma protein produced.
c) Globulin: This is a broad category of proteins, including alpha, beta, and gamma globulins. The liver synthesizes many of them, but the immunoglobulins (gamma globulins) are produced by plasma cells (B lymphocytes), not the liver.
d) Fibrinogen: The liver synthesizes fibrinogen, a crucial protein for blood clotting. However, its plasma concentration is much lower than that of albumin.
16 / 60
Category:
ASCP Exam Questions
A critically ill patient becomes comatose. The physician suspects hepatic failure. The most helpful initial assay is:
In a comatose patient where hepatic failure is suspected, the most urgent concern is hepatic encephalopathy .
A key toxin causing this condition is ammonia , which the failing liver cannot convert to urea.
An ammonia assay provides the most direct and immediate evidence for the cause of the coma (elevated ammonia leading to cerebral toxicity).
While ALT, AST, and GGT are markers of liver injury, they do not directly explain the acute neurological deterioration.
17 / 60
Category:
ASCP Exam Questions
The enzyme most specific for liver cell damage is:
While all these enzymes are associated with the liver, ALT is considered the most specific for damage to the liver cells (hepatocytes).
ALT (Alanine Aminotransferase): This enzyme is primarily found in the cytoplasm of hepatocytes. When liver cells are damaged, ALT is released into the bloodstream. Its concentration is much higher in the liver than in other tissues, making a significant elevation a strong indicator of hepatocellular injury.
Option breakdown:
a) AST (Aspartate Aminotransferase) → Also elevated in liver disease, but less specific because it’s also found in heart and muscle .
b) ALP (Alkaline Phosphatase) → Elevated in biliary obstruction and bone disorders , not specific to liver cells.
c) ALT (Alanine Aminotransferase) → Most specific for hepatocellular injury
d) GGT (Gamma-glutamyl transferase) → Sensitive to biliary disease and alcohol use , but not as specific for liver cell damage.
18 / 60
Category:
ASCP Exam Questions
The most common cause of a falsely increased LD1 fraction on electrophoresis is:
Lactate Dehydrogenase (LD) has five isoenzymes (LD1–LD5).
LD1 and LD2 are most abundant in red blood cells (RBCs) and heart tissue .
When hemolysis occurs (RBCs rupture), LD1 and LD2 are released into the serum, causing a falsely elevated LD1 fraction on electrophoresis.
Option review:
a) Liver disease → Increases LD5 , not LD1.
b) Specimen hemolysis → Releases RBC LD → ↑ LD1 → Correct
c) Congestive heart failure → May cause mild LD increase but not a false LD1 rise.
d) An older specimen → Enzymes may degrade, but this causes decreased , not increased, LD activity.
19 / 60
Category:
ASCP Exam Questions
A patient’s lab results show: Na+ 137 mEq/L, glucose 100 mg/dL, BUN 18 mg/dL, anion gap 19, osmolality 301 mOsm/Kg. This indicates a need to investigate for:
Key values given:
2. Calculate the osmolar gap Measured osmolality = 301Calculated osmolality = 2×Na + (Glucose/18) + (BUN/2.8)286 mOsm/kg
Osmolar gap = Measured – Calculated = 301 – 286 = 15 (normal < 10) → elevated
3. Interpretation
Elevated anion gap → suggests presence of unmeasured anions (like lactate, ketones, toxins).
Elevated osmolar gap → suggests presence of unmeasured osmotically active substances (like methanol, ethanol, ethylene glycol, isopropyl alcohol, acetone).
Combined elevated anion gap + elevated osmolar gap → classic for methanol or ethylene glycol poisoning .
4. Match with options
20 / 60
Category:
ASCP Exam Questions
A patient with a normal BUN and serum creatinine but increased serum and urinary uric acid levels most likely has:
Gout: This condition is characterized by hyperuricemia (increased serum uric acid). The elevated urinary uric acid reflects the kidneys’ attempt to excrete this high load. The key to the question is the normal BUN and serum creatinine . These normal values indicate that overall kidney function is intact, ruling out primary renal failure as the cause of the high uric acid.
Why the other options are incorrect:
a) Dehydration: Dehydration causes a pre-renal state that would elevate both BUN and serum creatinine (with BUN typically rising more prominently). The normal values for these tests rule out dehydration as the primary issue.
c) Nephrotic Syndrome: This condition primarily involves massive proteinuria and low serum albumin. While it can sometimes be associated with altered uric acid levels, the hallmark finding is protein loss, not isolated hyperuricemia with normal kidney function.
d) Renal Failure: In renal failure, the kidneys cannot effectively excrete waste products. This would lead to elevations in BUN, serum creatinine, and uric acid simultaneously. The normal BUN and creatinine directly contradict a diagnosis of renal failure.
21 / 60
Category:
ASCP Exam Questions
In respiratory acidosis, a compensatory mechanism is:
Respiratory acidosis is characterized by a primary increase in blood pCO2 (due to hypoventilation), which leads to a decrease in blood pH.
The body’s main compensatory mechanism is renal compensation :
The kidneys increase the reabsorption of bicarbonate (HCO₃⁻) and the excretion of hydrogen ions.
This increases the plasma bicarbonate concentration, which helps to neutralize the acid and return the pH toward normal.
Why the other options are incorrect:
a) Increased Respiratory Rate: This would be counterproductive. Increasing the respiratory rate would lower pCO2, which is the opposite of what is needed to compensate for a primary respiratory problem. In metabolic acidosis, the lungs compensate by increasing the respiratory rate.
b) Decreased Ammonia Formation: Ammonia (NH₃) in the kidneys is crucial for excreting hydrogen ions (as ammonium, NH₄⁺). In compensation for acidosis, the kidneys increase ammonia formation to get rid of more acid.
c) Increased Blood pCO2: This is the primary cause of respiratory acidosis, not a compensatory mechanism. Compensation works to correct the primary problem.
22 / 60
Category:
ASCP Exam Questions
The primary function of the liver is to:
The liver is a vital organ with hundreds of functions, but its primary and most defining roles are filtration and bile production :
Filter Blood: The liver acts as a processing and detoxification center. It filters blood from the digestive tract, removing toxins, metabolizing drugs, and processing nutrients before they enter the general circulation.
Produce Bile: The liver manufactures bile, which is essential for the digestion and absorption of fats in the small intestine.
Why the other options are incorrect:
a) Regulate blood pressure: While the liver produces angiotensinogen (a precursor in blood pressure regulation), the primary regulators of blood pressure are the heart, blood vessels, and kidneys.
c) Produce insulin: Insulin is produced by the beta cells of the pancreas , not the liver.
d) Store minerals: The liver stores certain vitamins (like A, D, B12) and glycogen, but it is not the primary organ for mineral storage. Minerals are stored in various tissues, notably bones.
23 / 60
Category:
ASCP Exam Questions
A stool specimen that appears black and tarlike should be tested for the presence of:
A black, tarry stool is described as melena . This appearance is caused by the digestion of blood as it passes through the gastrointestinal tract, typically indicating bleeding in the upper GI tract (esophagus, stomach, or duodenum). Therefore, it should be tested for the presence of occult blood (hidden blood), although the bleeding in such cases is often significant enough to be suspected visually.
b) Fecal Fat: This causes stools to be bulky, greasy, and foul-smelling (steatorrhea), not typically black and tarry.
c) Trypsin: This test is used to assess pancreatic function, not for diagnosing bleeding.
d) Excess Mucus: This is associated with inflammation of the intestines (e.g., in colitis or infections) and presents as slimy or stringy stools, not black and tarry.
24 / 60
Category:
ASCP Exam Questions
In the liver, bilirubin is conjugated to form:
In the liver, the enzyme UDP-glucuronosyltransferase conjugates bilirubin with glucuronic acid.
This process forms bilirubin diglucuronide (also known as conjugated bilirubin).
This conjugation makes bilirubin water-soluble, allowing it to be excreted in bile.
The other options are products formed later in the bilirubin metabolism pathway in the intestine.
26 / 60
Category:
ASCP Exam Questions
The creatinine clearance test is used to estimate:
The creatinine clearance test measures how efficiently the kidneys clear creatinine from the blood.
Since creatinine is produced at a nearly constant rate and freely filtered by the glomeruli (with little reabsorption or secretion), its clearance is a good estimate of the Glomerular Filtration Rate (GFR) — a key indicator of kidney function.
Why the other options are incorrect:
a) Liver function: Liver function is assessed by tests like albumin, bilirubin, and liver enzymes (ALT, AST, ALP), not creatinine clearance.
c) Uric acid level: Uric acid is a separate waste product; its level is measured directly in blood or urine, not via a creatinine clearance test.
d) Electrolyte balance: Electrolyte balance (sodium, potassium, etc.) is assessed by measuring their concentrations directly in the blood, not through creatinine clearance.
27 / 60
Category:
ASCP Exam Questions
Azotemia is the medical term for an elevated level of nitrogen-containing compounds (like urea and creatinine) in the blood. It is a laboratory finding that indicates impaired kidney function.
Option breakdown:
a) High blood sugar → Refers to hyperglycemia .
b) High nitrogenous waste in blood → Definition of azotemia.
c) Low urea level → Opposite of azotemia.
d) Increased albumin → Refers to hyperalbuminemia , not azotemia.
30 / 60
Category:
ASCP Exam Questions
In obstructive jaundice, which fraction of bilirubin is predominantly increased?
Obstructive jaundice (also known as post-hepatic jaundice) occurs when there is a blockage in the bile ducts, preventing the flow of bile from the liver to the intestine.
In this condition, the liver cells (hepatocytes) continue to conjugate bilirubin normally.
However, the conjugated (direct) bilirubin cannot be excreted due to the obstruction.
It therefore backs up, regurgitates into the bloodstream, and its levels rise predominantly.
Why the other options are incorrect:
a) Indirect bilirubin: This is the unconjugated fraction. Its production and conjugation are not impaired in a simple obstruction, so it does not predominantly increase.
c) Delta bilirubin: Delta bilirubin is conjugated bilirubin that is covalently bound to albumin. It does increase in obstructive jaundice and is responsible for the prolonged jaundice seen even after an obstruction is relieved because its clearance is slow (it has the half-life of albumin). However, the predominant and initial increase is in free conjugated bilirubin .
d) Both indirect and delta: Indirect bilirubin is not predominantly increased in obstruction. While delta bilirubin increases, the major and primary fraction that rises is conjugated bilirubin.
31 / 60
Category:
ASCP Exam Questions
Kernicterus is an abnormal accumulation of bilirubin in which tissue?
Kernicterus is a neurological condition caused by the deposition of unconjugated bilirubin in the basal ganglia and other areas of the brain .
This typically occurs in newborns with severe, untreated jaundice, as the unconjugated bilirubin is lipid-soluble and can cross the blood-brain barrier.
Accumulation in the brain tissue is neurotoxic and can lead to permanent neurological damage.
32 / 60
Category:
ASCP Exam Questions
The normal blood urea nitrogen (BUN) level (mg/dL) is approximately:
The normal range for blood urea nitrogen (BUN) is typically 7–20 mg/dL in adults. Option b (5–20) is the closest match, as it falls within the standard reference interval used in most clinical settings.
Why the other options are incorrect:
a) 1–5 mg/dL: This is abnormally low and may indicate liver failure (where urea is not produced), overhydration, or a very low-protein diet.
c) 25–40 mg/dL & d) 50–60 mg/dL: These values are elevated (azotemia). They suggest impaired kidney function, dehydration, a high-protein diet, or increased protein breakdown.
33 / 60
Category:
ASCP Exam Questions
A high ALP level with normal AST and ALT suggests:
This pattern of enzyme elevation is a classic clue to differentiate the source of Alkaline Phosphatase (ALP).
Why the other options are incorrect:
a) Hepatocellular damage: This would cause elevated AST and ALT .
c) Alcoholic liver disease: This typically shows an AST:ALT ratio of 2:1 or greater, with both enzymes elevated.
d) Acute hepatitis: This causes a massive elevation in AST and ALT , often into the thousands.
34 / 60
Category:
ASCP Exam Questions
Urea is produced as the end product of:
Here’s the process:
Dietary proteins and the body’s own proteins are broken down into amino acids.
The amino groups (–NH₂) from these amino acids are removed (a process called deamination).
These amino groups are converted into ammonia , which is highly toxic.
The liver detoxifies the ammonia by converting it into urea via the urea cycle .
The urea is then excreted by the kidneys in the urine.
Why the other options are incorrect:
a) Carbohydrate metabolism: The end products of carbohydrate metabolism are carbon dioxide and water.
b) Fat metabolism: The end products of fat metabolism are carbon dioxide, water, and ketone bodies.
d) Nucleic acid metabolism: The breakdown of purines from nucleic acids (like DNA and RNA) produces uric acid , not urea.
35 / 60
Category:
ASCP Exam Questions
Elevated serum uric acid is seen in:
Elevated serum uric acid (hyperuricemia) is the primary cause of gout . It is also commonly seen in renal failure , as the kidneys are responsible for excreting uric acid and impaired function leads to its buildup in the blood.
Option breakdown:
a) Gout and renal failure → Both cause elevated uric acid.
b) Hypoglycemia → Affects glucose, not uric acid.
c) Liver cirrhosis → May lower, not raise, uric acid due to impaired synthesis.
d) Vitamin deficiency → No direct effect on uric acid.
36 / 60
Category:
ASCP Exam Questions
The most common cause of respiratory alkalosis is:
Respiratory alkalosis is defined by a primary decrease in the partial pressure of CO₂ (PaCO₂) in the blood.
Hyperventilation causes excessive exhalation of CO₂, leading to a fall in PaCO₂ and a rise in blood pH.
This is the direct and most common mechanism for respiratory alkalosis.
Vomiting (a) causes metabolic alkalosis. Starvation (b) can cause metabolic acidosis. Asthma (c) typically causes respiratory acidosis due to impaired gas exchange.
37 / 60
Category:
ASCP Exam Questions
Which enzyme is most sensitive for detecting cholestasis?
Cholestasis is a condition where the flow of bile from the liver is reduced or blocked.
GGT is highly concentrated in the epithelial cells lining the bile ducts. When bile flow is obstructed, these cells are stimulated to produce more GGT, and the enzyme is released into the bloodstream. This makes GGT an extremely sensitive marker for detecting cholestasis and biliary tract disease.
Why the other options are less sensitive for cholestasis:
a) AST (Aspartate Aminotransferase): This enzyme is more specific for general hepatocellular injury (damage to liver cells) rather than specifically for bile duct obstruction.
c) LDH (Lactate Dehydrogenase): LDH is a very non-specific enzyme found in many tissues (heart, liver, red blood cells, muscle). An elevation is not specific to the liver, let alone to cholestasis.
d) ALT (Alanine Aminotransferase): Like AST, ALT is a marker of hepatocellular injury. While it may be elevated in cholestasis, it is not the most sensitive or primary indicator.
38 / 60
Category:
ASCP Exam Questions
The normal reference range for serum creatinine in adults (mg/dL) is approximately:
This is the standard reference range for serum creatinine in healthy adults. However, it’s important to note some nuances:
The range can vary slightly between different laboratories.
Sex Difference: Due to higher average muscle mass, the normal range for adult males is typically around 0.7–1.3 mg/dL , while for adult females it is typically around 0.6–1.1 mg/dL .
Values outside this range can indicate impaired kidney function, with rising levels suggesting a decrease in the glomerular filtration rate (GFR).
Why the other options are incorrect:
a) 0.1–0.5 mg/dL: This is too low and would be unusual for a healthy adult. It might be seen in individuals with very low muscle mass (e.g., elderly, cachexic).
c) 1.5–2.5 mg/dL & d) 2.5–4.0 mg/dL: These values are elevated and indicate renal impairment (azotemia). Values in these ranges suggest moderate to severe kidney dysfunction.
39 / 60
Category:
ASCP Exam Questions
A low urine specific gravity indicates:
Urine specific gravity measures the density of urine compared to water. A low value means the urine is less concentrated, or dilute , because it contains more water and fewer dissolved particles like salts and waste products.
Option breakdown:
a) Concentrated urine → Has high , not low, SG.
b) Dilute urine → Correct — indicates low solute concentration.
c) Dehydration → Causes high , not low, SG.
d) Glycosuria → Increases SG (due to glucose in urine).
40 / 60
Category:
ASCP Exam Questions
Creatinine is formed from:
Here is the process:
Creatine is synthesized in the liver and transported to muscles.
In muscle cells, it is phosphorylated to form creatine phosphate , which serves as a rapid, short-term energy reserve.
Creatine phosphate spontaneously and irreversibly cyclizes to form creatinine at a relatively constant rate, proportional to an individual’s muscle mass.
Creatinine is released into the blood and filtered by the kidneys for excretion in urine.
Because its production is constant and it is freely filtered by the kidneys, it is a key marker for assessing kidney function.
Why the other options are incorrect:
b) Amino acids: Amino acids are the building blocks for creatine itself, but creatinine is specifically the breakdown product of creatine phosphate.
c) Glucose: Glucose is involved in energy metabolism but is not a precursor for creatinine.
d) Fatty acids: Fatty acids are broken down for energy but are not involved in creatinine formation.
41 / 60
Category:
ASCP Exam Questions
A blood creatinine value of 5.0 mg/dL is most likely to be found with which of the following blood values?
A creatinine level of 5.0 mg/dL indicates severely impaired kidney function (severe azotemia).
Urea nitrogen (BUN) is also a nitrogenous waste product that accumulates when the glomerular filtration rate (GFR) falls.
A BUN of 80 mg/dL is also severely elevated and is a classic finding that accompanies a high creatinine level in renal failure.
The other values can be abnormal in various conditions, but the combination of high creatinine and high BUN is the hallmark of uremia/renal failure.
42 / 60
Category:
ASCP Exam Questions
Which of the following enzyme patterns is most consistent with obstructive jaundice?
Obstructive jaundice (cholestasis) → impaired bile flow → increased alkaline phosphatase (ALP) and gamma-glutamyl transferase (GGT) due to bile duct epithelial cell irritation and increased synthesis.
ALT and AST (transaminases) are markers of hepatocyte injury; they are only mildly elevated in obstruction unless there is secondary hepatic inflammation.
Option b fits the classic “cholestatic pattern”: ALP ↑↑, GGT ↑↑, transaminases ↑ (mild) .
Other options:
a → suggests hepatocellular injury (e.g., viral hepatitis).
c → also more consistent with hepatocellular injury.
d → isolated AST rise can occur in alcohol use, muscle injury, etc., not typical for obstructive jaundice.
43 / 60
Category:
ASCP Exam Questions
The different forms of hemoglobin (e.g., HbA, HbS) can be separated and identified based on their charge using:
Hemoglobin variants like HbA (normal adult hemoglobin), HbS (sickle cell hemoglobin), HbC, and HbF differ slightly in their amino acid composition. These amino acid changes often alter the electrical charge of the hemoglobin molecule.
Why the other options are incorrect:
a) Immunoassay: This method uses antibodies to detect specific antigens. While there are immunoassays for hemoglobin (like in fecal occult blood tests), they are not used to separate and distinguish between the different charge-based variants like HbA and HbS.
c) Mass Spectrometry: This technique separates molecules based on their mass-to-charge ratio. While it can identify hemoglobin variants and is increasingly used, the classic and most widely used method for initial separation based on charge is electrophoresis.
d) Ion-Selective Electrode: This is used to measure the concentration of specific ions (like sodium, potassium, or chloride) in a solution, not to separate different forms of a protein like hemoglobin.
44 / 60
Category:
ASCP Exam Questions
Which test is used to measure total bilirubin?
The Jendrassik–Grof method is the standard and most widely used photometric method for measuring total and direct bilirubin in serum. It uses a diazo reagent to react with bilirubin, and the intensity of the colored product formed is measured.
Why the other options are incorrect:
b) Biuret method: This is used to measure total serum protein .
c) Bromocresol green method: This is a common dye-binding method used to measure serum albumin .
d) Kjeldahl method: This is a classic, but older and more complex, method for determining the nitrogen content in a sample, which can be used to calculate protein content. It is not used for routine bilirubin testing.
45 / 60
Category:
ASCP Exam Questions
The major nitrogenous waste product in urine is:
Urea is the primary end product of protein and amino acid metabolism in humans. It is produced in the liver via the urea cycle and is the mechanism for excreting the majority of nitrogenous waste.
Why the other options are incorrect:
a) Creatine: Creatine is a compound used for energy storage in muscles, not a major waste product. Its waste product is creatinine , which is the second most abundant nitrogenous waste in urine but in much smaller quantities than urea.
b) Uric acid: Uric acid is a waste product from the breakdown of purines (from nucleic acids). It is present in urine but in significantly lower amounts than urea.
d) Ammonia: While some ammonia is excreted in the urine to help regulate pH, it is a minor component compared to urea. Most ammonia is converted to urea in the liver first.
46 / 60
Category:
ASCP Exam Questions
In which of the following disease states is conjugated (direct) bilirubin a major serum component?
Conjugated (Direct) Bilirubin is the water-soluble form of bilirubin that has been processed by the liver. It is normally excreted into the bile and then into the intestines.
In Biliary Obstruction (e.g., from a gallstone or tumor), the flow of bile from the liver to the intestines is blocked. This causes the conjugated bilirubin to back up into the bloodstream, making it the major serum component.
Why the other options are incorrect:
a) Hemolysis : This causes an unconjugated (indirect) bilirubin increase because the liver is overwhelmed by the breakdown products of red blood cells and cannot conjugate it fast enough.
b) Neonatal Jaundice : This is primarily due to the immature liver’s inability to conjugate bilirubin rapidly, leading to high levels of unconjugated bilirubin .
d) Erythroblastosis Fetalis : This is a severe form of hemolytic disease in newborns, so the major bilirubin component is also unconjugated .
47 / 60
Category:
ASCP Exam Questions
Which of the following tests best assesses tubular function?
Urine osmolality directly measures the concentration of particles in the urine. The kidney’s tubules are responsible for concentrating and diluting urine, so this test is a direct assessment of the tubules’ concentrating ability .
Option breakdown:
a) Creatinine clearance → Assesses glomerular filtration rate (GFR) → tests glomerular function , not tubular.
b) Urine osmolality → Best indicator of tubular function (ability to concentrate urine).
c) Bilirubin test → Evaluates liver function , unrelated to kidneys.
d) Serum ALP (alkaline phosphatase) → Reflects liver or bone activity , not renal function.
48 / 60
Category:
ASCP Exam Questions
The conjugation of bilirubin occurs in the:
Unconjugated (indirect) bilirubin is produced from the breakdown of hemoglobin in the spleen and transported to the liver bound to albumin.
In the liver , bilirubin is conjugated with glucuronic acid by the enzyme UDP-glucuronyl transferase , forming conjugated (direct) bilirubin .
This conjugated bilirubin is water-soluble and excreted into bile .
Option breakdown:
a) Spleen → Site of RBC breakdown (production of unconjugated bilirubin).
b) Liver → Site of bilirubin conjugation .
c) Kidney → Excretes conjugated bilirubin derivatives (e.g., urobilinogen).
d) Bone marrow → Site of RBC production, not bilirubin metabolism.
49 / 60
Category:
ASCP Exam Questions
The expected blood gas results for a patient in chronic renal failure would match the pattern of:
Chronic Renal Failure impairs the kidneys’ ability to excrete acid (specifically hydrogen ions, H⁺) and regenerate bicarbonate (HCO₃⁻). This leads to a buildup of acid in the blood.
Metabolic Acidosis is defined by a primary decrease in serum bicarbonate (HCO₃⁻) and a low blood pH (< 7.35). The body may attempt to compensate through hyperventilation (blowing off CO₂), leading to a lower partial pressure of carbon dioxide (PaCO₂).
The other options are incorrect because:
b) Respiratory Acidosis is caused by impaired gas exchange and CO₂ retention (e.g., in lung disease).
c) Metabolic Alkalosis is caused by a primary loss of acid or gain of bicarbonate (e.g., from vomiting).
d) Respiratory Alkalosis is caused by hyperventilation and excessive loss of CO₂ (e.g., due to anxiety or pain).
50 / 60
Category:
ASCP Exam Questions
An increased BUN and creatinine level is typically seen in:
An increase in both Blood Urea Nitrogen (BUN) and creatinine is the classic laboratory finding for renal failure (kidney failure).
The kidneys are responsible for filtering and excreting these waste products.
When kidney function declines, both BUN and creatinine accumulate in the blood.
Why the other options are incorrect:
a) Liver failure: The liver produces urea. In liver failure, BUN is often decreased or normal because the liver cannot synthesize urea, even though creatinine levels remain normal (as it is not dependent on the liver).
c) Hypoglycemia: This is related to blood glucose levels and has no direct, consistent effect on BUN or creatinine.
d) Dehydration only: Dehydration can cause a pre-renal azotemia , leading to an increased BUN and a lesser increase in creatinine (often with a high BUN:creatinine ratio, >20:1).
51 / 60
Category:
ASCP Exam Questions
The most widely used method for bilirubin measurement is based on the:
Here is why the other options are incorrect:
a) Jaffe Reaction: This method is used for the measurement of creatinine , not bilirubin.
b) Schales and Schales Method: This is a specific titration method used for measuring chloride levels.
c) 8-Hydroxyquinoline Reaction: This is not a standard method for bilirubin. 8-Hydroxyquinoline is sometimes used in methods for measuring magnesium .
54 / 60
Category:
ASCP Exam Questions
Which of the following is used as a marker of early renal damage in diabetes?
Microalbuminuria (small amounts of albumin in the urine that are undetectable by standard dipstick) is the earliest clinical sign of diabetic nephropathy (kidney damage). Detecting it allows for early intervention to prevent progression to overt kidney disease.
a) Total protein → Detects larger protein losses seen in advanced kidney disease, not early damage.
b) Microalbuminuria → Earliest indicator of diabetic renal damage.
c) Uric acid → Related to purine metabolism and gout, not diabetic nephropathy.
d) BUN → Rises in later stages of kidney failure, not early damage.
55 / 60
Category:
ASCP Exam Questions
Hypoalbuminemia is most commonly associated with:
Hypoalbuminemia means a low level of albumin in the blood. The two most common pathological causes are:
Liver Disease: The liver is the sole site of albumin synthesis. In chronic liver diseases like cirrhosis, the damaged liver cannot produce enough albumin.
Nephrotic Syndrome: This is a kidney disorder where the glomeruli are damaged, leading to massive loss of protein, including albumin, in the urine (proteinuria).
Why the other options are incorrect:
a) Dehydration: Dehydration causes hemoconcentration , which would lead to a falsely elevated or normal albumin level, not a low one.
c) Hemolysis: Hemolysis is the rupture of red blood cells. It does not directly cause a decrease in albumin synthesis or lead to its loss.
d) Polycythemia: This is an increased number of red blood cells. Like dehydration, it can cause hemoconcentration and a relative increase in albumin concentration, not a decrease.
56 / 60
Category:
ASCP Exam Questions
The Jaffe reaction is used to measure creatinine and involves the reaction with:
The Jaffe reaction is a colorimetric method used to measure creatinine in blood and urine. In this reaction, creatinine reacts with alkaline picrate to form a red-orange complex , the intensity of which can be measured spectrophotometrically — typically around 520 nm .
Reaction summary:
Creatinine+Alkaline Picrate→Red-Orange Complex\text{Creatinine} + \text{Alkaline Picrate} \rightarrow \text{Red-Orange Complex} Creatinine + Alkaline Picrate → Red-Orange Complex
Other options (for comparison):
(b) Diazotized Sulfanilic Acid → used in Griess reaction (for nitrite detection).
(c) Paradimethylaminobenzaldehyde (Ehrlich’s reagent) → used for urobilinogen detection.
(d) Cupric Sulfate → used in Biuret test for proteins .
57 / 60
Category:
ASCP Exam Questions
The most important buffer system in the blood is:
The bicarbonate buffer system (H₂CO₃ / HCO₃⁻) is the most important and effective buffer system in the blood .
It maintains physiological pH (~7.4) by balancing carbonic acid (H₂CO₃) and bicarbonate (HCO₃⁻) .
It also works in close coordination with the respiratory system (which controls CO₂) and the renal system (which regulates HCO₃⁻).
Option breakdown:
a) Phosphate buffer system → Important in urine and intracellular fluid , not the main blood buffer.
b) Bicarbonate buffer system → Primary blood buffer system →
c) Protein buffer system → Plays a role, especially intracellularly, but less significant in plasma.
d) Hemoglobin buffer system → Important in red blood cells, but overall less dominant than bicarbonate
58 / 60
Category:
ASCP Exam Questions
Bilirubin is produced from the breakdown of:
Bilirubin is a yellow-orange pigment that is the primary waste product of the normal breakdown of heme.
Approximately 80-85% of bilirubin comes from the breakdown of hemoglobin from senescent (old) red blood cells, which are destroyed by macrophages in the reticuloendothelial system (spleen, liver, bone marrow).
The heme portion of hemoglobin is converted to biliverdin and then to unconjugated bilirubin .
Why the other options are incorrect:
b) Albumin: Albumin is a blood plasma protein that transports unconjugated bilirubin in the bloodstream; it is not the source of bilirubin.
c) Creatinine: Creatinine is a waste product from the breakdown of creatine phosphate in muscle tissue.
d) Urea: Urea is the primary waste product formed from the breakdown of proteins and amino acids in the liver.
59 / 60
Category:
ASCP Exam Questions
Conjugated bilirubin is also known as:
Conjugated bilirubin is bilirubin that has been processed in the liver , where it is joined (conjugated) with glucuronic acid by the enzyme UDP-glucuronyl transferase .
This makes it water-soluble and able to be excreted in bile and urine .
In laboratory testing, it reacts directly with the diazo reagent — hence the name “direct bilirubin.”
Option breakdown:
a) Indirect bilirubin → = Unconjugated bilirubin (not yet processed by the liver).
b) Unconjugated bilirubin → Same as above.
c) Direct bilirubin → Conjugated form
d) Total bilirubin → = Direct + Indirect bilirubin.
60 / 60
Category:
ASCP Exam Questions
A patient has the following lab results: total bilirubin 9.5 mg/dL, unconjugated bilirubin 8.5 mg/dL, urine bilirubin negative, urine urobilinogen increased. This jaundice is classified as:
High unconjugated bilirubin (8.5 mg/dL out of 9.5 total) → not water-soluble, so urine bilirubin is negative .
Increased urine urobilinogen → indicates increased hemoglobin breakdown (e.g., hemolysis) and normal liver conjugation with increased enterohepatic circulation.
This pattern (unconjugated hyperbilirubinemia, no bilirubin in urine, high urobilinogen) is characteristic of prehepatic jaundice (e.g., hemolytic anemia).
Your score is
The average score is 63%
Follow us on Sicial Media:
Restart quiz
Top 8 Medical Laboratory Scientist (MLS) Exams: Top 8 Medical Laboratory Scientist (MLS) Exams that are recognized globally and can help professionals validate their credentials and enhance their career opportunities:
1. ASCP – American Society for Clinical Pathology (USA) Exam Name: MLS(ASCP)Eligibility: Bachelor’s degree with clinical laboratory experience.Global Recognition: HighPurpose: Certifies Medical Laboratory Scientists in the United States and internationally.2. AMT – American Medical Technologists (USA) Exam Name: MLT(AMT) or MT(AMT)Eligibility: Academic and/or work experience in medical laboratory technology.Global Recognition: ModeratePurpose: Credentialing for medical technologists and technicians.3. AIMS – Australian Institute of Medical and Clinical Scientists Exam Name: AIMS Certification ExamEligibility: Assessment of qualifications and work experience.Recognition: Required for practice in Australia.Purpose: Certification and registration in Australia.4. CSMLS – Canadian Society for Medical Laboratory Science Exam Name: CSMLS General or Subject-specific ExamsEligibility: Graduation from a CSMLS-accredited program or equivalent.Recognition: CanadaPurpose: Entry-to-practice certification in Canada.5. IBMS – Institute of Biomedical Science (UK) Exam Name: Registration and Specialist Portfolio AssessmentEligibility: Accredited degree and lab experience.Recognition: UK and some Commonwealth countries.Purpose: Biomedical Scientist registration with the HCPC (UK).6. HAAD / DOH – Department of Health, Abu Dhabi (UAE) Exam Name: DOH/HAAD License ExamEligibility: Degree in medical laboratory science and experience.Recognition: UAE (Abu Dhabi)Purpose: Licensure for medical laboratory practice in Abu Dhabi.7. DHA – Dubai Health Authority (UAE) Exam Name: DHA License Exam for Medical Laboratory TechnologistsEligibility: Relevant degree and experience.Recognition: Dubai, UAEPurpose: Professional license for clinical laboratory practice in Dubai.8. MOH – Ministry of Health (Gulf Countries like UAE, Saudi Arabia, Kuwait) Exam Name: MOH License ExamEligibility: BSc/Diploma in Medical Laboratory + experience.Recognition: Varies by country.Purpose: Required for practicing in public and private sector labs.Tags:
Possible References Used