Free ASCP MLS Exam Practice Questions: Part 45 covers 60 MCQs (3641 – 3700) on coagulation testing. Topics include PT, aPTT, INR, mixing studies, factor assays, fibrinogen assays, thrombin time, D-dimer, and lupus anticoagulant testing. Strengthen your knowledge of coagulation diagnostics.
Report a question
ASCP MLS Exam MCQs Chapter 45
Why Take This Mock Test? Strengthens exam confidence Highlights areas for improvement Provides practice with clinically relevant scenarios This mock test (60 MCQs (3641 – 3700) ) is part of our ongoing ASCP MLS Exam Practice Series , giving you structured preparation for all major immunology topics.
Our Coagulation Testing (PT, aPTT, Factor Assays, Special Studies) Mock Test is specifically designed for candidates appearing in ASCP MLS, AMT MLT/MT, AIMS, CSMLS, IBMS, HAAD/DOH, DHA, and MOH exams. This mock test mirrors the structure, difficulty level, and question style you can expect in the actual examination.
Take this test to:ASCP MLS Exam .
Who Should Use This Mock Test? Medical Laboratory Scientists and Technicians
Pathology Students
Professionals preparing for international laboratory certification exams
Anyone seeking to strengthen their knowledge of Coagulation Testing (PT, aPTT, Factor Assays, Special Studies)
How to Use This Mock Test Effectively Simulate Exam Conditions: Attempt the test in one sitting without referring to notes.
Track Your Time: Keep within the allotted time limit to build speed.
Review Explanations: Study the answer explanations to strengthen understanding.
Repeat for Retention: Re-attempt after revision to measure improvement.
1 / 60
Category:
ASCP Exam Questions
If a prolonged aPTT does not correct after mixing study, the cause is most likely:
If a prolonged aPTT does not correct after mixing with normal plasma, it indicates the presence of an inhibitor .
Common inhibitors include:
Lupus anticoagulant (an antiphospholipid antibody)
Specific factor inhibitors (e.g., antibodies against Factor VIII, IX, etc.)
These inhibitors interfere with coagulation factors or phospholipids, preventing normalization even when factors are supplied by normal plasma.
Other options:
a) Factor deficiency → would correct with mixing.
c) Vitamin K deficiency → would show correction in mixing studies (if tested via PT/aPTT).
d) Platelet dysfunction → does not affect aPTT.
3 / 60
Category:
ASCP Exam Questions
Reptilase time differs from thrombin time because:
Reptilase time uses an enzyme from snake venom that converts fibrinogen to fibrin, similar to thrombin.
The key difference is that reptilase is not inhibited by heparin (or antithrombin), whereas thrombin is strongly inhibited by heparin .
This makes reptilase time useful for identifying whether a prolonged thrombin time is due to heparin or other causes (e.g., hypofibrinogenemia, dysfibrinogenemia).
Other options:
b) Incorrect — Reptilase time is not necessarily faster; it depends on the fibrinogen level and presence of inhibitors.
c) Incorrect — It does not require platelet factor 3.
d) Incorrect — Reptilase time, like thrombin time, does not require calcium for fibrin formation.
4 / 60
Category:
ASCP Exam Questions
Chromogenic factor assays measure:
Chromogenic assays measure the activity of specific coagulation factors (e.g., Factor VIII, Factor IX, antithrombin, Protein C) by using synthetic chromogenic substrates that release a colored compound (measured photometrically) when cleaved by the target enzyme.
These assays are based on enzymatic reactions rather than clot formation, providing precise and specific factor activity levels.
Other options:
a) Cell granularity → analyzed by flow cytometry or microscopy.
c) Platelet aggregation → measured by platelet function analyzers or aggregometry.
d) Hemoglobin electrophoresis → used to identify hemoglobin variants.
5 / 60
Category:
ASCP Exam Questions
The test used to confirm the presence of Heparin-Induced Thrombocytopenia (HIT) antibodies is:
The serotonin release assay (SRA) is considered the gold standard for confirming HIT.
It is a functional test that detects heparin-dependent platelet-activating antibodies.
In this test, patient serum is mixed with donor platelets loaded with radioactive serotonin; if HIT antibodies are present, heparin induces platelet activation and serotonin release.
Other options:
b) Anti-Factor Xa assay → measures heparin level, not HIT antibodies.
c) D-dimer → indicates fibrin degradation, not specific to HIT.
d) Fibrinogen level → measures fibrinogen concentration, not related to HIT diagnosis.
6 / 60
Category:
ASCP Exam Questions
If a prolonged aPTT corrects after mixing study, the cause is most likely:
If a prolonged aPTT corrects (normalizes) immediately after mixing patient plasma with normal pooled plasma, it indicates a factor deficiency .
The normal plasma supplies the missing clotting factor, allowing the coagulation cascade to proceed normally.
Other options:
a) Lupus anticoagulant → typically shows no correction in mixing studies (inhibitor presence).
b) Specific factor inhibitor (e.g., Factor VIII antibody) → usually shows no correction or partial correction that reverses after incubation.
d) Vitamin K deficiency → would affect PT more prominently and show correction in mixing studies for the deficient factors, but the question focuses on aPTT correction.
7 / 60
Category:
ASCP Exam Questions
Which coagulation test is most sensitive to fibrinogen deficiency?
The thrombin time (TT) directly measures the conversion of fibrinogen to fibrin after adding exogenous thrombin.
It is the most sensitive to fibrinogen deficiency or dysfunction because it bypasses all earlier steps in the coagulation cascade and depends solely on fibrinogen levels and function.
Even mild reductions in fibrinogen (hypofibrinogenemia) or qualitative defects (dysfibrinogenemia) will prolong the TT.
Other options:
a) PT and b) aPTT — are affected by fibrinogen deficiency only when levels are severely reduced (<100 mg/dL), as they involve multiple coagulation factors and pathways.
d) dRVVT — used for lupus anticoagulant detection, not sensitive to isolated fibrinogen deficiency.
8 / 60
Category:
ASCP Exam Questions
The Thrombin Time (TT) test measures the final step of the coagulation cascade, which is:
The Thrombin Time (TT) test directly measures the functionality of the final common step of the coagulation cascade.
The test works by adding thrombin directly to the patient’s plasma.
This bypasses the entire intrinsic, extrinsic, and common pathways.
Thrombin’s job is to convert the soluble plasma protein fibrinogen into insoluble fibrin strands to form the clot.
Therefore, a prolonged TT indicates a problem in this specific reaction, such as low fibrinogen, abnormal fibrinogen (dysfibrinogenemia), or the presence of inhibitors like heparin.
10 / 60
Category:
ASCP Exam Questions
Activated partial thromboplastin time (aPTT) primarily evaluates which pathway?
The activated partial thromboplastin time (aPTT) test primarily evaluates the intrinsic pathway (Factors XII, XI, IX, VIII) and the common pathway (Factors X, V, II, and fibrinogen).
It is performed by adding an activator (e.g., kaolin, silica), phospholipid, and calcium to citrated plasma, then measuring the time to clot formation.
Other options:
b) Extrinsic only → evaluated by PT.
c) Platelet function → evaluated by bleeding time or platelet function assays.
d) Fibrinolysis → evaluated by D-dimer, FDP, or euglobulin lysis time.
11 / 60
Category:
ASCP Exam Questions
The PFA-100 (Platelet Function Analyzer) is used to assess:
The PFA-100 is a tool that simulates the conditions of a small vessel injury. It measures how long it takes for a platelet plug to form and occlude an aperture in a membrane coated with agonists (like collagen and ADP or epinephrine). This process is the core of primary hemostasis . It is a global screening test for platelet function and von Willebrand factor activity.
a) is incorrect because specific coagulation factor levels are measured by assays like PT, aPTT, and individual factor tests.
c) is incorrect because fibrinolytic system activity is assessed by tests like D-dimer, fibrin degradation products, or euglobulin lysis time.
d) is incorrect because circulating anticoagulants (e.g., lupus anticoagulant) are typically detected using specific phospholipid-dependent clotting tests.
12 / 60
Category:
ASCP Exam Questions
In a patient with a suspected bleeding disorder, a normal PT and aPTT would most likely rule out a deficiency in which of the following?
PT tests the extrinsic and common pathways (Factors VII, X, V, II, fibrinogen).
aPTT tests the intrinsic and common pathways (Factors XII, XI, IX, VIII, X, V, II, fibrinogen).
If both PT and aPTT are normal , it means there are no significant deficiencies in the intrinsic, extrinsic, or common pathway factors.
Other options:
a) Factor VIII — Would prolong aPTT, so a normal aPTT largely rules out a severe Factor VIII deficiency.
b) Factor XIII — Not detected by PT or aPTT, so a deficiency would still be possible.
c) Vitamin K dependent factors — Would prolong PT (and possibly aPTT), so a normal PT makes a severe deficiency unlikely.
13 / 60
Category:
ASCP Exam Questions
Which factor deficiency leads to prolonged clotting but no bleeding symptoms?
Factor XII (Hageman factor) deficiency causes a marked prolongation of the aPTT but is not associated with clinical bleeding .
This is because Factor XII is involved in the contact activation pathway in vitro, but it is not essential for in vivo hemostasis.
In fact, Factor XII deficiency may even be associated with a thrombotic tendency in some cases.
Other options:
a) Factor VIII deficiency (Hemophilia A) → causes bleeding.
b) Factor IX deficiency (Hemophilia B) → causes bleeding.
d) Factor VII deficiency → causes bleeding (prolonged PT).
14 / 60
Category:
ASCP Exam Questions
Which condition prolongs aPTT but not PT?
aPTT is sensitive to deficiencies in the intrinsic pathway (Factors XII, XI, IX, VIII) and common pathway.
PT is sensitive to deficiencies in the extrinsic pathway (Factor VII) and common pathway.
Factor VIII deficiency (Hemophilia A) affects the intrinsic pathway, so it prolongs aPTT but PT remains normal .
Other options:
b) Factor VII deficiency → prolongs PT, aPTT normal.
c) Vitamin K deficiency → affects Factors II, VII, IX, X → prolongs both PT and aPTT (PT affected first/more).
d) Warfarin therapy → causes vitamin K antagonist effect → prolongs PT (and often aPTT later).
15 / 60
Category:
ASCP Exam Questions
Which reagent is required in PT testing?
Other options:
b) Platelet-rich plasma → used in platelet function tests, not PT.
c) Kaolin and phospholipid → used in aPTT (activates the intrinsic pathway).
d) Collagen → used in platelet aggregation studies.
16 / 60
Category:
ASCP Exam Questions
Which condition prolongs both PT and aPTT?
Liver disease often leads to decreased production of multiple coagulation factors (II, V, VII, IX, X, XI, fibrinogen), affecting both the extrinsic and intrinsic pathways .
This results in prolongation of both PT and aPTT .
Other options:
a) Hemophilia A (Factor VIII deficiency) → prolongs aPTT only.
c) Factor VII deficiency → prolongs PT only.
d) von Willebrand disease → primarily affects platelet function and may prolong bleeding time, but PT and aPTT are typically normal.
17 / 60
Category:
ASCP Exam Questions
The test used to screen for the Lupus Anticoagulant (LA) is typically a(n):
Lupus Anticoagulant (LA) is an antiphospholipid antibody that acts as an inhibitor in vitro .
It interferes with phospholipid-dependent clotting tests, most commonly causing a prolonged aPTT .
When a mixing study is performed, the inhibitor prevents the normal plasma from correcting the prolonged time, so the aPTT does not correct .
This pattern (prolonged phospholipid-dependent test that fails to correct on mixing) is a key initial screening step for detecting Lupus Anticoagulant.
18 / 60
Category:
ASCP Exam Questions
Hemophilia A is caused by a deficiency of which coagulation factor?
Hemophilia A, also known as classic hemophilia, is a well-characterized X-linked recessive bleeding disorder.
It is caused by a deficiency or dysfunction of Factor VIII .
This deficiency impairs the intrinsic pathway of the coagulation cascade.
The hallmark laboratory finding is a prolonged Activated Partial Thromboplastin Time (aPTT) , while the Prothrombin Time (PT) remains normal.
19 / 60
Category:
ASCP Exam Questions
Prothrombin time (PT) primarily evaluates which pathway?
The prothrombin time (PT) test primarily evaluates the extrinsic pathway (via Factor VII) and the common pathway (Factors X, V, II, and fibrinogen).
It is performed by adding tissue factor (thromboplastin) and calcium to citrated plasma and measuring the time to clot formation.
Other options:
a) Intrinsic pathway → evaluated by aPTT.
c) Fibrinolytic pathway → evaluated by tests like D-dimer, FDP.
d) Platelet adhesion → evaluated by bleeding time or platelet function assays.
23 / 60
Category:
ASCP Exam Questions
A patient with liver disease would most likely exhibit:
The liver is the primary site of synthesis for almost all coagulation factors (except Factor VIII, which is also produced in vascular endothelium).
In liver disease, the synthesis of these factors is impaired.
Since both the Prothrombin Time (PT) and Activated Partial Thromboplastin Time (aPTT) tests depend on multiple coagulation factors produced in the liver, both tests are typically prolonged .
The PT is often prolonged first and is more sensitive, as Factor VII (part of the PT pathway) has the shortest half-life. However, as liver synthetic function declines, the aPTT will also become abnormal.
24 / 60
Category:
ASCP Exam Questions
Factor IX assays are important for diagnosis of:
Factor IX assays measure the activity level of Factor IX in plasma.
Deficiency of Factor IX causes Hemophilia B (also known as Christmas disease), an X-linked recessive bleeding disorder.
Diagnosis is confirmed by demonstrating reduced Factor IX activity.
Other options:
a) Hemophilia A → caused by Factor VIII deficiency.
c) von Willebrand disease → involves deficiency or dysfunction of von Willebrand factor.
d) Factor VII deficiency → causes prolonged PT, not related to Factor IX.
25 / 60
Category:
ASCP Exam Questions
A patient on warfarin (Coumadin) therapy would be expected to have a prolonged:
Warfarin (Coumadin) is a vitamin K antagonist. It works by inhibiting the synthesis of vitamin K-dependent clotting factors, which include Factor II, VII, IX, and X .
The Prothrombin Time (PT) test is specifically sensitive to deficiencies in Factors VII (Extrinsic Pathway), X, II, and Fibrinogen (Common Pathway).
Since warfarin affects several of these factors (especially Factor VII, which has the shortest half-life), it prolongs the PT .
The PT/INR (International Normalized Ratio) is the standard test used to monitor warfarin therapy.
26 / 60
Category:
ASCP Exam Questions
Which reagent is required in aPTT testing?
Other options:
a) Tissue factor → used in PT testing, not aPTT.
c) Platelet-rich plasma only → used in platelet function tests.
d) D-dimer reagent → used in D-dimer immunoassays, not aPTT.
27 / 60
Category:
ASCP Exam Questions
The INR (International Normalized Ratio) is used to monitor therapy with:
The INR (International Normalized Ratio) was developed to standardize prothrombin time (PT) results across different laboratories and thromboplastin reagents.
It is the primary test used to monitor warfarin (vitamin K antagonist) therapy .
The formula is:
INR=(Patient PTMean Normal PT)ISI INR = ( Mean Normal PT Patient PT ) ISI
where ISI = International Sensitivity Index of the thromboplastin used.
Other options:
a) Heparin → monitored by aPTT or anti-Factor Xa assay.
c) Aspirin → monitored by platelet function tests (not INR).
d) Direct Xa inhibitors → monitored by specific anti-Factor Xa assays (not INR).
28 / 60
Category:
ASCP Exam Questions
In the coagulation cascade, calcium ions are required for:
Calcium ions (Ca²⁺) act as a cofactor that enables coagulation factors (especially in the tenase and prothrombinase complexes) to bind to phospholipid surfaces (e.g., platelet membranes).
This binding is essential for efficient coagulation complex assembly and thrombin generation.
Other options:
a) Factor XII activation occurs through contact activation and does not require calcium specifically.
b) Vitamin K binds to its dependent factors during their synthesis in the liver, not in a calcium-dependent manner; calcium is needed for the function of these factors, not the binding of vitamin K.
d) Protein C activation by thrombin-thrombomodulin is actually enhanced by calcium, but calcium does not inhibit Protein C.
29 / 60
Category:
ASCP Exam Questions
Which coagulation test uses optical density to measure clot formation?
The photo-optical (or photometric) method measures clot formation by detecting changes in optical density (turbidity) as fibrin strands form in plasma.
As clotting occurs, the sample changes from clear to turbid, and this change in light transmission or scattering is recorded.
Other options:
a) Mechanical clot detection → uses physical movement of a ball or probe to detect clot formation.
c) Chromogenic substrate assay → measures color release from a synthetic substrate by enzyme activity (e.g., Factor Xa or thrombin), not clot formation.
d) Flow cytometry → used for cell analysis (e.g., immunophenotyping), not coagulation testing.
30 / 60
Category:
ASCP Exam Questions
A prolonged Prothrombin Time (PT) and a normal Activated Partial Thromboplastin Time (aPTT) is most suggestive of a deficiency in which factor?
This pattern occurs because of how the coagulation tests are designed:
The PT is initiated by Tissue Factor and is sensitive to the Extrinsic Pathway (Factor VII) and the Common Pathway .
The aPTT is initiated by contact activation and is sensitive to the Intrinsic Pathway (XII, XI, IX, VIII) and the Common Pathway .
Factor VII is unique because it is the only factor that is part of the Extrinsic Pathway but not the Intrinsic Pathway. Therefore, a deficiency only affects the PT , leaving the aPTT normal. Deficiencies in Factors VIII, IX, and XI would all prolong the aPTT.
31 / 60
Category:
ASCP Exam Questions
Which condition typically prolongs PT but not aPTT?
PT measures the extrinsic pathway (Factor VII) and common pathway.
aPTT measures the intrinsic pathway (XII, XI, IX, VIII) and common pathway.
Factor VII deficiency only affects the extrinsic pathway, so it prolongs PT but aPTT remains normal .
Other options:
b) Hemophilia A (Factor VIII deficiency) → prolongs aPTT, PT normal.
c) Hemophilia B (Factor IX deficiency) → prolongs aPTT, PT normal.
d) Factor XI deficiency → prolongs aPTT, PT normal.
32 / 60
Category:
ASCP Exam Questions
The Activated Protein C Resistance (APCR) test is most commonly associated with a mutation in:
Activated Protein C Resistance (APCR) is most often caused by the Factor V Leiden mutation .
This mutation makes Factor Va resistant to inactivation by Activated Protein C, leading to a hypercoagulable state.
The APCR test is used to screen for this condition, and genetic testing for Factor V Leiden confirms it.
Other options:
a) Prothrombin — Associated with the prothrombin G20210A mutation, but not directly with APCR.
c) MTHFR — Related to homocysteine metabolism, not APCR.
d) Protein S — Deficiency causes reduced Protein C cofactor activity, but APCR specifically refers to Factor V resistance.
33 / 60
Category:
ASCP Exam Questions
Disseminated Intravascular Coagulation (DIC) is characterized by all of the following laboratory findings EXCEPT:
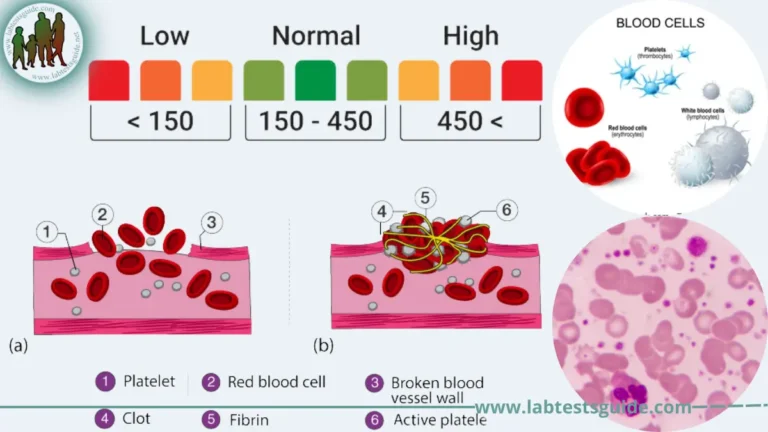
Disseminated Intravascular Coagulation (DIC) is a consumptive coagulopathy where widespread clotting depletes clotting factors and platelets.
Prolonged PT and aPTT: Occurs due to the consumption of multiple coagulation factors.
Decreased platelet count (thrombocytopenia): Occurs due to platelet consumption in microthrombi.
Elevated D-dimer levels: A key finding, indicating the breakdown of fibrin clots (fibrinolysis).
Fibrinogen levels are typically low or decreased , not elevated. While it is an acute-phase reactant, the rapid consumption in DIC usually overwhelms the liver’s ability to produce it, leading to low levels. An elevated fibrinogen would be an unexpected finding in acute DIC.
34 / 60
Category:
ASCP Exam Questions
The Bethesda assay is used to measure:
The Bethesda assay is a specialized test used to quantify Factor VIII inhibitors (alloantibodies or autoantibodies).
It measures the titer of neutralizing antibodies by incubating mixtures of patient plasma with normal plasma and then measuring residual Factor VIII activity.
One Bethesda unit (BU) is defined as the amount of inhibitor that inactivates 50% of Factor VIII in normal plasma after 2 hours of incubation.
Other options:
a) Platelet antibodies → detected by ELISA or flow cytometry.
c) Heparin concentration → measured by anti-Factor Xa assay.
d) Fibrinogen level → measured by Clauss method or PT-derived method.
35 / 60
Category:
ASCP Exam Questions
Which assay is used to detect lupus anticoagulant?
The dilute Russell viper venom test (dRVVT) is one of the primary assays used to detect lupus anticoagulant (LA) , which is an antiphospholipid antibody.
dRVVT uses Russell’s viper venom to directly activate Factor X, bypassing the intrinsic and extrinsic pathways.
The test is phospholipid-dependent ; lupus anticoagulant causes prolongation of the clotting time by binding phospholipids, and this effect is reversed with excess phospholipid (confirmatory step).
Other options:
a) Platelet function test → evaluates platelet disorders, not lupus anticoagulant.
c) PT/INR → used for warfarin monitoring or extrinsic pathway evaluation.
d) Thrombin time → assesses fibrinogen conversion to fibrin; not specific for LA.
37 / 60
Category:
ASCP Exam Questions
Which condition may interfere with PT/INR monitoring due to prolonged baseline clotting?
Lupus anticoagulant (LA) is an antiphospholipid antibody that interferes with phospholipid-dependent coagulation tests in vitro.
It can cause a prolonged baseline PT (depending on the sensitivity of the thromboplastin reagent used), which may complicate INR monitoring in patients on warfarin.
This occurs because LA binds phospholipids in the PT reagent, delaying clot formation and artificially elevating the INR, potentially leading to underdosing if not recognized.
Other options:
b) Hemophilia A → prolongs aPTT, not PT.
c) vWD → typically does not affect PT.
d) Aspirin therapy → affects platelet function but not PT.
38 / 60
Category:
ASCP Exam Questions
Which factor deficiency causes both prolonged PT and aPTT but normal thrombin time?
Factor V is part of the common pathway (along with Factors X, II, and fibrinogen).
A deficiency in Factor V will prolong both PT and aPTT because both pathways converge at the common pathway.
Thrombin time (TT) remains normal because TT directly converts fibrinogen to fibrin and does not depend on Factor V.
Other options:
b) Factor VIII → Only prolongs aPTT, PT is normal.
c) Factor XII → Only prolongs aPTT, PT is normal.
d) Factor VII → Only prolongs PT, aPTT is normal.
40 / 60
Category:
ASCP Exam Questions
The test of choice for monitoring low molecular weight heparin (LMWH) therapy is:
Low molecular weight heparin (LMWH) works mainly by inhibiting Factor Xa .
The anti-Factor Xa assay directly measures the anticoagulant effect of LMWH by quantifying its inhibition of Factor Xa.
Routine tests like aPTT , PT , and TT are not sensitive to the therapeutic range of LMWH and do not reliably reflect its activity.
Thus, for monitoring LMWH therapy (especially in special situations like renal impairment, obesity, or pregnancy), the anti-Factor Xa assay is the test of choice.
41 / 60
Category:
ASCP Exam Questions
Which of the following tests would be most sensitive to the presence of unfractionated heparin?
Unfractionated Heparin (UFH) enhances the activity of antithrombin III , which inhibits factors IIa (thrombin) and Xa , among others.
The aPTT measures the activity of the intrinsic and common pathways of coagulation, which are directly affected by heparin.
Therefore, aPTT is most sensitive to the presence and effect of unfractionated heparin and is routinely used to monitor UFH therapy .
Other options: PT (Prothrombin Time): Measures the extrinsic pathway — more sensitive to warfarin , not heparin.
TT (Thrombin Time): Can also be prolonged by heparin, but it’s too sensitive for monitoring purposes and not typically used for dose adjustment.
Bleeding Time: Assesses platelet function , not coagulation factors — unaffected by heparin.
42 / 60
Category:
ASCP Exam Questions
A falsely prolonged PT and aPTT in a patient with no bleeding symptoms could be caused by:
Coagulation tests require proper blood-to-anticoagulant ratio in citrate tubes (usually 9:1).
In polycythemia or high hematocrit (>55%), the plasma volume is reduced, so the same volume of citrate can over-anticoagulate the sample, leading to falsely prolonged PT and aPTT.
This is a preanalytical error — the patient has no true bleeding disorder.
Other options:
a) Hemophilia A → prolongs aPTT, but PT is normal; patient would have bleeding symptoms.
c) Liver failure → prolongs PT and possibly aPTT, but patient would likely have bleeding tendency.
d) DIC → prolongs PT, aPTT, but patient is acutely ill with bleeding/thrombosis.
43 / 60
Category:
ASCP Exam Questions
Which laboratory abnormality is most consistent with vitamin K deficiency?
Vitamin K deficiency impairs the synthesis of functional vitamin K-dependent factors (II, VII, IX, X).
Factor VII has the shortest half-life (~4–6 hours), so its levels drop first, causing prolonged PT .
As deficiency progresses, reductions in Factors II, IX, and X lead to prolonged aPTT as well.
Low Factor VII activity is an early and sensitive indicator.
Thrombin time (TT) and reptilase time remain normal, as fibrinogen and the final common pathway are unaffected.
Other options are inconsistent with vitamin K deficiency:
b) Normal PT would not occur, as PT is the most sensitive test.
c) Thrombin time is unaffected.
d) Reptilase time is unrelated to vitamin K factors.
44 / 60
Category:
ASCP Exam Questions
The anti-Xa assay is commonly used to monitor therapy with:
The anti-Factor Xa (anti-Xa) assay measures the ability of heparin (both unfractionated heparin [UFH] and low-molecular-weight heparin [LMWH] ) to inhibit Factor Xa.
It is considered a more accurate and direct method for monitoring heparin therapy, especially for:
LMWH (where aPTT is not sensitive)
UFH in certain clinical situations (e.g., pregnancy, high doses, or when aPTT is unreliable)
Other options:
a) Warfarin → monitored by PT/INR.
c) Aspirin → monitored by platelet function tests (not anti-Xa).
d) Vitamin K → not monitored by coagulation assays; it is a treatment, not an anticoagulant.
45 / 60
Category:
ASCP Exam Questions
A patient with a family history of thrombosis is found to have decreased levels of free Protein S antigen. This is most consistent with:
Protein S acts as a cofactor for activated Protein C in the inactivation of Factors Va and VIIIa.
A decreased level of free Protein S antigen is the laboratory finding that directly confirms Protein S deficiency , which is a known inherited thrombophilia.
This matches the patient’s family history of thrombosis.
Other options:
a) Factor V Leiden → causes activated Protein C resistance, but Protein S levels are normal.
c) Antithrombin III deficiency → causes low antithrombin levels, not Protein S.
d) Prothrombin G20210A → increases prothrombin levels, Protein S is normal.
46 / 60
Category:
ASCP Exam Questions
A patient with a prolonged aPTT has a normal PT. A mixing study with normal plasma corrects the aPTT. This indicates:
Low molecular weight heparin (LMWH) works mainly by inhibiting Factor Xa (and to a lesser extent, thrombin).
The aPTT is relatively insensitive to LMWH and is not used for routine monitoring.
The anti-Factor Xa assay measures the ability of LMWH to inhibit Factor Xa and is the recommended test when monitoring is needed (e.g., in obesity, renal impairment, pregnancy, or pediatric use).
PT and TT are not used for LMWH monitoring.
47 / 60
Category:
ASCP Exam Questions
A prolonged thrombin time with normal reptilase time suggests:
Thrombin time (TT) is sensitive to heparin , direct thrombin inhibitors, low fibrinogen, and fibrinogen abnormalities.
Reptilase time is unaffected by heparin because reptilase (from snake venom) is not inhibited by antithrombin or heparin.
Therefore, if the TT is prolonged but the reptilase time is normal , it strongly suggests the presence of heparin (or another thrombin-specific inhibitor).
Other options:
b) Dysfibrinogenemia → would prolong both TT and reptilase time.
c) Factor VII deficiency → affects PT only; TT and reptilase time are normal.
d) Vitamin K deficiency → prolongs PT (and possibly aPTT), but TT and reptilase time are normal.
48 / 60
Category:
ASCP Exam Questions
The primary role of Protein C and Protein S in the coagulation system is to:
Protein C (activated by thrombin bound to thrombomodulin) and its cofactor Protein S function as key natural anticoagulants .
They work together to proteolytically inactivate Factors Va and VIIIa , which are critical cofactors in the coagulation cascade.
This action downregulates thrombin generation and limits clot formation.
Other options:
a) Incorrect — They inactivate, not activate, FV and FVIII.
b) Incorrect — Protein S is a cofactor for activated Protein C, not for thrombin.
d) Incorrect — They do not promote platelet aggregation; they inhibit coagulation.
49 / 60
Category:
ASCP Exam Questions
The reptilase time is used to differentiate heparin effect from other causes of a prolonged thrombin time because reptilase:
Reptilase (from snake venom) clots fibrinogen by directly converting it to fibrin, similar to thrombin.
However, unlike thrombin, reptilase is not inhibited by heparin or antithrombin.
Therefore, if the thrombin time is prolonged but the reptilase time is normal , the cause is likely heparin (or another thrombin-specific inhibitor).
If both are prolonged, the problem may be low fibrinogen, abnormal fibrinogen, or inhibitors acting on fibrin formation/common pathway
50 / 60
Category:
ASCP Exam Questions
Which of the following coagulation factors is Vitamin K dependent?
Vitamin K is essential for the gamma-carboxylation of specific clotting factors , which allows them to bind calcium and function properly.
The vitamin K-dependent factors are:
Factor II (Prothrombin)
Factor VII
Factor IX
Factor X
Proteins C and S
51 / 60
Category:
ASCP Exam Questions
Which test evaluates fibrinolysis by measuring plasminogen activity?
The Euglobulin Clot Lysis Time (ECLT) evaluates the fibrinolytic system by measuring the time it takes for a clot to dissolve in the euglulin fraction of plasma.
This fraction contains plasminogen , plasminogen activators (like t-PA), and fibrinogen , but is largely free of fibrinolysis inhibitors.
A shortened lysis time indicates increased fibrinolytic activity , while a prolonged time suggests reduced plasminogen activation or hypofibrinolysis.
Other options:
a) Thrombin time → assesses fibrin formation, not fibrinolysis.
c) Mixing study → distinguishes factor deficiencies from inhibitors.
d) dRVVT → detects lupus anticoagulant.
52 / 60
Category:
ASCP Exam Questions
The principle of the clot-based PT test involves the addition of which reagent to citrated plasma?
The Prothrombin Time (PT) test measures the extrinsic and common coagulation pathways.
The test is performed by adding tissue factor (thromboplastin) and calcium to citrated plasma, which recalcifies the plasma and activates the extrinsic pathway via Factor VII.
The time to form a fibrin clot is then measured.
Other options:
a) Kaolin and phospholipid → used in aPTT (intrinsic pathway activation).
c) Thrombin and calcium → used in Thrombin Time (TT).
d) Russell’s viper venom and calcium → used in some specific assays (e.g., dilute Russell’s viper venom time, dRVVT) for lupus anticoagulant testing.
53 / 60
Category:
ASCP Exam Questions
Which of the following conditions is associated with a prolonged bleeding time but normal platelet count?
Bleeding time measures primary hemostasis (platelet plug formation), which depends on platelet function and von Willebrand factor (vWF).
In vWD , there is a defect in vWF, leading to impaired platelet adhesion and prolonged bleeding time, but the platelet count is typically normal .
Other options:
a) ITP — Low platelet count causes prolonged bleeding time, not normal platelet count.
c) Hemophilia A — Bleeding time is normal; problem is secondary hemostasis (coagulation cascade).
d) Vitamin K deficiency — Affects coagulation factors, not platelet function; bleeding time is normal.
54 / 60
Category:
ASCP Exam Questions
Factor VIII assays are typically performed using:
Factor VIII activity is most commonly measured using an aPTT-based clotting assay .
The test is performed by mixing patient plasma with Factor VIII-deficient plasma and performing an aPTT test.
The degree of correction in clotting time compared to a standard curve determines the Factor VIII activity level.
Other options:
a) PT method → Used for Factors VII, X, V, II — not Factor VIII.
c) Platelet aggregation test → Assesses platelet function, not coagulation factor levels.
d) Chromogenic anti-Xa assay → Used for heparin monitoring or some factor assays (like Factor VIII via chromogenic method), but the most typical routine method is aPTT-based.
57 / 60
Category:
ASCP Exam Questions
Heparin therapy is best monitored using:
Unfractionated heparin (UFH) therapy is most commonly monitored using the activated partial thromboplastin time (aPTT) .
Heparin potentiates the action of antithrombin, primarily inhibiting thrombin and Factor Xa, which prolongs the aPTT.
The therapeutic range for UFH is typically 1.5–2.5 times the normal aPTT value.
Other options:
a) PT/INR → Used for warfarin monitoring, not heparin.
c) D-dimer → Measures fibrin degradation, not heparin effect.
d) Platelet count → Monitored during heparin therapy to detect heparin-induced thrombocytopenia (HIT), but does not measure anticoagulant effect.
58 / 60
Category:
ASCP Exam Questions
Which coagulation factor is most sensitive to vitamin K deficiency?
Factor VII has the shortest half-life (approximately 4–6 hours) among the vitamin K-dependent coagulation factors (II, VII, IX, X).
In vitamin K deficiency (or with warfarin therapy), Factor VII levels drop first and most rapidly , making the PT (Prothrombin Time) the earliest and most sensitive screening test for this condition.
Other vitamin K-dependent factors:
Factor IX → half-life ~24 hours
Factor X → half-life ~40 hours
Factor II (prothrombin) → half-life ~60–72 hours
60 / 60
Category:
ASCP Exam Questions
The thrombin time (TT) evaluates:
The thrombin time (TT) measures the time for fibrin clot formation after adding exogenous thrombin to plasma.
It directly evaluates the final common step of the coagulation cascade: the conversion of fibrinogen to fibrin .
Prolonged TT can be caused by:
Heparin (or direct thrombin inhibitors)
Hypofibrinogenemia or dysfibrinogenemia
Elevated fibrin degradation products (FDPs)
Other options:
a) Conversion of prothrombin to thrombin → measured by PT and aPTT.
c) Platelet aggregation → assessed by platelet function assays.
d) Factor XIII activity → assessed by clot solubility tests.
Your score is
The average score is 52%
Follow us on Sicial Media:
Restart quiz
Top 8 Medical Laboratory Scientist (MLS) Exams: Top 8 Medical Laboratory Scientist (MLS) Exams that are recognized globally and can help professionals validate their credentials and enhance their career opportunities:
1. ASCP – American Society for Clinical Pathology (USA) Exam Name: MLS(ASCP)Eligibility: Bachelor’s degree with clinical laboratory experience.Global Recognition: HighPurpose: Certifies Medical Laboratory Scientists in the United States and internationally.2. AMT – American Medical Technologists (USA) Exam Name: MLT(AMT) or MT(AMT)Eligibility: Academic and/or work experience in medical laboratory technology.Global Recognition: ModeratePurpose: Credentialing for medical technologists and technicians.3. AIMS – Australian Institute of Medical and Clinical Scientists Exam Name: AIMS Certification ExamEligibility: Assessment of qualifications and work experience.Recognition: Required for practice in Australia.Purpose: Certification and registration in Australia.4. CSMLS – Canadian Society for Medical Laboratory Science Exam Name: CSMLS General or Subject-specific ExamsEligibility: Graduation from a CSMLS-accredited program or equivalent.Recognition: CanadaPurpose: Entry-to-practice certification in Canada.5. IBMS – Institute of Biomedical Science (UK) Exam Name: Registration and Specialist Portfolio AssessmentEligibility: Accredited degree and lab experience.Recognition: UK and some Commonwealth countries.Purpose: Biomedical Scientist registration with the HCPC (UK).6. HAAD / DOH – Department of Health, Abu Dhabi (UAE) Exam Name: DOH/HAAD License ExamEligibility: Degree in medical laboratory science and experience.Recognition: UAE (Abu Dhabi)Purpose: Licensure for medical laboratory practice in Abu Dhabi.7. DHA – Dubai Health Authority (UAE) Exam Name: DHA License Exam for Medical Laboratory TechnologistsEligibility: Relevant degree and experience.Recognition: Dubai, UAEPurpose: Professional license for clinical laboratory practice in Dubai.8. MOH – Ministry of Health (Gulf Countries like UAE, Saudi Arabia, Kuwait) Exam Name: MOH License ExamEligibility: BSc/Diploma in Medical Laboratory + experience.Recognition: Varies by country.Purpose: Required for practicing in public and private sector labs.Tags:
Possible References Used